Living with a vestibular disorder during the Covid-19 pandemic: An online survey study
Abstract
BACKGROUND:
People with vestibular disorders experience symptoms which put them at risk of reduced wellbeing during the Covid-19 pandemic.
OBJECTIVE:
To assess the impact of the Covid-19 pandemic on vestibular symptoms, access to healthcare and daily activities amongst people living with a vestibular disorder.
METHODS:
An online survey was completed by 124 people in the UK with a vestibular disorder. The survey incorporated the Vertigo Symptom Scale-Short Form and questions regarding health status, healthcare received, daily activities and employment during Covid-19.
RESULTS:
The Covid-19 pandemic affected perceptions of wellbeing. 54.1% rated their health as worse now than before the pandemic. Vertigo, unsteadiness, dizziness, tinnitus, loss of concentration/memory, and headaches were the most exacerbated symptoms. Respondents reported changes to their daily activities including reduced social contact (83%) and exercise (54.3%). Some experienced healthcare delays or received a remote appointment. Remote care was perceived as convenient, but barriers included difficulty communicating, trouble concentrating and perceived unsuitability for initial appointments. Unintended benefits of the pandemic included less social pressure, avoiding busy environments, and engaging in self-care.
CONCLUSION:
The effects of the Covid-19 pandemic are diverse. Clinical services should be mindful that Covid-19 can exacerbate vestibular and allied neuropsychiatric symptoms that require acute, multi-disciplinary intervention, but not lose sight of the potential benefit and cost saving associated with promoting self-management and delivering remote care, especially post-diagnosis.
The direct and indirect effects of the Covid-19 pandemic are pervasive. The coronavirus (SARS-CoV-2) can infect the brain or overstimulate the immune system, compromising brain function and inducing neurological or psychiatric effects [1]. Reducing transmission of Covid-19 required rapid responses which, for many countries, meant introducing social distancing restrictions. While these measures helped slow the spread of infection, they disrupted key aspects of daily life including social interactions, work and education, access to transport, and provision of healthcare services [2]. The health benefits of the pandemic response must therefore be balanced against the negative effects on mental and physical health [3]. Identifying and supporting those most affected by the pandemic has become an international priority [4]. Numerous factors are associated with higher risk of reduced well-being, such as those with existing neurological and mental health conditions [5, 6]. One such at-risk group are people with vestibular disorders.
People with vestibular disorders experience a constellation of dizziness, vertigo and imbalance symptoms [7]. Dizziness and vertigo are prevalent within the general population (∼30% of adults), with an increased prevalence in older adults [8]. This is also the age group most at risk of severe illness from Covid-19 [9]. Vestibular disorders significantly impact an individual’s quality of life leading to adjustments in their daily lifestyle (e.g., dietary restrictions), socialising (e.g., avoid crowded environments) and employment (e.g., difficulty multitasking) [10]; they are also associated with highly morbid symptoms including falls and wandering amongst older adults [11].
Emerging evidence suggests that Covid-19 can induce vestibular problems as a consequence of the infection [12]. Signs of peripheral and central nervous system complications (e.g., encephalopathy, stroke, seizures) and neurological symptoms (e.g., anosmia, headache) have been reported during and after the Covid-19 infection [13] with vertigo, dizziness, tinnitus and hearing loss [2, 14] commonly described. Another important problem is the finding that those with a history of migraine, a disorder commonly accompanied by vestibular symptomology, appear to have a higher likelihood of Covid-19 infection, and subsequently report more frequent symptoms than those without migraine [15, 16]. As yet, the causes and origins of these vestibular problems are unclear; Covid-19 may directly damage the central nervous system and inner ear organs, or trigger systemic immune responses through a viral infection that affects the vestibular system less specifically [17].
Infection aside, the mental distress associated with the pandemic and social distancing restrictions could indirectly worsen vestibular symptoms [2]. ‘Invisible’ psychological symptoms are already experienced by up to 60% of people with vestibular disorders [18]. These include cognitive problems, ‘brain fog’, and mental health disturbances. Somatic complaints including headache and fatigue are also prevalent. A complex bidirectional interaction exists between vestibular symptoms and psychological distress, whereby they can exacerbate each other [19, 20] and limit recovery [21].
To further complicate management, vestibular disorders are difficult for clinicians without neuro-otological expertise to diagnose, meaning patients can wait one or two years before a correct diagnosis and referral is made, during which time disability accrues [22]. Due to the increased pressure the Covid-19 pandemic has placed on healthcare services, it has been more difficult to receive timely healthcare for conditions such as vestibular disorders that are not life-threatening. Some patients may also be hesitant to report symptoms or attend face-to-face appointments [23]. This may, in turn, increase the disruption and economic burden of vestibular disorders.
Where consultations for vestibular disorders are taking place, these are sometimes being conducted remotely over telephone or video calls [24]. People with vestibular disorders can find travelling to and attending hospitals challenging because of symptom induction [25] so remote consulting brings unexpected potential to benefit this group. However, remote consultations are susceptible to degraded sound quality and reduced lip reading which can adversely affect the communication abilities of people who experience hearing loss or tinnitus [26]. Additionally, some parts of the clinical examination such as an MRI or head impulse testing cannot be done remotely [25] which is causing a backlog of appointments with the unfortunate result that some patients’ symptoms have deteriorated in the meantime [23].
In light of the above concerns, there is a consensus that more needs to be understood about how best to care for people with vestibular disorders during and after the Covid-19 pandemic [27]. Little is known about how the pandemic might have affected the experiences of people living with a vestibular disorder [28], although the potential for the pandemic to restrict daily activities (including access to healthcare), and intensify psychological symptoms is believed to be considerable. To this end, the present study administered an online survey to explore the perceived effects of the Covid-19 pandemic on people with vestibular disorders, focusing on changes in vestibular symptoms, healthcare received, and activities of daily living. A rapid online survey methodology, similar to other Covid-19 research was employed. Survey items were based on emerging research literature and articles from vestibular-related charity organisations, supplemented by our own discussions and theorizing.
1Methods
An online survey was iteratively developed with input from researchers, healthcare professionals, and two people living with vestibular disorders. The study received ethical approval from the Psychology Research Ethics Committee at the University of Kent.
1.1Participants
Eligible participants were 18 years or older, living in the UK and self-reported a diagnosed vestibular disorder. Self-reported disorders which could produce dizziness symptoms without a vestibular component (e.g., fainting and light-headedness due to cardiovascular disease) were not considered in this study. Eligibility criteria were presented in the participant information sheet and page one of the survey. All participants provided informed consent prior to data collection. Participant characteristics are presented in Table 1.
