Associations between socioeconomic and public health indicators and the case-fatality rate of COVID-19 in sub-Saharan Africa
Abstract
Aim: To investigate the influence of socioeconomic and public health indicators on the COVID-19 case-fatality rate (CFR) in sub-Saharan African countries.
Methods: Ecological study using publicly available, aggregated COVID-19 data, between February 2020 to May 2021, from 46 sub-Saharan African countries. As the outcome of interest, country-specific CFRs were calculated for five 13-week periods. Spatial and temporal distributions of the variables were analysed, and negative binomial regressions with rate ratios (RR) were conducted to estimate the association between socioeconomic and public health indicators with CFR of COVID-19.
Results: There were 1.7 million confirmed COVID-19 cases and 29,685 deaths in the 46 sub-Saharan African countries during the investigated time period. The median CFR was between 1% and 2%. A higher human development index (RR = 0.80; 95%CI: 0.63-1.02), higher political stability index (RR = 0.94; 95%CI: 0.90-1.00), higher number of hospital beds (RR = 0.84; 95%CI: 0.73-0.97), and higher population density (RR = 0.85; 95%CI: 0.71-1.01) resulted in a lower CFR. Elevated prevalence of diabetes mellitus (RR = 1.56; 95%CI: 0.99-2.45) and cardiovascular disease mortality (RR = 1.51; 95%CI: 1.04-2.20) were associated with higher CFR. Chronic respiratory disease and handwashing facilities presented little to no effects on COVID-19 CFR.
Conclusion: The results draw attention to the vulnerabilities of the sub-Saharan African region which must be considered in the interpretation of our study. Nevertheless, the potential benefits of a lower proportion of pre-existing medical conditions and the young age structure seem to be contrasted by challenges due to socioeconomic and public health factors, which may present possible drivers of CFR on a population level.
Keywords
INTRODUCTION
On the 30th of January 2020, the World Health Organisation (WHO) declared the novel coronavirus (SARS-CoV-2) and the resulting disease COVID-19 a Public Health Emergency of International Concern and emphasised the danger of the health effects. The pandemic has and still is causing exceptional situations, with devastating implications for populations, healthcare systems, and economies globally[1,2]. The virus spreads primarily through aerosols, droplets of saliva, and discharge from the nasopharyngeal area[2]. One of the most important action points to reduce incidence rates is to slow the transmission of the virus and thus prevent infection. A few examples of those preventive actions are practising social distancing, washing and disinfecting one’s hands, covering the mouth and nose, refraining from activities that weaken the lungs (e.g., smoking), and getting vaccinated[3]. About 80% of people who contract COVID-19 recover without needing to be admitted to the hospital, but 15% experience a severe course of the disease and require further medical care such as oxygen therapy. Around 5% of infected people become critically ill and need intensive care. Respiratory failure, sepsis, multiorgan failure, and acute respiratory distress syndrome are examples of complications that may lead to death. People of all ages can contract COVID-19, become critically ill, and die. Nevertheless, findings suggest that people aged 60 years or above and having underlying medical conditions such as hypertension, cardiovascular diseases, diabetes mellitus, obesity, and cancer are at higher risk of developing a severe disease progression[1,4]. By the 23rd of May 2021, the end of the period observed in this work, 167 million confirmed cases and 3.6 million deaths of COVID-19 had been reported worldwide[5]. At present, a new wave of the pandemic is ongoing. By the 5th of December 2021, 263 million confirmed cases and 5.2 million deaths of COVID-19 had been reported worldwide[5].
A study in Italy found that a high human development index (HDI), a summary measure of average achievement in key dimensions of human development (i.e., a long and healthy life, being knowledgeable, and having a decent standard of living), was associated with a high COVID-19 infection and fatality rate[6]. Similar results were found in two other studies comparing countries globally, one of which found a positive association between a high HDI and the incidence rate. Another concluded that countries with a high HDI reported more deaths due to COVID-19 than countries with a lower HDI. Several hypotheses have been put forward, such as whether the contagiousness and transmissibility of the virus overcame intra-country social inequalities and thus reduced the overall effect of socioeconomic factors. It was also speculated that the higher incidence and death rates in high HDI countries might be related to health policies; pandemic response restrictions might have been introduced with delay and viewed with suspicion by the population[7,8]. Khalatbari-Soltani et al.[9] argued that socioeconomic status is associated with contracting the disease, the progression thereof, and mortality. Depending on the workplace, a person may be at increased risk of infection. Stress due to workload has a known association with cardiovascular disease, a risk factor for more severe COVID-19 disease progression. People with lower incomes might live in deprived areas, where population density and overcrowding could impact infection rates[4,9]. Previous research confirms this double link, where it is known that the proportion of people with pre-existing medical conditions is higher in disadvantaged socioeconomic positions[10]. Lack of water, sanitation facilities, and health care resources were also linked to a higher infection rate and severe courses of disease[9-13]. Political stability is another factor that has been found to have an impact on the spread of COVID-19. Vulnerable populations living amid war, conflict, or equivalent conditions were most affected, with political and economic challenges affecting, for example, the management of the pandemic response[14,15]. Sorci et al.[15] reported positive associations between the proportion of population aged ≥ 70 years, as well as the gross domestic product, and the COVID-19 case-fatality rate. A negative association was found with hospital beds per 1000 people[15]. These previous findings point to an interrelation between socioeconomic and public health determinants.
