
Is COVID-19 the New Atherosclerosis? Acute Aortic Dissection Type A in the Early Period after COVID -19 Infection
*Corresponding Author(s):
Stavros VergopoulosThird Department Of Cardiology, Ippokratio General Hospital, Aristotle University Of Thessaloniki, Greece Str. 49 54642 Thessaloniki, Greece
Tel:+30 6975572188,
Email:stavverg@gmail.com
Abstract
The novel corona virus pandemic has since spread rapidly throughout the world resulting in more than 400 million cases. The clinical manifestations and complications associated with COVID-19 is yet to be elucidated. The clinical presentation may be variable, as it has been previously described. In the published literature many cases of acute aortic dissection caused by COVID-19 infection have been described, but only one in the early period after the resolution of the infection. We present a39year-oldwoman, who was admitted to our department complaining of chest pain after the yoga session. Her past medical history was notable for COVID-19 infection two weeks ago. Her electrocardiogram showed sinus rhythm and mild ST segment elevation in lead a VR, while the transthoracic echocardiogram revealed a dilation of the ascending aorta. After the echocardiographic examination, contrast enhanced computed tomography of aorta was conducted, which revealed an acute aortic dissection (type A- Stanford classification). The patient was admitted for emergent cardiovascular surgery, that was successful and eventually was discharged at the ninth post-operative day.
Introduction
The novel coronavirus pandemic (coronavirus disease 2019 or COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 emerged in December 2019 and has since spread rapidly throughout the world resulting in more than 400 million cases. The full spectrum of the clinical manifestations and complications associated with COVID-19 is yet to be elucidated. The initial clinical presentation includes symptoms and clinical signs of respiratory infection, such as fever, dry cough and fatigue, whereas other commonly reported symptoms include headache, sore throat, neurological symptoms, gastrointestinal manifestations, and anosmia [1-3]. Since then, the clinical presentation may be variable, complicating multiple organs and systems, as it has been described in the literature.
The new SARS-CoV-2 has linked to many cardiovascular manifestations such as aortitis, myocarditis, acute coronary syndrome and pericarditis [4-7]. Acute Aortic Dissection (AAD) is a life-threatening condition with critical clinical presentation and extremely low survival rate even after surgical or endovascular treatment. It suggests of separation of intima from media layer of aorta, while risk factors for aortic dissection consist of trauma, genetic abnormalities, vascular inflammation (giant cell arteritis, Takayasu arteritis), connective tissue disorders (such as Marfan syndrome and Ehlers-Danlos syndrome), lifestyle factors (dyslipidemia, cocaine use, smoking, hypertension) and cardiac valve abnormalities (bicuspid aortic valve) [4]. Transthoracic and transesophageal echocardiography, widely used in the Emergency Department (ED), can contribute to the rapid diagnostic approach of AAD. However, Chest Computed Tomography Angiography (CCTA)is an indispensable imaging method for the conclusive diagnosis of AAD, with 100 % sensitivity and 98 % specificity [8].In the published literature many cases of AAD caused by COVID-19 infection have been described [5], but only one in the early period after the resolution of the infection[5].
Case Presentation
A 39 year-old woman presented to the ED of our hospital complaining only for chest pain radiating to her back. The pain was initiated while she was attending yoga session and was constant but mild and relieved with intravenous paracetamol. Her past medical history was notable for a COVID-19 infection (omicron variant) two weeks ago, with mild symptoms and she was recovered at home and two normal pregnancies with normal delivery. Furthermore, she was no vaccinated for COVID-19.Her clinical examination was normal. Auscultation of heart and lungs did not reveal any pathological findings. Her blood pressure was within normal limits in both arms (left arm 123/65 mmHg, right arm 122/66 mmHg) and ankle-brachial index was 1,15 in both sides. Her peripheral pulses were palpable (in femoral and radial arteries). Blood examination of the patient revealed elevated d-dimers 4,926 μg/dL (normal value: 0-500μg/dL), lactate dehydrogenase305 U/L (normal value: 100-248U/L), creatine phosphokinase281 U/L (normal value: <145U/L) and white blood cell count 14.400 μL (neutrophils 87,4%, lymphocytes 7,6%, monocytes 4,6%) (3.800-10.500), while the rest of blood tests were within normal limits. Her electrocardiogram revealed sinus rhythm with a rate of 72 beats per minute, inverted T waves in leads I, aVL, V2-V6, left posterior fascicular block and mild ST segment elevation in lead a VR (Figure 1). The transthoracic echocardiogram revealed a dilation of the ascending aorta at 5,1cm and mild pericardial effusion around the right ventricle, while the rest of the examination was normal (Figure 2). Patient’s previous electrocardiogram and echocardiogram assessment were normal (she reports a cardiological examination the previous year for preventive reasons). After echocardiographic examination, the patients was submitted to contrast enhanced computed tomography of aorta, which showed an AAD(type A- Stanford classification) which was extending from the ascending aorta to anonymous artery (Figure3) and the patient was transferred to cardiac surgery unit for emergency cardiovascular surgery. The surgery was successful and the patient was discharged at the ninth post-operative day.