Table 1
Participant characteristics
| Characteristic | Sample (N %) |
| Age | |
| Mean (SD) | 48.81 (13.01) |
| Gender | |
| Female | 106 (85.5%) |
| Male | 16 (12.9%) |
| Identify outside these categories | 2 (1.6%) |
| Ethnicity | |
| White | 119 (96%) |
| Asian/Asian British | 2 (1.6%) |
| Mixed/multiple ethnic groups | 1 (0.8%) |
| Other ethnic group | 2 (1.0%) |
| Education level* | |
| General Certificate of Secondary Education (GCSE) | 17 (13.7%) |
| Advanced Level qualifications (A Level) | 27 (21.8%) |
| University degree | 27 (21.8%) |
| Higher degree | 38 (30.6%) |
| Other | 15 (12.1%) |
| Employment (prior to Covid-19) | |
| Full-time | 48 (38.7%) |
| Part-time | 21 (16.9%) |
| Self-employed | 7 (5.6%) |
| Retired | 24 (19.3%) |
| Voluntary full/part-time | 4 (3.2%) |
| Full-time education | 4 (3.2%) |
| Looking for work | 1 (0.8%) |
| Not working and not looking for work | 13 (10.5%) |
| Other | 2 (1.6%) |
| Living situation | |
| Alone | 19 (15.3%) |
| Living with partner | 54 (43.5%) |
| Living with family | 47 (37.9%) |
| Other | 4 (3.2%) |
| Time since diagnosis (years) | |
| Mean (SD) | 7.58 (8.69) |
| Median (interquartile range) | 5.00 (8.00) |
| Vestibular disorder∧ | |
| Benign Paroxysmal Positional Vertigo (BPPV) | 28 (22.6%) |
| Labyrinthitis | 31 (25%) |
| Ménière’s Disease (MD) | 45 (36.3%) |
| Vestibular Migraine (VM) | 43 (41.9%) |
| Vestibular Neuritis/Neuronitis (VN) | 18 (14.5%) |
| Endolymphatic Hydrops | 4 (3.2%) |
| Perilymph Fistula | 1 (0.8%) |
| Other | 27 (21.8%) |
Note. *GCSEs and A Levels are British educational qualifications usually taken by 14 to 16-year-olds and 16 to 19-year-olds respectively. ∧Denotes a multi-answer question, the percentage of respondents who selected each answer option are presented.
1.2Recruitment
Vestibular-related charity organisations such as the Ménière’s Society and the Vestibular Disorders Association were asked to share information about the study including eligibility criteria, overview of survey content, and the weblink to the online survey on their websites and social media channels. Study information and a link for completion were also shared through the social media channels of several support networks for people with vestibular disorders. Special interest groups for Allied Healthcare Professionals were asked to share information about the survey with their membership. A poster advertising the survey was also displayed at a neuro-otology clinic (London Neuro-Otology Centre).
The survey was published using Jisc Online Surveys platform on April 6th 2021, and data collection remained open until July 2nd 2021. We closed the survey ahead of Step 4 of the UK Government’s planned roadmap out of lockdown when legal limits on social contact were originally due to be lifted [29]. No identifiable data were collected.
1.3Survey design
This cross-sectional survey was designed in a semi-structured format comprising multiple-choice questions and free-text fields for elaboration. The survey took approximately 20 minutes to complete and aimed to cover a range of relevant aspects while minimizing participant burden. The full survey questionnaire is available in the Supplementary Materials. The survey covered the following:
• Demographic information
Including age, gender, ethnicity, and education.
• Medical history
Such as diagnosed neurological and mental health conditions. It also captured whether participants have been infected with the coronavirus, when this occurred, and whether this was confirmed by testing.
• Health and vestibular symptoms
Including vestibular diagnosis, time since diagnosis, and the type of healthcare professional who diagnosed this.
Vestibular symptoms were captured using the Vertigo Symptom Scale –Short Form (VSS-SF) [30], which contains fifteen items relating to vestibular-balance and autonomic-anxiety symptoms. Participants rated the frequency of each symptom using a five-point Likert scale ranging from “Never” to “Very often”. To adapt this scale to our context, we asked participants how frequently they had experienced these symptoms at the start of the coronavirus outbreak (early 2020). We also added an additional four items to the scale to capture symptoms thought to be relevant during Covid-19 (tinnitus, hearing loss, cognitive problems, visual disturbances).
To explore whether participants had experienced any changes during Covid-19, participants were then presented with the same nineteen items and three response options “No”, “Yes (Got worse)”, “Yes (Got better)”. Those who had been infected with the coronavirus were asked to focus on changes during the coronavirus infection. Those who had not been infected were asked to focus on changes during the Covid-19 pandemic.
Participants were also asked if they had received the coronavirus vaccine (Y/N) and whether they had experienced any changes in their vestibular symptoms following this (Y/N). An open-ended free-text question was included to allow participants to provide more detail.
Finally, a five-point Likert scale ranging from “Much worse now than before the pandemic” to “Much better now than before the pandemic” was used to quantify changes in general health status.
• Vestibular care during the Covid-19 pandemic
Questions covered what vestibular healthcare activities participants had received since the start of the coronavirus outbreak and from what type of healthcare professional.
Questions also explored views on how the Covid-19 pandemic had affected healthcare and perceptions about attending consultations either remotely or in-person. A five-point Likert scale ranging from “Much worse” to “Much better” was used to quantify the impact remote care would have (relative to face-to-face care) on aspects of care provision.
• Impact of Covid-19 on daily activities
Explored how much daily activities have been affected by Covid-19, what changes people had made to their routine, and what impact this has had on everyday life. Items were informed by The Coronavirus Disability Survey (COV-DIS) (Section on Impact of Covid-19 on daily activities) [31].
• Working during Covid-19
Including employment arrangements prior to Covid-19, participants’ work situations during Covid-19, and what impact the Covid-19 pandemic had on their ability to work. A five-point Likert scale ranging from “Much worse than before” to “Much better than before” was used to quantify the impact of the pandemic on 11 items related to working. The same Likert scale was also used to quantify the impact of the pandemic on 10 items related to work-life balance.
• Support needs
Explored the impact the pandemic has had or will have on finances, any unintended benefits of the lockdown, and what support people would have found helpful during Covid-19.
1.4Analysis
Descriptive statistics were used to examine responses to closed questions. Branching logic was used and thus the number of responses to some items varied. Results are presented as percent of total answers.
A qualitative analysis of the written comments provided to five open-ended questions was performed using thematic analysis [32, 33]. Familiarisation with the dataset began by reading the responses, sections of text were then coded, and a coding framework was developed to describe the contents of the responses (LS). Two authors (LS and MT) separately applied the coding framework to the dataset. Coding disparities were resolved by discussion. Exemplary quotes are provided from individual respondents (R).
2Results
2.1Participant characteristics
Responses were received from 139 participants. Of these, 15 were excluded: 10 were based outside of the UK and 5 did not self-report having a diagnosed vestibular disorder. Thus, 124 surveys were included in the analysis (see Table 1 for sample characteristics and Supplementary Table 1 for recruitment sources).
The most prevalent vestibular disorders were Ménière’s disease (36.3%, n = 45) and vestibular migraine (41.9%, n = 43). Half the sample (51%, n = 43) had a combination of multiple diagnosed vestibular disorders. The average time since diagnosis was 7.58 (±8.69) years with a wide range of < 1 month–48 years. Diagnoses were made by a healthcare professional, usually an Ear Nose Throat (ENT) specialist or neuro-otologist.
50.8% (n = 63) reported having a diagnosed mental health condition, of those 37 (59%) reported having more than one condition. Anxiety (82.5%, n = 52), depression (66.7%, n = 42) and post-traumatic stress disorder (17.5%, n = 11) were the most prevalent conditions. 13 respondents (10.5%) reported having a diagnosed comorbid neurological condition (including stroke, head injury, chronic fatigue syndrome).
2.2Vestibular symptoms during Covid-19
22 respondents (17.7%) self-reported as having been infected with the coronavirus, of these 14 (63.6%) self-reported having their diagnosis confirmed by a Covid test or healthcare professional. 18.9% (n = 20) were unsure if they had been infected.
At the start of the coronavirus outbreak (early 2020), most respondents (78%, n = 97) experienced severe vestibular symptoms using the cut-off score of ≥12 on the VSS-SF [34]. Tinnitus, hearing loss, loss of concentration or memory, and visual disturbances were also frequently experienced (see Supplementary Table 2).