The African continent was rated at high risk for COVID-19 deaths at the onset of the pandemic, strongly based on severe courses of epidemics and disease outbreaks in the past[16-18]. Sub-Saharan Africa consists of 48 countries, many of them facing adverse socioeconomic and other conditions. These circumstances could entail limited opportunities to implement preventive actions (e.g., social isolation) and to reduce barriers to access health care[10,19].
The aforementioned early predictions for the sub-Saharan African region could not be confirmed as the reported COVID-19 cases and deaths were far lower than expected. In a teaching hospital in Zambia, nasopharyngeal swabs were sampled post-mortem from 10% of all deceased patients. They found that 15% of the sample tested positive for the virus, and 73% of these patients had died in their communities, pointing towards a lack of testing. Generalising their data, they concluded that many COVID-19 cases and deaths remained unreported and that widespread transmissions within the communities must occur. Similar to other research, they found that patients presented comorbidities like, tuberculosis (31%), hypertension (27%), and diabetes (13%)[20,21]. Discussions exist as to whether factors such as a young population, experience with epidemics, and a low test rate could have influenced the disease development in sub-Sahara Africa. So far, few studies have been conducted for the region[16,22].
Using publicly available data, this study aimed to investigate the influence of selected socioeconomic and public health indicators on the COVID-19 case-fatality rate (CFR) in sub-Saharan African countries.
METHODS
Data sources
This ecological study used all confirmed COVID-19 cases and deaths reported in 46 of the 48 sub-Saharan African countries from the 24th of February 2020 to the 23rd of May 2021. Tanzania was excluded from the sample because of missing data for more than half of the time under investigation due to the former government that denied the existence of the pandemic. South Africa was omitted from main analyses since it accounts for 48% of the cumulative confirmed cases in sub-Saharan Africa and in our view should be considered separately because of major economic differences compared to other sub-Saharan states. Data on weekly confirmed cases and deaths were obtained from the European Centre for Disease Prevention and Control[23]. These data were total numbers not stratified by age groups or sex. In calendar week nine (i.e., in the week February 24th, 2020 to March 1st, 2020), the first COVID-19 cases in sub-Sahara Africa were recorded, and thus it was chosen as the starting point of this research. Country-level information about socioeconomic, demographic, and public health variables of interest was sourced from
Variables
We calculated the CFR for each of five non-overlapping 13-week time periods per country as given below.
- Time 1: 24.02.2020 [Calendar week (CW): 09/20]-24.05.2020 (CW: 21/20).
- Time 2: 25.05.2020 (CW: 22/20)-23.08.2020 (CW: 34/20).
- Time 3: 24.08.2020 (CW: 35/20)-22.11.2020 (CW: 47/20).
- Time 4: 23.11.2020 (CW: 48/20)-21.02.2021 (CW: 07/21).
- Time 5: 22.02.2021 (CW: 08/21)-23.05.2021 (CW: 20/21).
This allowed us to analyse the data spatially and temporally. We used two different methods for calculation of CFR:
(1) The cumulative number of COVID-19 deaths in the respective time period divided by the cumulative number of COVID-19 cases for the chosen 13-week period.
(2) The cumulative number of COVID-19 deaths in the respective time period divided by the cumulative number of COVID-19 cases with a delay of 14 days between case reporting and possible death to mitigate potential bias[27]. The first method (CFRC) is commonly used, whereas the latter method (CFRL) takes the delay from reporting an infection to death into account which we assumed to be two weeks on average. In this study, we put more emphasis on the latter method.
For the presentation of the CFR on a map we also use the total CFR as obtained by dividing the total number of COVID-19 deaths by the total number COVID-19 cases in the observation period.
As exposures and covariates socioeconomic and public health indicators were chosen based on the aforementioned literature research and data availability for the region and should be considered as umbrella terms for the variables. Most recent data available were used. Socioeconomic indicators were represented by:
- The HDI calculates a value between 0 and 1.0 out of the different aspects of life expectancy at birth, education, and gross domestic product per capita[28].
- Population density indicates how many people of the population live in one square kilometre of the country.
- Political stability and absence of violence/terrorism index which calculates values from -2.5 to +2.5 out of several indicators (e.g., press freedom)[26].
As public health indicators, the following variables were used:
- Cardiovascular disease mortality rate per 100,000.
- Chronic respiratory disease mortality rate per 100,000.
- Diabetes mellitus prevalence in percentage.
- Share of the population with basic handwashing facilities on the premises.
- Hospital beds per 1000 people.
The following demographic variables were used for descriptive purposes and to adjust for potential confounding at country-level:
- Median age of the population or share of the population aged 65 years.
- Share of the female population.
- Population size in millions.
Statistical analyses
Descriptive statistics were calculated to gain an insight into the characteristics of the included countries. To describe the correlation between the covariables, Spearman’s correlation coefficient was calculated.
