Introduction
The whole world witnessed the outbreak of the COVID-19 pandemic due to the SARS-Cov-2 infection, presenting a public health problem that was declared by the World Health Organization as a state of emergency of international interest on January 30, 2020. The pandemic fundamentally changed the natural course of activity of all economic sectors worldwide. One of the areas that were deeply influenced is the health services sector. At the level of the European Union, the COVID-19 pandemic gradually spread, reaching new negative records day by day, reaching the maximum in the spring of 2020. This crisis has significantly affected the daily activities everywhere in order to prevent the dramatic effects of the pandemic and reduce mortality and morbidity associated with this phenomenon. In this context, in addition to providing essential healthcare to the population, a firm and prompt attitude is called for through specifically targeted actions to combat the COVID-19 pandemic and limit its effects on the population.
Health Status in Europe Before the Covid-19 Pandemic
The European Union (EU) is a political and economic party that includes 27 Member States and respects a set of common principles and values (human dignity, freedom, democracy, equality, the rule of law and human rights) as well as the health of its citizens. The EU includes the recent trends in key health indicators, in the context of the COVID-19 pandemic, that are vital in coordinating its work. Among these health indicators, the authors of this paper consider it important to analyze life expectancy, as well as the mortality rate and especially the rate of preventable deaths, because these variables provide a real picture of the demand for health services of the population. To get a clearer picture of the magnitude of the health crisis generated by the COVID-19 pandemic at the EU level, this paper will summarize the health condition of the EU population and the main challenges facing the proper functioning of the health services sector before the pandemic: demand for health services and healthcare provided.
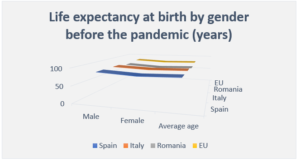
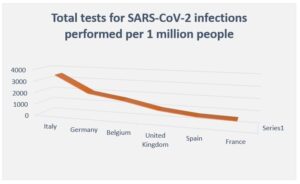
The 2018 European Commission report highlights that life expectancy at birth reached 81 years in EU Member States in 2016, with Spain and Italy having the highest life expectancy exceeding 83 years. This bears some risks in terms of the consequences of the COVID-19 pandemic. While, on the other hand, this indicator is still limited to around the age of 75 in countries such as Romania, Bulgaria, Latvia and Lithuania. As illustrated in Figure no. 1, in all countries, both inside the EU and outside, women have a longer life expectancy than men, and in the EU, in the pre-pandemic period, this indicator exceeded 80 years in about two-thirds of the Member States.
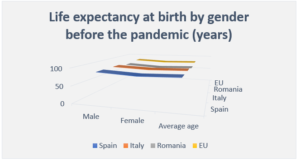
Fig. 1: Life expectancy at birth by gender in EU Member States in 2016
(Source: Data processing performed by authors based on information from the Eurostat database
Research on the mortality rate in the EU in the period before the pandemic shows that the leading causes of death are mainly cardiovascular diseases and various cancers, followed by respiratory diseases and external causes of death, including accidents of all kinds, suicide, homicide or other causes. It is alarming that in Romania, the cardio-circulatory mortality rate is on the penultimate place before Bulgaria in the analysis of all EU Member States, while deaths due to cancer have rates similar to those of other Member States in the EU (OECD, Eurostat and WHO, 2017). It should be observed that Spain and Italy, as described by the positive trend in the analysis of life expectancy at birth as well as in the case of the mortality rate, retain one of the top three favorable positions among the Member States of the European Union, registering values of about half of Bulgaria and Romania (OECD, Eurostat and WHO, 2017).
The rate of preventable deaths largely overlaps with these values because through adequate primary prevention and adequate population screening, this health indicator could be significantly improved, and the context presented before the pandemic already signaled an inefficiency of the health system in providing health services and preventing certain diseases.
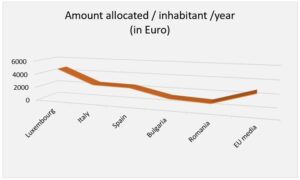
To study the medical care provided to the population before the pandemic, the material and human resources are analyzed from the perspective of the sanitary material costs, equipment, and the shortage of medical personnel compared to the pandemic period. As defined by the System of Health Accounts (OECD, Eurostat and WHO, 2017), the expenditure on the health system refers to costs for all medical services and goods, prevention programs, screening and public health, regardless of the method of financing. Figure no. 2 shows the costs allocated to health services per capita in each EU Member State. The wide range of amounts recorded is due to various social and economic factors being closely related to the economic performance of each state, the organization, as well as the proper functioning and structure of each health system. The EU state that allocates the largest budget for health services per capita is Luxembourg with 4713 euros in 2017, while at the opposite pole, the EU states with the lowest values of the same indicator are Bulgaria with 1234 euros/capita in 2017 and Romania with 983 euro/inhabitant in 2017, respectively. Italy and Spain are close to the EU average (2773 euro/inhabitant/year), registering 2551 euro/inhabitant/year, and 2446 euro/inhabitant/year, respectively.