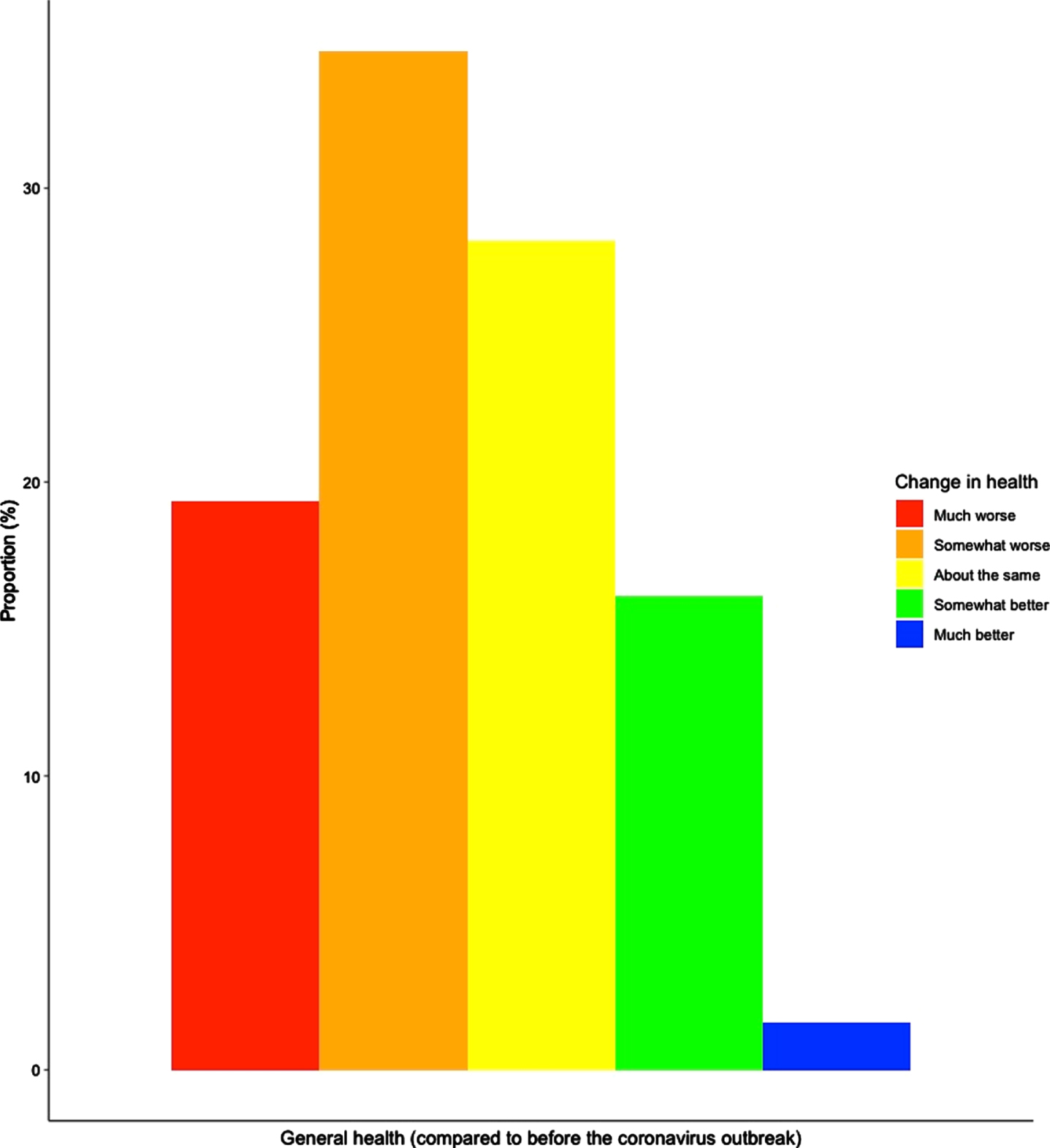
Most respondents noticed some negative change in their vestibular symptoms during their infection (where applicable) or, more generally, during the Covid-19 pandemic. Vestibular-balance symptoms (dizziness, vertigo, and unsteadiness: 37.1 –46%), tinnitus (46.8%, n = 58) and loss of concentration or memory (39.5%, n = 49) were the symptoms most rated as having worsened (see Fig. 1). Most respondents reported autonomic-anxiety symptoms had generally remained stable, except for headaches (46%, n = 57 got worse). In line with this, most respondents viewed their general health as much worse now (19.4%, n = 24), somewhat worse now (34.7%, n = 43) or about the same now as before the pandemic (28.2%, n = 35) (see Fig. 2).
Fig. 1
Percentage of reported changes in vestibular symptoms during the Covid-19 infection or pandemic.
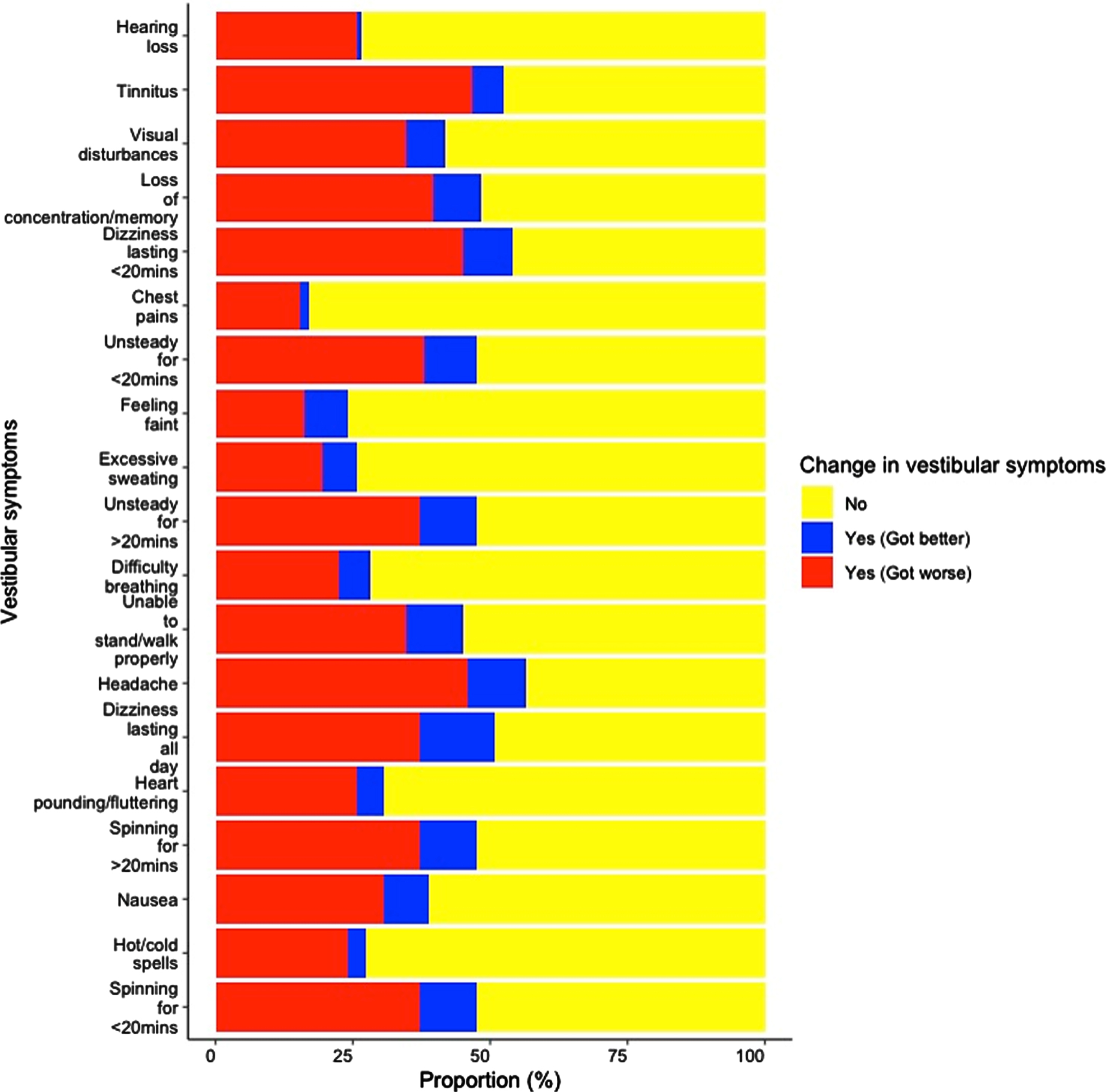
Fig. 2
Compared with before the coronavirus outbreak in January 2020, how would you rate your health in general now?