To analyse the association between the socioeconomic and public health variables with the CFR, a Poisson regression model was fitted. Extra Poisson variation was accounted for using a negative binomial error structure. Observations with 100 or fewer confirmed COVID-19 cases per time period were excluded from the model. The regression analysis was performed both with a univariable and a multivariable model. The model equations were:
log(dij) = log(nij) + α + β + βkxik + γj(univariable model, separately for each covariable k, k = 1, …, K)
and
log(dij) = log(nij) + α + ∑βkxik + γj(multivariable model)
where dijdenote the number of deaths in country i, time interval j, nijdenote the number of cases in country i and time interval j, either with or without a two-week lag, xikdenote the observed covariable k, k = 1, …, K in country i, α, β and γ denote the regression coefficients, where the latter describes a possible time effect. Crude estimates were calculated with the univariable model, and each model was repeated adjusted for demographic variables. The full model was also fitted which included the covariables HDI, population density, political stability index, diabetes mellitus prevalence, cardiovascular diseases and chronic respiratory disease mortality, handwashing facilities, and hospital beds.
In the sensitivity analysis, we excluded observations with case numbers below the calculated median. This was to test whether differences could be detected with respect to the estimates of the main analysis, where all observations with less than 100 cases were excluded. We also checked the robustness by using ranks for those exposure variables which show an extremely high range between minimum and maximum values (i.e., population density, diabetes prevalence, and handwashing facilities). We fitted the models with the ranks and compared the effect with the original analysis[29].
All analyses were performed with SAS software, version 9.4. Copyright © 2016 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA. A significance level of alpha = 0.05 was used to denote statistically significant finding.
RESULTS
Descriptive characteristics
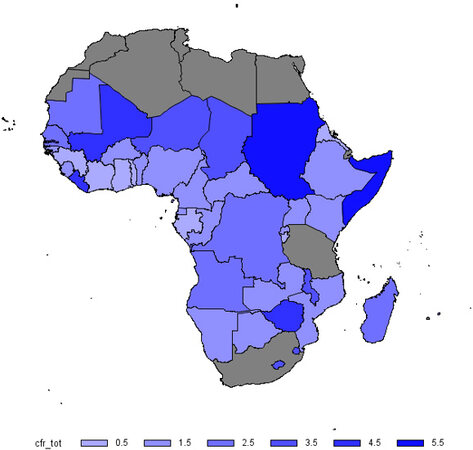
This study included 1.7 million confirmed COVID-19 cases and 29,685 deaths reported in the 46 sub-Saharan African countries between February 24th, 2020 and May 23rd, 2021. On the country level, Ethiopia reported the highest number of cumulative cases (269,194) and deaths (4076), followed by Kenya (cases: 168,432; deaths: 3059). Factoring in the population size, the Seychelles (10,609 cases per 100,000) and Cap Verde (5276 cases per 100,000) presented the highest number of confirmed COVID-19 cases per 100,000 inhabitants. Figure 1 gives a map of Africa which displays the total CFR over the observation period.
Figure 1. Overall crude case-fatality rate (in percent) of COVID-19, sub-Saharan Africa, period February 24th, 2020 to May 23rd, 2021.
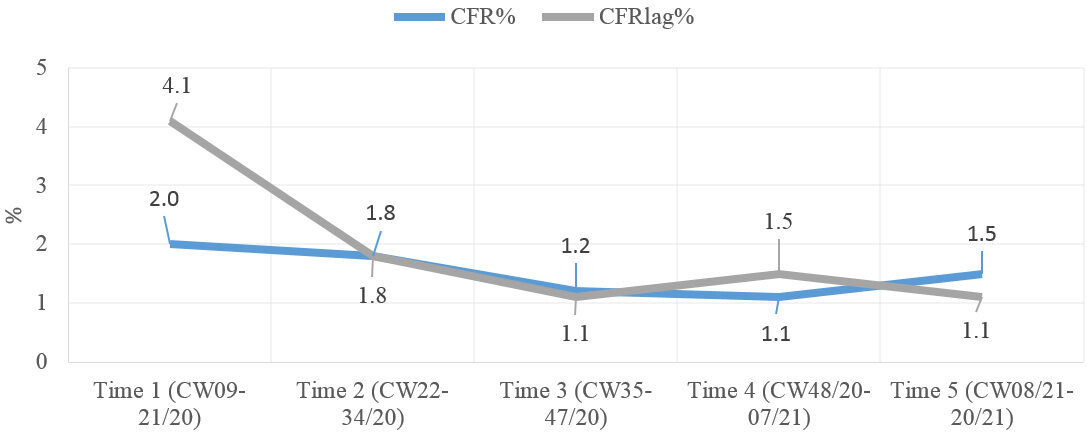
The distributions of the COVID-19 CFRC and CFRL, separated into five time periods, of the 46 countries are summarised in [Table 1]. Of the observations, 9.1% (21 of 230) showed a CFR of 0%, with reported COVID-19 cases but no deaths in the respective countries and time periods. Excluding all observations that presented less than 100 cases per time period (3.0%; 7 of 230) reduced that proportion to 6.1% (14 of 230). Wide ranges indicated higher and lower values as well as outliers.