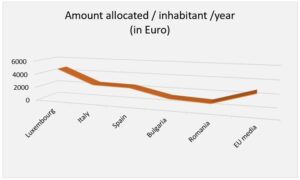
Fig. 2: Health expenditure per capita by country in EU Member States in 2017
(Source: Authors’ processing based on data provided by the Eurostat database,“WHO Global Health Expenditure Database”)
It is important to note that this wide range of budgets allocated by each state for health services provided to the population is explained by the close relationship between a country’s income level and how much that country’s population spends on health care according to the legislative regulations and economic development of each state.
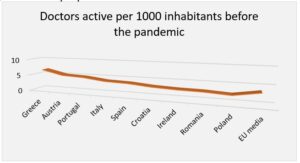
To address the deficiencies of the health system in each EU state, human resources are analyzed from the perspective of the shortage of medical staff before the pandemic period. The data refer to all doctors with the right to practice medicine freely, resulting in an overestimation in some cases. This overestimation is explained by the fact that the data include not only doctors providing direct care to patients, but also doctors working in the health sector and who have the functions of managers, academics, researchers, etc. (adding another 5-10%).
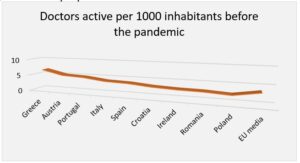
Fig. 3: Practicing doctors per 1000 population by country in EU Member States in 2016
(Source: Authors’ processing based on data provided from the Eurostat database)
As it appears from Figure no. 3, Romania is one of the last places among the states of the European Union when analyzing the number of doctors per 1000 inhabitants with a value of 2.8; while Italy and Spain are slightly above the EU average (3.6 doctors/1000 inhabitants) with a coverage of 4.0 doctors/1000 inhabitants and 3.8 doctors/1000 inhabitants, respectively.
To explain the shortage of the medical staff in Romania, it is necessary to consider that after January 2007, when Romania became a member state of the European Union, the Romanian health system witnessed a phenomenon of the emigration of highly trained medical professionals to other EU Member States searching for better living and working conditions. Thus, Romania remained with the lowest number of doctors and nurses in relation to the number of inhabitants, compared to both the EU average and the years before the EU accession. The decision of the medical staff to emigrate was largely due to the working conditions, overwork and insufficient income (Duran et al., 2019).
Health Status in Europe During the Covid-19 Pandemic
Given that the economic situation and the medical infrastructure of a state are the determining factors in assessing a country’s ability to cope with and minimize losses due to the pandemic, are further analyzed, the main indicators of health during the COVID-19 pandemic (life expectancy at birth, mortality rate and preventable death rate), reflect the demand for health services, as well as the material and human resources available during the pandemic in the EU, particularly in the situation of EU Member States: Romania, Italy and Spain.
Health experts note that states with a high life expectancy population and a higher percentage of the aging population, as in Italy and Spain, are facing the risk of a large number of deaths caused by COVID-19 (SA Shams et al., 2020). It has already been stated by the WHO that SARS-CoV-2 infection leads to higher mortality rates among people over 60 and that there is a direct exponential relationship between old age and mortality.
The latest data published by Eurostat show that in March-November 2020, there were more than 450,000 deaths in Europe compared to the values of mortality rates between 2016 and 2019 in the same geographical area. Although there was no direct evidence of the cause of this excess mortality, it can be considered that most of the deaths were due to SARS-CoV-2 infection, as the highest reported mortality rates took place in the period between March-April 2020, and October-November 2020. These periods overlap with the first and second waves of the pandemic in all EU Member States.
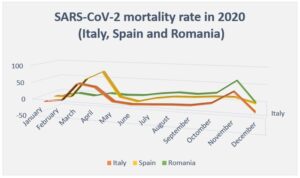
The first European country to report a sharp increase in the number of SARS-CoV-2 infections was Italy, recording deaths by 49.4% above average in March 2020, as illustrated in Figure no. 4. Figure 4 also presents the situation of death rates during 2020 in Spain, where there is an increase in the percentage of excessive mortality in April 2020, while in Spain, this health indicator showed an increase of 79.4% compared to the period prior to the pandemic. It is important to note that the variable “excessive mortality” refers to the number of additional deaths in comparison to a reference interval; that is the average number of deaths for a given month during the four years from 2016 to 2019 in the same geographical region.
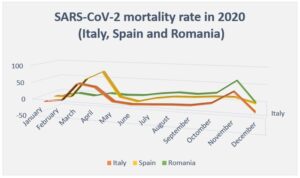
Fig. 4: Excessive mortality in EU countries in 2020 (Italy, Spain and Romania)
(Source: Data processing performed by authors based on information from the Eurostat database)
In Romania, as illustrated in Figure no. 4, there is an increase in the mortality rate in the second half of 2020, with a peak in November 2020 when the second wave of the pandemic increased mortality by more than 60% compared to November of the years before the pandemic. It is worth noting that in Romania, unlike Italy and Spain, the first wave of the pandemic (from March-April 2020) did not register unfavorable values of mortality rates. This trend can be explained by the decisions of the Romanian authorities, which were different from those taken in other EU Member States.