A Welch’s ANOVA was used to explore changes in general health between those who self-reported having been infected with the coronavirus (n = 22) and those who did not (n = 102), while accounting for the unequal sample sizes of the groups. Those infected with the coronavirus were more likely to report worse general health [F(1,122) 4.44, p < 0.05, ηp2 = 0.04]. Composite scores were also calculated for the vestibular-balance and autonomic-anxiety sub-scales of the VSS-SF (average of the individual symptom scores) and compared between the groups. Those infected with the coronavirus were more likely to report autonomic-anxiety symptoms had gotten worse compared to those who did not have the infection [F(1,122) 8.84, p < 0.05, ηp2 = 0.07]. No other group differences were present (p > 0.17).
91 respondents were asked whether they had received the coronavirus vaccine (item added during data collection). 77 (84.6%) respondents had been vaccinated. Of these, 29 (37.7%) experienced changes in their vestibular symptoms following the vaccine. 29 respondents used the free-text space to describe the changes experienced. Some described existing symptoms worsening following the vaccine [“Headaches became more frequent accompanied with throbbing and dizziness”(R41); “Tinnitus which was mild and occasional prior to the jab is now much more pronounced and more frequent”(R139)], while others felt the vaccine had triggered an attack during a period where they were otherwise well [“Within hours of my first AstraZeneca vaccine I had a bout of vertigo, this did not rectify and lasted 7 weeks. Prior to this my balance problem had not affected me in approximately one year”(R39)].
2.3Vestibular healthcare during Covid-19
Around half of respondents (n = 69, 55.6%) had received clinical care for their vestibular disorder since the start of the coronavirus outbreak (early 2020). Care included vestibular rehabilitation, prescribed medicines, consultation, Epley manoeuvre, hearing test, counselling, and an MRI. Healthcare was delivered by multiple healthcare professionals including GPs, physiotherapists, nurses, neurologists, neuro-otologists, ENT practitioners, and audiologists. For some, their healthcare continued as normal (25%, n = 31). However, for most, the pandemic had altered their healthcare (see Table 2) including participating in remote consultations (27.4%, n = 34) and rescheduling appointments (19.4%, n = 24).
Table 2
Reported changes in vestibular healthcare during the Covid-19 pandemic
| Did the Covid-19 pandemic alter your vestibular care at all? | N |
| No, it continued as normal | 31 (25%) |
| Yes, my appointment was rescheduled | 24 (19.4%) |
| Yes, I was put on an appointment waiting list | 16 (12.9%) |
| Yes, I was offered a remote appointment (over the telephone or a video call) | 34 (27.4%) |
| Yes, my treatment was paused | 14 (11.3%) |
| Yes, my treatment was modified | 3 (2.4%) |
| Yes, I had difficulties obtaining prescriptions or medication for my vestibular Disorder | 11 (8.9%) |
| Not applicable | 21 (16.9%) |
| Other | 13 (10.5%) |
Note. Multi-answer question: Percentage of respondents who selected each answer option.
Respondents were asked to indicate the impact that remote appointments (as compared to face-to-face appointments) would have on their care. Figure 3 shows that most respondents viewed remote care as having the potential to improve travel (23.4% better, 37.9% much better) and convenience (29.8% better, 19.4% much better), and to reduce exposure to illness (26.6% better, 29% much better) and aggravating vestibular symptoms (23.4% better, 18.5% much better). But, they also felt that it could be detrimental to the quality of service (29% worse, 13.7% much worse) and feeling connected to their doctor (40.3% worse, 20.2% much worse).
Fig. 3
As compared to face-to-face care, please rate the impacts you think remote care (over the telephone/video call) would have for.
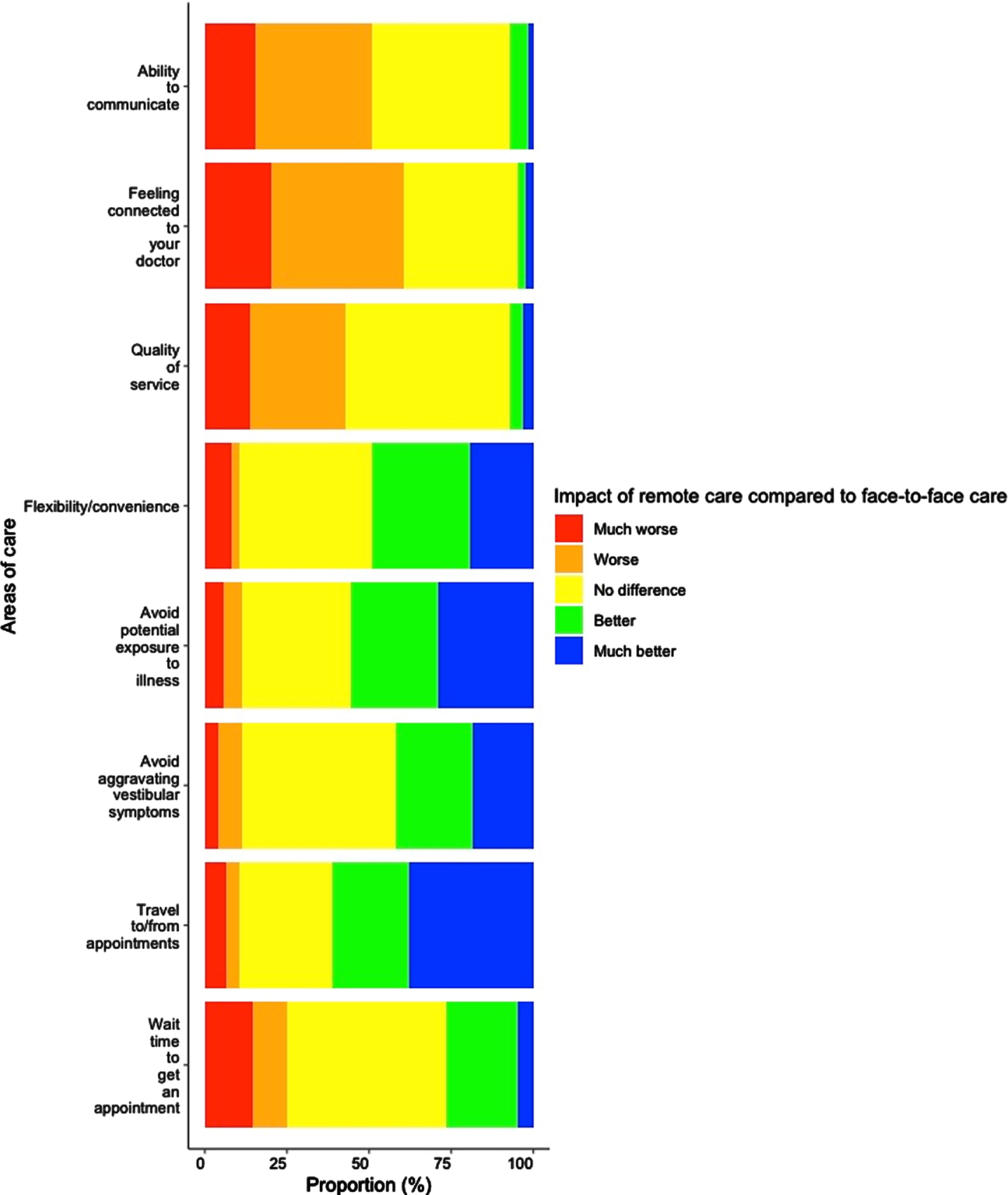
Exploratory analyses examined whether the perceived impact of remote care was related to demographic or clinical factors. Negative correlations were found between age and travel to/from appointment [r(124) = –0.26, p = 0.004], avoiding potential exposure to illness [r(124) = –0.23, p = 0.009], and flexibility/ convenience [r(124) = –0.18, p = 0.004]. Younger participants viewed these aspects of care provision more positively. No other correlations with age were found (all p’s > 0.08). Spearman’s rank correlations also assessed the relationship between composite scores of the VSS-SF (vestibular-balance and autonomic-anxiety) and perceptions of remote care. Vestibular-balance symptoms only correlated with waiting time for appointment [r(124) = –0.25, p = 0.005]. Those with less severe symptoms, viewed the impact of remote care on waiting times more positively. No other correlations with symptom severity were found (all p’s > 0.13). No significant correlations were found between time since diagnosis and the perceived impact of remote care (all p’s > 0.07). Statistical comparisons between vestibular disorders were limited by the unequal sample sizes of the different groups and the multi-morbidities of some participants.