Overall CFR per time period in n = 46 countries of sub-Saharan Africa
| Mean (SD; 95%CI) | Median (Q1; Q3) | Min | Max | |
| CFRC (%) | ||||
| 24.02.2020-24.05.2020 | 2.6 (± 2.5; 1.9-3.4) | 2.0 (0.6; 4.0) | 0.0 | 9.8 |
| 25.05.2020-23.08.2020 | 1.9 (± 1.5; 1.5-2.4) | 1.8 (0.6; 2.5) | 0.0 | 7.3 |
| 24.08.2020-22.11.2020 | 1.6 (± 1.9;1.0-2.2) | 1.2 (0.6; 2.1) | 0.0 | 12.6 |
| 23.11.2020-21.02.2021 | 1.72 (± 1.5; 1.3-2.2) | 1.1 (0.6; 2.8) | 0.0 | 5.7 |
| 22.02.2021-23.05.2021 | 2.16 (± 2.5; 1.4-2.9) | 1.5 (0.8; 2.3) | 0.0 | 12.3 |
| CFRL (%) | ||||
| 24.02.2020-24.05.2020 | 6.1 (± 11.2; 2.8-9.4) | 4.1 (0.9; 7.1) | 0.0 | 75.0 |
| 25.05.2020-23.08.2020 | 2.0 (± 1.6; 1.6-2.5) | 1.8 (0.9; 2.6) | 0.0 | 6.8 |
| 24.08.2020-22.11.2020 | 1.6 (± 2.5; 0.8-2.4) | 1.1 (0.6; 1.8) | 0.0 | 17.2 |
| 23.11.2020-21.02.2021 | 2.0 (± 2.3; 1.4-2.8) | 1.5 (0.7; 3.0) | 0.0 | 14.1 |
| 22.02.2021-23.05.2021 | 1.7 (± 1.9; 1.2-2.3) | 1.1 (0.8; 2.2) | 0.0 | 11.9 |
The median CFRC and CFRL for the first time period were 2.0% [quantile 1 (Q1): 0.6%; quantile 3 (Q3): 4.0%] and 4.1% (Q1: 0.9%; Q3: 7.1%), respectively. As shown in [Figure 2], from the second time period onwards, the median of both CFRC and CFRL presented no major differences and fluctuated between 1% and 2%. The higher value of CFRL in the first period may be due to underreporting of cases at the beginning of the pandemic.
Figure 2. COVID-19 CFRC and CFRL, sub-Saharan Africa, over time. CFR: Case-fatality rate; CFRC: case-fatality rate with lag of 14 days; CFRL: case-fatality rate without lag of 14 days; CW: calendar week.
Table 2 presents the distributions of the socioeconomic, public health and demographic variables. Most indicators were available for all countries. The variables hospital beds, HDI and population density each had one missing. Seven countries had no data for the variable “handwashing facilities”. Of the considered countries, 91% had a low or medium HDI, resulting in a mean HDI of 0.54 (n = 45; 95%CI: 0.52-0.57) for the overall sample. The share of the female population was almost identical in all countries (median: 50.2%).
Distribution of socioeconomic, public health, and demographic variables, 46 countries of sub-Saharan Africa
| n | Median (Q1; Q3) | Min | Max | |
| Socioeconomic variables | ||||
| HDI | 45 | 0.54 (0.48; 0.58) | 0.39 | 0.80 |
| Population density (per km2) | 45 | 66.1 (23.5; 135.6) | 3.1 | 622.9 |
| Political stability index | 46 | -0.5 (-1.3; -0.1) | -2.6 | 1.0 |
| Public health variables | ||||
| CVD death rate (p. 100,000) | 46 | 271.3 (235.8; 325.7) | 181.0 | 435.7 |
| CRD death rate (p. 100,000) | 46 | 45.7 (37.0; 56.9) | 20.3 | 100.4 |
| Diabetes prevalence (%) | 46 | 3.9 (2.4; 6.1) | 0.9 | 22.0 |
| Handwashing facilities (%) | 39 | 15.9 (7.9; 24.6) | 1.1 | 52.2 |
| Hospital beds (p. 1000) | 45 | 0.9 (0.5; 1.7) | 0.1 | 6.3 |
| Demographic variables | ||||
| Median age | 46 | 19.1 (17.7; 20.3) | 15.1 | 37.4 |
| Aged 65 years (%) | 46 | 3.01 (2.7; 3.4) | 2.1 | 10.9 |
| Female sex (%) | 46 | 50.1 (49.9; 50.6) | 44.6 | 51.5 |
| Population (mil.) | 46 | 12.5 (2.4; 26.3) | 0.1 | 206.1 |
In the correlation analysis, a few variables showed relevant [r(s) = 0.6 to < 0.8] correlations [Supplementary Table 2]. Median age and the share of population aged 65 years or older presented a correlation coefficient of 0.70 (P < 0.0001). For further investigations, only age 65 years or older was retained as a covariate.