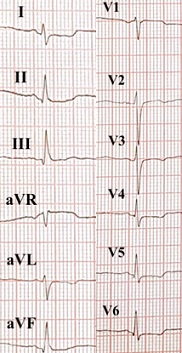 Figure 1: Electrogradiogram of the patient showing sinus rhythm with a rate of 72 beats per minute, inverted T waves in leads I, aVL, V2-V6, left posterior fascicular block and mild ST elevation in lead aVR.
Figure 1: Electrogradiogram of the patient showing sinus rhythm with a rate of 72 beats per minute, inverted T waves in leads I, aVL, V2-V6, left posterior fascicular block and mild ST elevation in lead aVR.
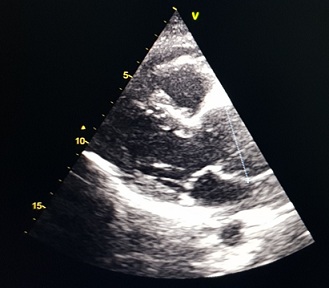 Figure 2: Echocardiogram of the patient showing dilation of the ascending aorta at 5,1cm and mild pericardial effusion (red arrow) around the right ventricle.
Figure 2: Echocardiogram of the patient showing dilation of the ascending aorta at 5,1cm and mild pericardial effusion (red arrow) around the right ventricle.
 Figure 3: Contrast enhanced computed tomography of the patient showing aortic dissection type A (black arrow) extended from the ascending aorta to anonymous artery.
Figure 3: Contrast enhanced computed tomography of the patient showing aortic dissection type A (black arrow) extended from the ascending aorta to anonymous artery.
Discussion
As far as we know this is the second case report type AAAD in a patient in the early period after COVID-19 infection and the first in woman patient [5]. Pathophysiology of aortic dissection is based on inflammation of the endothelium, atherosclerosis, genetic factors and connective tissue disorders [4]. Inflammation of the endothelium and development of aortitis is a well-established condition in COVID-19 infection. Three receptors which SARS-CoV-2 utilizes to enter endothelium are may be responsible for dissection of the intima layer of aorta. These receptors are angiotensin-converting enzyme 2 (ACE2) receptor, transmembrane serine protein 2(TMPRSS2) and matrix metalloproteinase inducer (CD147) [9,10]. Furthermore, SARS-CoV-2 through hypersensitivity type 3 induces proinflammatory cytokines (such as inteleukin-1, inteleukin-6 and Tumor Necrosis Factor-a) and the complement (mainly C3 activation). The inflammation pathways which are mediated from the above elements are strongly associated with the development of aortic dissection4. Much more further investigation is needed in order to establish a pathophysiologic pathway by which COVID-19 infection leads to dissection of intima layer of arteries. Clinicians nowadays must be aware and alarmed of cardiovascular complications caused by COVID-19 infection.
References
- Yang X, Yu Y, Xu J, Shu H, Xia J, et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. The Lancet Respiratory Medicine 8: 475-481.
- Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-O, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine 382: 1708-1720.
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382: 727-733.
- Nienaber CA, Clough RE, Sakalihasan N, Suzuki T, Gibbs R, et al. (2016) Aortic dissection. Nat Rev Dis Primers 2: 1-18.
- Engin M, Ayd?n U, Eskici H, Ata Y, Türk T (2021) Type 1 Acute Aortic Dissection in the Early Period After COVID-19 Infection. Cureus 13: 13751.
- Montero-Cabezas J, Córdoba-Soriano J, Díez-Delhoyo F, Abellán-Huerta J, Girgis H, et al. (2022) Angiographic and clinical profile of patients with COVID-19 referred for coronary angiography during SARS-CoV-2 outbreak: results from a collaborative, european, multicenter registry. Angiology 73: 112-119.
- Tschöpe C, Ammirati E, Bozkurt B, Caforio ALP, Cooper LT, et al. (2021) Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nature Reviews Cardiology 18: 169-193.
- Bossone E, LaBounty TM and Eagle KA (2018) Acute aortic syndromes: diagnosis and management, an update. Eur Heart J 39: 739-749.
- Karapanagiotidis GT, Antonitsis P, Charokopos N, Foroulis CN, Anastasiadis K, et al. (2009) Serum levels of matrix metalloproteinases-1,-2,-3 and-9 in thoracic aortic diseases and acute myocardial ischemia. J Cardiothorac Surg 4: 1-6.
- Jung F, Krüger-Genge A, Franke R-P, Hufert F, Küpper J-H, et al. (2020) COVID-19 and the endothelium. Clin Hemorheol Microcirc 75: 7-11.
Citation: Vergopoulos S, Evangeliou AP, Boulmpou A, Sidiropoulou MS, Giannopoulos G, et al. (2022) Is COVID-19 the New Atherosclerosis? Acute Aortic Dissection Type A in the Early Period after COVID -19 Infection. J Angiol Vasc Surg 7: 085.
Copyright: © 2022 Stavros Vergopoulos, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