2.4Daily activities during Covid-19
Most respondents felt their daily life had been disrupted by the pandemic, 33.9% (n = 42) by a fair amount, and 36.3% (n = 45) by a lot. Respondents made several changes to their daily routine during the Covid-19 pandemic including shielding, staying home, meeting outdoors, and socialising virtually (see Supplementary Table 3).
Almost half (54.3%, n = 57) reported reduced levels of exercise. Most also reported reduced social interactions with friends and family (83%, n = 87), and activities outside of their home (88%, n = 92). Most respondents who were employed at the time had shifted to working from home (34.5%, n = 30). 44.4% (n = 55) reported having more trouble taking care of day-to-day activities (e.g., grocery shopping, banking, picking up medicines) during the pandemic. Barriers to completing daily activities included: difficulty communicating, feeling unwell, feeling anxious about coping with symptoms in the future, feeling anxious about going out alone, and feeling anxious about being exposed to coronavirus (see Supplementary Table 4).
When asked about how the Covid-19 pandemic had affected their work duties respondents indicated aspects had become more challenging, including: handling stress or anxiety, concentrating and remembering information, energy levels and motivation, communicating, and sensitivity to sound (see Supplementary Table 5). Work-life balance was also affected by the Covid-19 pandemic, particularly: coping with vestibular symptoms, managing other responsibilities (e.g., home schooling, housework), handling fatigue, maintaining relationships, and engaging in leisure activities (see Supplementary Table 5). Some thought the Covid-19 pandemic would negatively impact their finances (33.9%, n = 42), while others thought it would have a positive impact (21%, n = 26) or no impact (33.9%, n = 42).
When asked about what additional support they would have liked to receive during the pandemic, more than half of respondents advocated support to manage their vestibular symptoms (56.5%, n = 70). Support for managing anxiety or low mood (30.6%, n = 38) and loneliness or isolation (19.4%, n = 24) were also requested, as well as support to manage cognitive problems (24.2%, n = 30). Some felt they did not need additional support (29%, n = 26). See Supplementary Table 6. Respondents were asked if there had been any advantage or unintended benefit of the Covid-19 lockdown/restrictions for their situation, 51.6% (n = 64) reported some benefit.
2.5Qualitative analysis
175 written comments were provided. The extent of the data ranged from a few words to paragraphs of text. Eight themes were generated from the analysis of the dataset (see Table 3), these are described below.
Table 3
Themes identified within the qualitative analysis of comments
| Theme | Context |
| Psychological symptoms | Experiencing mood disturbances and cognitive problems and trying to cope with these symptoms. |
| Pressured healthcare services | Increasing demands on overstretched NHS services have made it difficult to access support. |
| Stage of vestibular care | Those in an acute or earlier stage require more support and a face-to-face delivery format. |
| Communication difficulties | Challenge of conveying ‘invisible’ vestibular symptoms can be exacerbated by remote delivery. Particularly, amongst those with hearing loss and tinnitus. |
| Convenience and flexibility | Able to spend more time at home with family and save time/money travelling to attend events in-person. |
| Quieter controlled environments | Having more control over the environment and enjoying quieter spaces. |
| Self-care and management | Engaging in self-care behaviours to manage vestibular symptoms. |
2.5.1Psychological symptoms
Respondents described experiencing cognitive problems during the pandemic, including difficulty concentrating and holding information in mind.
“I struggle with concentrated listening for extended periods of time”(R120, MD)
The cause of these problems was difficult to pinpoint. For some the shift to communicating remotely was cognitively demanding.
“Phone and video calls are uncomfortable and exhausting for my brain fogged confused brain”(R90, superior semi-circular canal dehiscence (SSCD), VM)
Mood disturbances including anxiety and depression were also reported.
“I have really struggled with depression and my regular counselling was just dropped at beginning of pandemic”(R10, BPPV, labyrinthitis, VN)
Several respondents found it difficult to cope with these symptoms and wanted more support.
“I just want some advice about it. As it’s controlling my daily life”(R123, BPPV)
2.5.2Pressured healthcare services
Respondents recognised the pandemic had increased the workload of busy healthcare teams which resulted in delays [“I am now 14 months overdue for my neuro follow-up appointment”(R18, MD, VM)] and poor communication.
“I had 3 appts with 2 different neuro-otologists and all of them lasted no more than 5 minutes. I didn’t feel that I had a chance to speak”(R86, VM, VN)
Models of care provision had changed, with Covid related activities (e.g., supporting acute departments, safety measures) being the focus. This raised issues around which clinical groups should be prioritised.
“People like me have been forgotten about during this time. I am not quite ill enough it seems to be taken notice of for support”(R18 MD, VM)
Some felt let forgotten by their clinical team due to the lack of contact with their service.
“Feeling very let down by my hospital to not only have no contact but also no check-in to see how my Ménière’s is going with lockdown”(R44, MD)
Respondents commented on continuing pressures (including long waiting times for appointments and clinical procedures) as services try to resume in light of backlogs from the pandemic.
“Support for those with chronic conditions has suffered and the fear is that at a primary care level this will never be the same again and may in turn put further pressure on acute services”(R106, endolymphatic hydrops, MD, VM)
2.5.3Stage of vestibular care
Different stages of vestibular care were described including obtaining a diagnosis, establishing a treatment plan, participating in treatment and monitoring outcomes, and implementing self-management strategies. Obtaining a vestibular diagnosis was thought to be critical, since this precedes the other stages. However, this process can be difficult.