The results of the regression analyses show RR estimates in univariable and multivariable models, adjusted for demographic characteristics.
When the socioeconomic variables were introduced separately into the model, an increase of the HDI by 0.10 resulted in a crude RR of 0.74 (95%CI: 0.63-0.86), indicating a lower fatality in countries with higher development index [Table 3]. Adjustment for population density and age changed the RR slightly to 0.77 (95%CI: 0.61-0.96). Similarly, an increase by 0.2 in the political stability index resulted in decreased fatality by a factor of 0.93 (95%CI: 0.90-0.97) in the univariable analysis, and by a factor of 0.95 in the multivariable analysis.
Effect of socioeconomic, public health and demographic variables on COVID-19 fatality. Results of Poisson regression modelling
| Variables | Obs. (n) | Crude RR (95%CI) | P | Adj. RR§ (95%CI) | P |
| Socioeconomic indicators | |||||
| HDI | 208 | 0.74 (0.63-0.86) | < 0.0001 | 0.77 (0.61-0.96) | 0.023 |
| Political stability index | 213 | 0.93 (0.90-0.97) | 0.001 | 0.95 (0.91-0.99) | 0.026 |
| Public health indicators | |||||
| Diabetes mellitus prev. | 213 | 1.21 (0.80-1.83) | 0.372 | 1.55 (1.14-2.11) | 0.006 |
| CVD death rate | 213 | 1.44 (1.03-2.01) | 0.034 | 1.36 (0.94-1.95) | 0.100 |
| CRD death rate | 213 | 1.08 (0.87-1.33) | 0.482 | 1.01 (0.82-1.25) | 0.892 |
| Handwashing facilities | 183 | 0.98 (0.87-1.10) | 0.707 | 0.95 (0.87-1.04) | 0.284 |
| Hospital beds per 1000 | 208 | 0.80 (0.72-0.88) | < 0.0001 | 0.82 (0.74-0.97) | 0.018 |
| Demographic Indicators | |||||
| Population density | 208 | 0.82 (0.71-0.94) | 0.006 | 0.84 (0.71-1.00) | 0.05 |
| Share of aged 65 years | 213 | 0.86 (0.75-0.98) | 0.03 | 0.84 (0.71-1.00) | 0.05 |
| Time period | |||||
| 24.02.2020-24.05.2020 | 213 | 2.68 (1.85-3.88) | < 0.0001 | 2.62 (1.84-3.74) | < 0.0001 |
| 25.05.2020-23.08.2020 | 213 | 1.21 (0.92-1.59) | 0.182 | 1.17 (0.89-1.54) | 0.235 |
| 24.08.2020-22.11.2020 | 213 | 0.96 (0.73-1.25) | 0.747 | 0.90 (0.69-1.18) | 0.483 |
| 23.11.2020-21.02.2021 | 213 | 1.20 (0.89-1.61) | 0.218 | 1.22 (0.89-1.66) | 0.205 |
| 22.02.2021-23.05.2021 | 213 | Ref. | Ref. |
The results for the public health indicators were as follows: a higher diabetes prevalence and a higher mortality from cardiovascular diseases or chronic respiratory diseases are associated with a higher COVID-19 fatality, with significant result for cardiovascular disease in the univariate analysis, and for diabetes in the multivariable analysis. The variable hospital beds per 1000 people showed significant results in both the crude and adjusted models. Increasing the variable by one hospital bed per 1000 people led to a decreased CFRL by factor 0.80 (95%CI: 0.72-0.88) in the crude model and a factor 0.82 (95%CI: 0.74-0.97) when adjusted. A higher rate of handwashing facilities shows a small, non-significant positive effect.
Since there is a strong correlation between the variables as shown above, the multivariable model including all variables led to higher variances of the effect estimates. However, the overall results did not change much. For example, the estimate for the HDI changed to 0.79, however with a wider 95% confidence interval as (0.55-1.13). When we excluded the first time period’s COVID-19 cases and deaths, in both the univariable and multivariable models, the results remained largely unchanged.
In the sensitivity analysis, we restricted the analysis to observations with more than 2000 reported cases within a time period thus omitting observations from smaller countries [Supplementary Table 3]. This change resulted only in minor changes in estimates that were in accordance with the results of
To test the models’ robustness, the analyses were repeated with the calculated ranks. The results presented similar trends, supporting the results from the main analysis [Supplementary Table 4].
DISCUSSION
The COVID-19 pandemic presents global health, economic, and social challenges. Studies on the influence of socioeconomic and public health factors are scarce, and the African continent or certain areas are underrepresented research-wise. In terms of past outbreaks and theorised associations with social position, the sub-Saharan African region was predicted to fare poorly in the pandemic. This study used aggregated, country-level data to analyse the associations of socioeconomic and public health indicators with the CFR of COVID-19 in 46 sub-Saharan African countries.
Socioeconomic indicators and demographic characteristics
An increasing HDI indicated a negative association with COVID-19 CFRL. The direction of the impact was in line with theories that disadvantaged populations are at greater risk for infection and death due to, for example, fewer opportunities to carry out preventive actions[9,19]. Previous studies, using sub-national data, reported opposite effects, where an increase in HDI presented a higher COVID-19 spreading rate and, in one case, a higher incidence and death rate[6,12,13]. Liu et al.[6] found that an increase in HDI was positively associated with infection and fatality rates comparing regions within Italy. However, it should be noted that the Italian areas included had a median HDI of 0.89, which placed the whole sample within a very high HDI by definition[6] and which is therefore not to be compared with the sub-Saharan countries.
A higher population density was negatively associated with COVID-19 in our analyses. Other studies, each focusing on one country and using sub-national data, found positive associations where higher population density increased infection rates[12,13]. Their findings would align with theories that assume that the denser people live together, the greater the chance of encountering others and thus being exposed to a risk of infection. Cao et al.[11] found no indication that population density impacted COVID-19 CFR globally. Higher population density promotes transmission, but it is also an indication that people may be living in urban areas. Social inequalities are present within cities and more rural regions; however, it could indicate that healthcare resources and testing facilities are more readily available in urban areas.
So far, few studies have been conducted to investigate the associations between political stability and COVID-19. This study found that an increase in the political stability index presented a decreasing COVID-19 CFRL. Previous research comparing the COVID-19 spread in the Arab Levant countries had similar findings. They concluded that regions enduring war and conflict were the most vulnerable to the disease’s spread. The global pandemic exposed inadequacies in their health care systems and related sectors. The government response was often slow, and measures to prevent further spread were unattainable due to lack of resources or public dissent. As the political stability index represents political, economic and other determinants, they suggested using it as an indicator to predict a country’s ability to respond to an outbreak[14].
Public health indicators
An increase in hospital beds per 1000 resulted in a slight decrease in CFRL. A previous study found similar results[15]. A positive linear relationship was observed between hospital beds per 1000 and the HDI of the countries in this work. Bassino et al.[13] used health expenditures per capita to test a similar theory and found significant negative associations with COVID-19 prevalence in Japan. It seems reasonable to assume that the higher availability of health care resources positively influences the case-fatality rate of COVID-19.
The impact of pre-existing health conditions on the COVID-19 CFR was tested using variables on diabetes mellitus prevalence, cardiovascular disease and chronic respiratory disease death rate. In this study, increased diabetes mellitus prevalence and cardiovascular disease death rate were associated positively with COVID-19 CFRL. The results were in accord with the findings of previous studies and supported the recommendations that these underlying medical conditions are risk factors for worse COVID-19 disease progression[1,15,21]. Other research concluded in a multi-country comparison of COVID-19 CFR that comorbidities significantly impact the outcome at the population level. Specifically, they found that the countries with the highest disability-adjusted life years lost to cardiovascular diseases, diabetes mellitus, and cancer presented the highest CFR[15]. In their multi-country study, Cao et al.[11] found an adverse association between diabetes mellitus prevalence, as well as cardiovascular disease death rate, and CFR.
A 10% increase in the share of the population with basic handwashing facilities resulted in little to no effects. It is the variable that had the highest number of missing data (15%), and the results should be interpreted with this knowledge in mind. Several studies have excluded the variable from their analysis because of concerns that the excess of missing data would distort the results and expressed doubts about the explanatory power[11].
Interrelationships
A striking feature mentioned in this work and previous research was the interrelationships of the variables. The presence of pre-existing medical conditions was considered a risk factor for COVID-19 and its progression. Also, the share of the population aged 60 years or older are said to live with heightened risk of severe disease progression[1]. The sub-Saharan African region has a median age of 19 and a median proportion of persons aged 65 years or older of 3%. In comparison, the European Union member states have a median age of 44 years and a share of populations aged 65 years or older of 21%[30]. Older age has been associated with an increase in, for example, cardiovascular disease, chronic respiratory disease, cancer, and diabetes mellitus. It stands to reason that these aspects may influence each other, as confirmed by previous research and official recommendations[1,22]. In sub-Saharan Africa, favourable factors come together with the assumption that a younger age structure and lower proportions of pre-existing health conditions reduce the progression of COVID-19. They thus may contribute to explaining why fewer deaths were reported, and the COVID-19 CFR was lower. Also, many countries have prior experience with disease outbreaks and resistance to preventive measures may be lower[17,22].
Nevertheless, some countries are exposed to socioeconomic deprivation, which is reflected in the low median HDI (0.54) and, according to the median of the political stability index, live in regions where armed conflict, social, ethnic, and religious unrest, terrorism, international tensions, and the likelihood of a disorderly transfer of governmental power may be high or already taking place[26]. As Bizri et al.[14] noted, pandemic response measures may be delayed or not introduced in more unstable regions. This could be accompanied by a lack of resources, which could worsen the outbreak if many people contract the virus and the health system cannot cope. Resource scarcity leads to prioritisation. A shortage of COVID-19 tests or a lack of testing can lead to misjudgements in the form of under - or overreporting[14]. A research group made this finding in Zambia, where a post-mortem examination revealed that despite existing hospital policies, many of the admitted patients were not tested for COVID-19, resulting in unreported cases and, at the time of the study, unreported COVID-l9 deaths[20,21]. de Souza et al.[19] observed how COVID-19 spread in the more socioeconomically advantaged Brazilian communities and then progressed to the vulnerable municipalities. The impact in deprived areas was even more pronounced as poverty, sanitation, pre-existing medical conditions, and health care resources were already a challenge before the pandemic and were exacerbated by the disease outbreak. They predicted that the proportion of people living in poverty would increase again due to the impact of the pandemic[19].