“For the stage I am at where I have a diagnosis and the focus is on managing chronic symptoms, the pandemic has been a blessing because I’ve had more control over my lifestyle. However, if I had still been trying to get a diagnosis, I think it would have been very difficult as it was extremely challenging to do this pre-pandemic and the frustration exacerbated symptoms”(R61, labyrinthitis, persistent postural-perceptual dizziness (PPPD), VM, VN)
Respondents thought longer, face-to-face appointments were important to the diagnostic process so that any necessary observations could be completed.
“Would be difficult to initially assess walking and balance capabilities (remotely)”(R12, bilateral vestibular hypofunction (BVH))
Remote care was thought to be better suited for follow-up appointments once a diagnosis and treatment plan were established.
“It depends on purpose of visit - great for check-ins/support/queries but often practitioner needs to observe symptoms (unsteadiness, gait etc) especially early on”(R29, bilateral vestibular failure)
2.5.4Communication difficulties
Respondents thought ‘invisible’ vestibular symptoms could be difficult to explain to a clinician.
“Challenging to convey some of the subjective descriptions of vestibular related symptoms. Doctors can’t see/check balance or how this is effecting my ability to do day-to-day things”(R19, VM)
The shift towards remote delivery could create additional communication barriers. Particularly, amongst those with hearing loss and tinnitus.
“Telephone conversations are very difficult due to hearing loss leading to poor communication, misunderstandings and frustration”(R57, BPPV, endolymphatic hydrops, MD)
The absence of non-verbal cues (body language, social cues, and facial expressions) were highlighted as a potential barrier to remote consulting.
“I respond to social communication which is missing in a telephone appointment” (R88, BPPV, Labyrinthitis)
As well as technology limitations (e.g., interference/poor signal).
“I find it difficult to use the phone, particularly when the other person is on a mobile on speaker, it has an echo that a direct line doesn’t”(R90, SSCD, VM)
Wearing a facemask was also problematic for those with hearing problems.
“Social distancing and mask wearing make communication worse, embarrassing not to understand what is being said”(R57, BPPV, endolymphatic hydrops, MD)
2.5.5Convenience and flexibility
Benefits of remote care were also reported, including saving time:
“As I am unable to drive due to my condition, it is a bonus not to have to spend 3 hours travelling for a 10minute appointment with my consultant”(R88, BPPV, Labyrinthitis)
And money spent travelling to in-person appointments.
“I was able to get in with some of the best doctors sooner and cheaper due to available telehealth due to the pandemic”(R126, perilymph fistula)
More generally, social distancing restrictions afforded more opportunities to spend time at home.
“Quiet of working from home and no commuting has really helped with vestibular symptoms”(R5, labyrinthitis, MD)
This was helpful when vestibular symptoms were active.
“Handy especially if you’re not feeling very well on the day of your appointment”(R112, MD, VM).
2.5.6Quieter controlled environments
Many respondents had shifted to working from home. Being able to control their surrounding environment or workspace was perceived as having health benefits.
“Working from home means I have more control over my environment (heat, light, noise) and a lot less commuting/driving”(R7, labyrinthitis, PPPD, VM)
Respondents also highlighted changes outside their home, whereby local shops, footpaths, and public transport had become less busy. This afforded the opportunity to practice balance and vestibular compensation in a safe environment with fewer obstacles.
“I need to try and walk to improve my balance and it has been great to walk in quieter places with less movement and challenge”(R6, BVH)
2.5.7Self-care and management
Respondents had reflected on their symptoms and implemented coping strategies to manage these during the pandemic.
“I’ve been able to look after myself better and manage my symptoms a lot better”(R37, MD)
Strategies were implemented to manage fatigue, mental wellbeing, and physical health.
“Better able to manage chronic health needs; no exacerbation of symptoms due to commute and busy environments; able to rest for short periods when needed; time and energy for exercise and relaxation”(R61 labyrinthitis, PPPD, VM, VN)
However, others felt their self-management strategies were restricted by the pandemic and that this could cause setbacks.
“Can’t go to gym, sedentary, worsens vertigo”(R131, BPPV, VN).
Self-management was particularly relevant to those in a chronic stage or several years post-diagnosis, who were aware of their symptoms and triggers.
“I have had Ménière’s for 25 years and know how to manage it”(R102, MD)
2.5.8Reduced social pressure
Some respondents reported that the pandemic had reduced feelings of social exclusion as social distancing restrictions meant that others were now staying home more.
“I’ve limited time away from home in fear of embarrassment from an attack. People now know what my life has been like and I didn’t feel so left out”(R48, MD)
This meant they were not missing out on social activities that they might previously have done because of illness.
“Before Covid I was more or less housebound, so lockdown made me feel more normal as no-one was going out and I was therefore not missing out”(R12, BVH)
However, others found staying at home lonely and isolating:
“I seem to have suffered a cognitive decline over the past year… I don’t know if that is from the isolation and restriction from seeing other people and stimulation or just a progression of my medical problems”(R90, SSCD, VM)
3Discussion
This survey provides novel insights into the diverse experiences of people living with vestibular disorders in the UK during the Covid-19 pandemic. Respondents experienced changes in their vestibular symptoms during the Covid-19 infection/pandemic; vertigo, unsteadiness, and dizziness were most frequently rated as having gotten worse. Headache, loss of concentration or memory, and tinnitus were also among the most affected symptoms. Over half of respondents viewed their general health as worse now than before the pandemic. This extends the report by Soylemez and Ertugrul [28] which found that 63% of dizzy patients thought the severity of their ‘dizziness’ had increased during the Covid-19 process. Further, self-ratings of general health and autonomic-anxiety symptoms were worse amongst the 22 respondents who thought they had been infected with Covid-19, compared to those who had not been infected. The changes reported by our sample align with reports of audio-vestibular symptoms in confirmed Covid-19 cases [17], as well as complex interactions between Covid-19 and pre-existing neurological conditions including migraine [16], where there is a higher likelihood of Covid symptomology and reduced wellbeing.
The timing of our survey aligned with the rollout of the UK coronavirus vaccine campaign; 84.6% respondents had been vaccinated. Of these, just over a third experienced changes in their vestibular symptoms following the vaccine. These changes included an exacerbation of existing symptoms (e.g., headaches, fatigue, tinnitus) as well as triggering an attack of vertigo and dizziness during a period when they were otherwise well. Similar findings have been reported in case studies showing sudden unilateral tinnitus following the vaccine [35], and larger cross-sectional survey studies where dizziness symptoms were self-reported to onset following the vaccine [36]. Healthcare professionals should remain vigilant to acute attacks and exacerbations of chronic vestibular symptoms, particularly vertigo, unsteadiness, headaches, tinnitus, and cognitive problems. Increased awareness will help improve surveillance of the coronavirus infection and vaccine and better define possible adverse reactions involving the audio-vestibular system and other indirect responses to living through a pandemic. The nature of our sample suggests this recommendation will be applicable to a range of vestibular disorders, particularly those which are characterised by acute episodes alongside a chronic balance problem (including vestibular migraine, Ménière’s disease and labyrinthitis).
Lifestyle changes imposed by the pandemic could also be a factor in respondents’ perceptions of their health. Reduced physical exercise, social interaction, and leisure activities were commonly reported. This shift towards a more sedentary lifestyle could decrease vestibular compensation in turn increasing perceptions of vestibular symptoms experienced (e.g., visual dominance, feeling unsteady). When less active, fewer compensatory strategies or adaptive behaviours are being practised and thus people with vestibular disorders can feel ‘setback’ or as though their symptoms have worsened. This sedentary lifestyle may be particularly problematic amongst older adults, who are most at risk of severe illness from Covid-19 [37] and developing other conditions including dementia [11, 38]. Encouraging people with vestibular disorders to adopt active, healthy lifestyle choices would therefore seem important. Healthcare providers can signpost and support people with vestibular disorders to access evidence-based resources (e.g., exercise programs, support groups, and information) to promote preventative behaviours.