Strengths and limitations
Validated, reliable, and up-to-date open-source databases were available for this international comparative study focusing on sub-Sahara Africa. However, the use of databases and aggregated data must also be noted as a limitation. The origin and processing of the data were presented transparently. Nevertheless, secondary data may be inaccurate or altered over time. Appropriate steps to avoid errors, for example, sample comparisons with other databases, have been taken. Since the database operators were dependent on the regional health offices to gather data, there is an unknown margin of under - or overreporting for the COVID-19 cases and deaths. Even though many of the countries already have experience with disease outbreaks, it was not possible to assess each country’s data quality. The fact remains that in resource-constrained settings, the collection, verification, and aggregation of data may be difficult to accomplish[11,22]. Overall, there are some differences between countries in how a COVID-19 case or death is defined. In some regions, only cases that die from the disease were counted. At the same time, elsewhere, all deaths within a specific time window were reported if a person had died and tested positive beforehand[11,27].
The COVID-19 case-fatality rate was chosen as this study’s outcome. CFR use during an ongoing outbreak is not without controversy, as misinterpretation may occur, especially in the early stages, when symptomatic cases are more likely to be detected than asymptomatic cases. In addition, test capacities are very limited. This leads to an overestimation of CFR. As testing rates usually rise and more cases are detected during the outbreak, the CFR should reflect a more realistic value. This logic depends on the possibility of increasing test capacities, which is a major challenge for resource-constrained regions[27].
The WHO suggested including the “number of recovered from disease” in the CFR formula and considering possible delays in reporting cases and deaths. The number of recovered from COVID-19 was not available for the countries included in this study. To mitigate the bias from delayed reporting, the choice was made to calculate the CFR with cumulative cases and deaths for five 13-week periods for each country and repeat these calculations to create the CFRL.
When the study was conducted, there were no specifications on the distribution of COVID-19 cases and deaths by age or sex. The available variable “share of the population ≥ aged 65 years” was used for adjustment in the models. Nevertheless, residual confounding is likely to remain. In connection with data availabilities, the variables represented country-level data. Concerning the socioeconomic and public health indicators, other research has established that substantial differences may also exist on subnational or individual levels, making the study vulnerable to aggregation bias.
This study found that increasing the selected socioeconomic indicators (i.e., HDI, population density, and political stability index) was negatively associated with COVID-19 CFRL. The public health indicators diabetes mellitus prevalence and cardiovascular disease death rate showed a positive association with CFRL. Increased hospital beds were negatively associated with COVID-19 CFRL, and chronic respiratory disease and handwashing facilities showed little to no effect.
The results draw attention to possible vulnerabilities of sub-Saharan Africa. There is the assumption that the young age structure and the lower proportions of pre-existing medical conditions mitigate some of the effects of the pandemic. These facilitating factors are contrasted by socioeconomic and public health challenges that have emerged as possible drivers for the region.
This study provided a first insight into the associations of socioeconomic and public health indicators with COVID-19 CFR on a population level. There are some limitations due to the design and data accuracy and availability, but this work should be used as a starting point for further research. The collection of sub-national or individual data is seen as the next appropriate step to examine the impact of possible inner-country differences.
DECLARATIONS
Authors’ contributionsCollection and curation of the data: Kreienbrinck A
Data analysis: Kreienbrinck A, Becher H
Supervising the paper: Zeeb H, Becher H
Writing: Kreienbrinck A
Availability of data and materialsThe data used for this research were obtained from open-source databases of the ECDC, ourworldindata.org, and the World Bank. All sources are referenced in the article.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2021.
REFERENCES
1. WHO. Coronavirus disease (COVID-19). Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19 [Last accessed on 27 Dec 2021].
2. WHO. Coronavirus. Overview. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_1 [Last accessed on 27 Dec 2021].
3. WHO. Coronavirus. Prevention. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_2 [Last accessed on 27 Dec 2021].
4. WHO. Coronavirus. Symptoms. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_3 [Last accessed on 27 Dec 2021].
5. WHO. Coronavirus disease (Covid-19) Dashboard. Available from: https://covid19.who.int/ [Last accessed on 27 Dec 2021].
6. Liu K, He M, Zhuang Z, He D, Li H. Unexpected positive correlation between human development index and risk of infections and deaths of COVID-19 in Italy. One Health 2020;10:100174.
7. Troumbis AY. Testing the socioeconomic determinants of COVID-19 pandemic hypothesis with aggregated Human Development Index. J Epidemiol Community Health 2020; doi: 10.1136/jech-2020-215986.
8. Khazaei Z, Mazaheri E, Hasanpour-dehkordi A, et al. COVID-19 pandemic in the world and its relation to human development index: a global study. Arch Clin Infect Dis 2020; doi: 10.5812/archcid.103093.
9. Khalatbari-Soltani S, Cumming RC, Delpierre C, Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health 2020;74:620-3.
10. Singu S, Acharya A, Challagundla K, Byrareddy SN. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front Public Health 2020;8:406.
11. Cao Y, Hiyoshi A, Montgomery S. COVID-19 case-fatality rate and demographic and socioeconomic influencers: worldwide spatial regression analysis based on country-level data. BMJ Open 2020;10:e043560.
12. Ahmadi M, Sharifi A, Dorosti S, Jafarzadeh Ghoushchi S, Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ 2020;729:138705.
13. Bassino JP, Ladmiral G. Socio-economic factors influencing COVID-19 spread in Japan; evidence from the second wave (March-May 2020). 2020; doi: 10.13140/RG.2.2.12371.60961.
14. Bizri NA, Alam W, Mobayed T, Tamim H, Makki M, Mushrrafieh U. COVID-19 in conflict region: the arab levant response. BMC Public Health 2021;21:1590.
15. Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep 2020;10:18909.
17. Africa CDC. Disease Outbreak Archive. Available from: https://africacdc.org/disease-outbreak/ [Last accessed on 27 Dec 2021].
18. Cabore JW, Karamagi HC, Kipruto H, et al. The potential effects of widespread community transmission of SARS-CoV-2 infection in the World Health Organization African Region: a predictive model. BMJ Glob Health 2020;5:e002647.
19. de Souza CDF, Machado MF, do Carmo RF, et al. Human development, social vulnerability and COVID-19 in Brazil: a study of the social determinants of health. Infect Dis Poverty 2020;9:124.
20. Mwananyanda L, Gill CJ, MacLeod W, et al. Covid-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ 2021;372:n334.
21. Western Cape Department of Health in collaboration with the National Institute for Communicable Diseases, South Africa. Risk Factors for Coronavirus Disease 2019 (COVID-19) Death in a Population Cohort Study from the Western Cape Province, South Africa. Clin Infect Dis 2021;73:e2005-15.
22. Musa HH, Musa TH, Musa IH, Musa IH, Ranciaro A, Campbell MC. Addressing Africa’s pandemic puzzle: Perspectives on COVID-19 transmission and mortality in sub-Saharan Africa. Int J Infect Dis 2021;102:483-8.
23. ECDC Data Source. Data on 14-day notification rate of new COVID-19 cases and deaths. Available from: https://www.ecdc.europa.eu/en/publications-data/data-national-14-day-notification-rate-covid-19 [Last accessed on 27 Dec 2021].
24. OWID. Data Source: Data on COVID-19. Available from: https://github.com/owid/covid-19-data/tree/master/public/data [Last accessed on 27 Dec 2021].
25. OWID. Data Source: age-standardised deaths rates for chronic respiratory disease. Available from: https://ourworldindata.org/grapher/respiratory-disease-death-rate?region=Africa [Last accessed on 27 Dec 2021].
26. World Bank. Data Source: Worldwide Governance Indicators. Political stability and absence of violence/terrorism: estimate. Available from: https://databank.worldbank.org/source/worldwide-governance-indicators# [Last accessed on 27 Dec 2021].
27. WHO. Estimating mortality from COVID-19. Available from: https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19 [Last accessed on 27 Dec 2021].
28. United Nations Development Programme. Human development index (technical notes). Available from: http://hdr.undp.org/sites/default/files/hdr2020_technical_notes.pdf [Last accessed on 27 Dec 2021].
30. Eurostat. Population structure and ageing. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#Median_age_is_highest_in_Italy [Last accessed on 27 Dec 2021].
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Kreienbrinck A, Zeeb H, Becher H. Associations between socioeconomic and public health indicators and the case-fatality rate of COVID-19 in sub-Saharan Africa. One Health Implement Res 2021;1:66-79. http://dx.doi.org/10.20517/ohir.2021.08
AMA Style
Kreienbrinck A, Zeeb H, Becher H. Associations between socioeconomic and public health indicators and the case-fatality rate of COVID-19 in sub-Saharan Africa. One Health & Implementation Research. 2021; 1(2): 66-79. http://dx.doi.org/10.20517/ohir.2021.08
Chicago/Turabian Style
Kreienbrinck, Annika, Hajo Zeeb, Heiko Becher. 2021. "Associations between socioeconomic and public health indicators and the case-fatality rate of COVID-19 in sub-Saharan Africa" One Health & Implementation Research. 1, no.2: 66-79. http://dx.doi.org/10.20517/ohir.2021.08
ACS Style
Kreienbrinck, A.; Zeeb H.; Becher H. Associations between socioeconomic and public health indicators and the case-fatality rate of COVID-19 in sub-Saharan Africa. One. Health Implement. Res. 2021, 1, 66-79. http://dx.doi.org/10.20517/ohir.2021.08
About This Article
Copyright
Data & Comments
Data
 Cite This Article 5 clicks
Cite This Article 5 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.