Anxiety, social isolation, and low mood, also shaped respondents’ experiences during the pandemic. This aligns with previous literature indicating that uncertainty, feeling isolated, and reduced access to mental health support during the pandemic are associated with poorer mental health outcomes within the general population [3]. Prior to the Covid-19 pandemic, psychological symptoms including anxiety, stress, and avoidant behaviours have been associated with reduced vestibular recovery [21, 39]. More recently, Li et al. [27] showed an increase in psychogenic/PPPD diagnoses within a Beijing Neurology clinic during the Covid-19 pandemic relative to the corresponding period in 2019; people’s psychological stress response to the Covid-19 pandemic was thought to underlie this trend. The high prevalence of diagnosed mental health conditions in vestibular cohorts [18, 40], combined with population-wide increased levels of emotional distress during the pandemic [41], means addressing mental wellbeing is particularly relevant in people with vestibular disorders. A third of our respondents thought more support should be available for managing anxiety, low mood, and cognitive problems during the pandemic. To address this, healthcare commissioners could consider the increased provision of psychological support, and clinical teams could pay attention to emotional triggers of dizziness and embed brief targeted questions/assessments addressing psychological symptoms into routine clinical care.
Fortunately, not all experiences of the pandemic were negative. For some respondents, staying at home reduced the usual pressure to socialise in busy environments and made them feel less socially excluded since others were now doing the same. Burton et al. [42] reported a “normalisation” of emotional responses during the pandemic, whereby shared experiences of social isolation led to people with mental health conditions feeling more understood by others. Similarly, in this study while some people with vestibular disorders previously felt socially excluded or held back because of vestibular symptoms, this was reduced during the pandemic. Others also had greater empathy for their situation after staying home themselves.
Engaging in self-care and implementing coping strategies was another unintended benefit of the pandemic. Controlling the surrounding environment (e.g., noise, lighting, temperature), adopting a slower pace, taking time to rest, and practicing balancing techniques in quieter environments were commonly implemented during the pandemic. Our sample thought more support for managing vestibular and psychological symptoms would be valuable. This highlights the importance of self-management training (i.e., help people to help themselves) during the provision of vestibular therapies and fits with the NHS’s long-term plan [43] to deliver clinical care to neurological patients in concert with supported self-management as a means of promoting self-efficacy, perceived sense of control, and willingness to adopt healthy lifestyle practices [44, 45].
Self-management does however require an understanding of the condition itself which means an accurate vestibular diagnosis must be in place for this to be implemented effectively. Unfortunately, it can be difficult for primary care clinicians to elucidate the quality of dizziness a patient is experiencing and decide upon a diagnosis [46]. This finding was echoed by our survey respondents, several of whom underwent a lengthy and stressful process to obtain a diagnosis. Given the importance of establishing an appropriate diagnosis, during the pandemic it may be sensible to limit face-to-face appointments for initial, diagnostic appointments and to reserve remote appointments for post-diagnostic management and continuing an established treatment plan. Our survey results tell us that remote consultations have the potential to offer improved access, increased convenience, and to reduce symptom induction for patients. Healthcare systems and regulators should therefore continue to develop nuanced approaches to remote care and research ways to overcome some of the barriers identified in this study, particularly remote balance assessment, communication difficulties and building rapport.
A strength of our study is the range of topics covered (including symptomology, healthcare, remote consultations, daily activities, and work) and the combination of quantitative and qualitative data, providing novel insights into the challenges and unintended benefits of the pandemic. However, the respondents comprised a UK convenience sample recruited via vestibular charities, peer support networks, social media channels, and a poster displayed at a private neuro-otology clinic. Future studies with more representative samples will therefore be needed to understand the effect of the pandemic on the wider vestibular community. Our findings are based on cross-sectional, self-reported, survey data designed as a rapid response to the pandemic. Future longitudinal studies which incorporate corroborating clinical data (e.g., clinic waiting lists, clinical history, clinical diagnoses, and assessments from multiple clinics) and examine changes over time will help elucidate the impact of Covid-19.
4Conclusion
Given the uncertainty of how long the hardship of Covid-19 may persist, it is important to understand the experiences of people with vestibular disorders and to identify the best ways to support them throughout this period. The current survey indicates that improving care by addressing psychological symptoms, promoting an active lifestyle, supporting self-management, and developing nuanced approaches for remote care may help. The need for additional data on the risk of people with a vestibular disorder contracting Covid-19, as well as on likely audio-vestibular adverse reactions to the infection and vaccine also reman pressing.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/VES-210119.
References
[1] | Varatharaj A. et al., Neurological and neuropsychiatric complications of COVID-19 in 153 patients: A UK-wide surveillance study,}, The Lancet Psychiatry 7: (10), ((2020) ) 875–882. doi: 10.1016/S2215-0366(20)30287-X. |
[2] | Beukes E.W. et al., Changes in Tinnitus Experiences During the COVID-19 Pandemic, Frontiers in Public Health 8 (202), 681. [Online]. Available: https://www.frontiersin.org/article/10.3389/fpubh.2020.592878. |
[3] | Pierce M. et al., Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population,, The Lancet Psychiatry 7: (10), ((2020) ) 883–892. doi: https://doi.org/10.1016/S2215-0366(20)30308-4. |
[4] | World Health Organization, “COVID-19 Strategy Update,” 2020. [Online]. Available: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf. |
[5] | Douglas M. , Katikireddi S.V. , Taulbut M. , McKee M. , McCartney G. Mitigating the wider health effects of covid-19 pandemic response,, Bmj 369: ((2020) ). |
[6] | Holmes E.A. et al., Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science,, The Lancet Psychiatry 7: (6), ((2020) ) 547–560. doi: https://doi.org/10.1016/S2215-0366(20)30168-1. |
[7] | Neuhauser H.K. The epidemiology of dizziness and vertigo,, Handb Clin Neurol 137: , ((2016) ) 67–82. |
[8] | Murdin L. , Schilder A.G.M. Epidemiology of balance symptoms and disorders in the community: A systematic review,, Otol Neurotol 36: (3), ((2015) ) 387–392. |
[9] | Clark A. et al., Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in: A modelling study, Lancet Glob Heal 8: (8), ((2020) ) e1003–e1017. |
[10] | Benecke H. , Agus S. , Goodall G. , Kuessner D. , Strupp M. The burden and impact of vertigo: Findings from the REVERT patient registry,, Front Neurol 4: , ((2013) ) 136. |
[11] | Agrawal Y. , Smith P.F. , Rosenberg P.B. Vestibular impairment, cognitive decline and Alzheimer’s disease: Balancing the evidence,, Aging Ment Health 24: (5), ((2020) ) 705–708. |
[12] | Almufarrij I. , Uus K. , Munro K.J. Does coronavirus affect the audio-vestibular system? A rapid systematic review, Int J Audiol 59: (7) (202), 487–491. doi: 10.1080/14992027.2020.1776406. |
[13] | Nersesjan V. et al., Central and peripheral nervous system complications of COVID-19: A prospective tertiary center cohort with 3-month follow-up, J Neurol (2021), 1–19. doi: 10.1007/s00415-020-10380-x. |
[14] | Saniasiaya J. , Kulasegarah J. Dizziness and COVID-19,, Ear Nose Throat J 100: (1), ((2021) ) 29–30. doi: 10.1177/0145561320959573. |
[15] | Uygun Ö. et al., Headache characteristics in COVID-19 pandemic-a survey study,, J Headache Pain 21: (1), ((2020) ) 121. doi: 10.1186/s10194-020-01188-1. |
[16] | Shapiro R.E. , Gallardo V.J. , Caronna E. , Pozo-Rosich P. The impact of headache disorders on COVID-19 survival: A world population-based analysis, medRxiv (2021), 2021.03.10.21253280. doi: 10.1101/2021.03.10.21253280. |
[17] | Amiri M. , Hasanalifard M. , Delphi M. Impact of COVID-19 on the auditory and vestibular system, Audit Vestib Res (2021). |
[18] | Smith L. , Wilkinson D. , Bodani M. , Bicknell R. , Surenthiran S.S. Short-term memory impairment in vestibular patients can arise independently of psychiatric impairment, fatigue, and sleeplessness,, J Neuropsychol 13: (3),((2019) ) 417–431. |
[19] | Gurvich C. , Maller J.J. , Lithgow B. , Haghgooie S. , Kulkarni J. Vestibular insights into cognition and psychiatry,, Brain Res 1537: , ((2013) ) 244–259. |
[20] | Hanes D.A. , McCollum G. Cognitive-vestibular interactions: A review of patient difficulties and possible mechanisms,, J Vestib Res 16: (3), ((2006) ) 75–91. |
[21] | Cousins S. et al., Predictors of clinical recovery from vestibular neuritis: A prospective study,, Ann Clin Transl Neurol 4: (5), ((2017) ) 340–346. doi: https://doi.org/10.1002/acn3.386. |
[22] | Department of Health (DH), Provision of Adult Balance Services:AGood Practice Guide, 2009. [Online].Available: https://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH093862.. |
[23] | Verghese G. , Hannah C. Lessons learnt from the COVID-19 pandemic Priorities in care for people with neurological conditions after the pandemic, 2021. |
[24] | Vozel D. , Battelino S. Adjustments of audiological, vestibular and otosurgical management during COVID-19 epidemics, 2020. |
[25] | Murdin L. , Harrop-Griffiths K. Dizziness—The Audiovestibular Perspective, in Postural Tachycardia Syndrome, Springer, (2021) , pp. 153–159. |
[26] | Naylor G. , Burke L.A. , Holman J.A. Covid-19 lockdown affects hearing disability and handicap in diverse ways: A rapid online survey study, [Online]. Available:, Ear Hear 41: (6) ((2020) ), [Online]. Available: https://journals.lww.com/ear-hearing/Fulltext/2020/11000/Covid_19_Lockdown_Affects_Hearing_Disability_and.3.aspx. |
[27] | Li C. , Guo D. , Ma X. , Liu S. , Liu M. , Zhou L. The impact of coronavirus disease epidemic on dizziness/vertigo outpatients in a neurological clinic in China,, Front Neurol 12: , ((2021) ) 663173. doi: 10.3389/fneur.2021.663173. |
[28] | Soylemez E. , Ertugrul S. Severity of dizziness increased in dizzy patients during Covid-19 process,, Hear Balanc Commun 19: (2), ((2021) ) 72. doi: 10.1080/21695717.2020.1836579. |
[29] | Gov.UK, COVID-19 Response - Spring 2021 (Summary), 2021. https://www.gov.uk/government/publications/covid-19-response-spring-2021/covid-19-response-spring-2021-summary. |
[30] | Yardley L. , Masson E. , Verschuur C. , Haacke N. , Luxon L. Symptoms, anxiety and handicap in dizzy patients: Development of the Vertigo symptom scale,, J Psychosom Res ((1992) ) 36: (8), 731–741. doi: https://doi.org/10.1016/0022-3999(92)90131-K. |
[31] | Bernard A. et al., Assessing the impact of COVID-19 on persons with disabilities: Development of a novel survey,, Int J Public Health 65: (6), ((2020) ) 755–757. |
[32] | Braun V. , Clarke V. Successful qualitative research: A practical guide for beginners. sage, 2013. |
[33] | Braun V. , Clarke V. , Boulton E. , Davey L. , McEvoy C. The online survey as a qualitative research tool, Int J Soc Res Methodol (2020), 1–14. |
[34] | van Vugt V.A. et al., Internet based vestibular rehabilitation with and without physiotherapy support for adults aged 50 and older with a chronic vestibular syndrome in general practice: Three armed randomised controlled trial,, bmj 367: ((2019) ). |
[35] | Parrino D. , Frosolini A. , Gallo C. , De Siati R.D. , Spinato G. , , de Filippis C. , Tinnitus following COVID-19 vaccination: Report of three cases, Int J Audiol (2021), 1–4. doi: 10.1080/14992027.2021.1931969. |
[36] | Kadali R.A.K. et al., Non-life-threatening adverse effects with COVID-19 mRNA-1273 vaccine: A randomized, cross-sectional study on healthcare workers with detailed self-reported symptoms, J Med Virol (2021). |
[37] | Jordan R.E. , Adab P. , Cheng K.K. Covid-19: Risk factors for severe disease and death, m, BMJ368: , 1198 ((2020) ) . doi: 10.1136/bmj.m1198. |
[38] | Beck D.L. , Bant S. , Clarke N.A. Hearing loss and cognition: A discussion for audiologists and hearing healthcare professionals,, J Otolaryngol ENT Res 12: (3), ((2020) ) 72–78. |
[39] | Tschan R. et al., Patients’ psychological well-being and resilient coping protect from secondary somatoform vertigo and dizziness (SVD) 1 year after vestibular disease,, J Neurol 258: (1), ((2011) ) 104–112. doi: 10.1007/s00415-010-5697-y. |
[40] | Best C. , Eckhardt-Henn A. , Tschan R. , Dieterich M. Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes,, J Neurol 256: (1), ((2009) ) 58–65. |
[41] | Saladino V. , Algeri D. , Auriemma V. The psychological and social impact of Covid-19: New perspectives of well-Being, Frontiers in Psychology 11: , ((2550) ) , [Online]. Available: https://www.frontiersin.org/article/10.3389/fpsyg.2020.577684. |
[42] | Burton A. , McKinlay A. , Aughterson H. , Fancourt D. Impact of the Covid-19 pandemic on the mental health and wellbeing of adults with mental health conditions in the UK: A qualitative interview study, MedRxiv (2021), 2012–2020. |
[43] | NHSEngland, “Supported self-management,” 2020. https://www.england.nhs.uk/personalisedcare/supported-self-management/ (accessed Jul. 13, 2021). |
[44] | Peters M. , Potter C.M. , Kelly L. , Fitzpatrick R. Self-efficacy and health-related quality of life: A cross-sectional study of primary care patients with multi-morbidity,, Health Qual. Life Outcomes 17: (1), ((2019) ) 37. doi: 10.1186/s12955-019-1103-3. |
[45] | Bodenheimer T. , Lorig K. , Holman H. , Grumbach K. Patient self-management of chronic disease in primary care,, JAMA288: (19), ((2002) ) 2469–2475. doi: 10.1001/jama.288.19.2469. |
[46] | Thompson T.L. , Amedee R. Vertigo: A review of common peripheral and central vestibular disorders, {Ochsner J 9: (1) ((2009) ) 20–26[Online]. Available: https://pubmed.ncbi.nlm.nih.gov/21603405. |