It is important to highlight that in all the 3 EU Member States analyzed, the second wave of the pandemic was felt very differently from one state to another. The rate of excessive mortality broadly overlaps with the rate of preventable deaths, this being explained by the wide range of these health indicators in different states across the EU, as a consequence of the decisions made by the authorities in their attempt to cope with the adverse effects of the pandemic. The mortality rate rose by about 25% above average in all 27 EU Member States in April during the first wave of the pandemic.
The pandemic has also significantly impacted the health expenditure due to new pandemic costs that have been added to the budgets. These new costs included diagnostic tests, protective sanitary materials, equipping hospitals with mechanical ventilators for patients, the costs associated with caring for patients infected with SARS-CoV-2, consumables in health facilities, the purchase of vaccines and their administration costs for the population.
As illustrated in Figure no. 5, on March 20, 2020, Italy, one of the EU Member States that were heavily affected by the first wave of the pandemic, ranks third in the world and first among the EU Member States in the number of diagnostic tests performed on one million people, while Spain is ranked eleventh in the world and fifth among the EU Member States. It should be noted that from these data, the EU Member States that have performed the most diagnostic tests are Italy, Germany, Belgium, Spain and France; these are also states whose economic performance allows them to allocate a higher budget for health services per capita than other member states such as Romania.
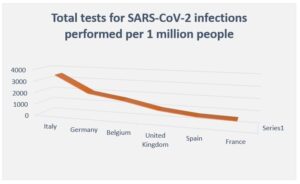
Fig. 5: Total tests for SARS-CoV-2 infections performed per 1 million people in different countries on March 20, 2020.
(Source: Data processing performed by authors based on information from official country reports)
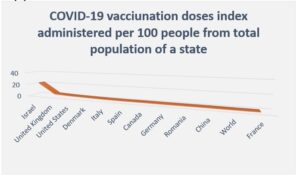
Another source of additional costs associated with the pandemic in the health services sector was the immunization of the population through vaccination. On January 13, 2021, Italy, Spain and Romania administered more doses of SARS-CoV-2 vaccine to the population than the global vaccination average (Figure no. 6) so that the Italian population was three times more vaccinated compared to the average of this indicator worldwide (1.32 compared to 0.38). This process does not correlate with the economic development of each state, but rather with the awareness of the possibility of ending the pandemic as well as with the decisions and actions of the authorities in each country.
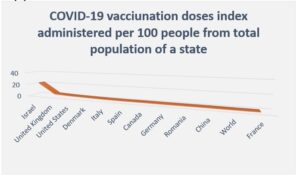
Fig. 6: COVID-19 vaccination doses index administered per 100 people from the total population of a state, in different countries on Jan 13, 2021.
(Source: Data processing performed by authors based on information from official country reports)
Regarding the shortage of medical staff during the pandemic, this aspect was well known in the EU before the pandemic, as mentioned earlier; however, the pandemic exacerbated this deficit because in countries that were severely affected by SARS-CoV-2, the large number of new patients diagnosed needing medical care have further increased the workload of medical staff. Consequently, a temporary phenomenon called “professional retraining” appeared in some areas of Italy. This phenomenon meant that doctors of any specialty in a hospital would have to provide the medical care of intensive care doctors because many patients urgently needed such care (P. Tozzo et al., 2020).
Innovative Solutions to Prepare a Supporting Health System for Major Crisis Situations
As new research emerges, connected to how successful different countries have responded to the SARS COVID-19 pandemic, it is found that the level of development of a country does not mean that the health system is better capable of successfully navigating through the crisis (Saha, S. and Pai, M., 2021). Along with the efforts exerted to fight against the pandemic, it is found that in the race toward vaccination, new threats are unfolding such as uneven vaccine purchase (10 countries account for 75% of the total vaccine purchases) or vaccine nationalism.
The exponential rate of the virus’s spread has made it impossible for hospitals and doctors to accommodate an overwhelming number of patients in a short time. The traditional way of handling more patients with creating more caretaking spaces and recruiting more healthcare personnel, becomes impossible to implement. A different solution was needed, and, in some cases, it came in the form of Artificial Intelligence (AI) and Robotic Process Automation (RPA) triage system that helped in coping with inquiries from patients, staff, ambulatory clinics as well as hotline and chatbots. Such systems managed to keep most of the mild-symptoms patients in self-quarantine while offering other alternatives for the more severe cases.
AI and machine learning were also used by studies in China to reveal the differences in patients with COVID-19 computer tomograph scans and those with other pneumonia. Other studies focus on using AI to find new treatment opportunities (Farrugia, G. and Plutowski, R., 2020)
Innovations that have seen a spike in demand as a result of the COVID- 19 pandemic, although many of them existed before the outbreak, include 3D printing technology, healthcare wearables, flexible manufacturing systems and bid data analytics (Brem, A., Viardot, E. & Nylund, P. A., 2021). Examples of how these technologies have helped in fighting the pandemic include the 3D printing of N95 masks and elements for respirators, manufacturing systems that could pivot toward sanitizers, diagnostic tests and ventilators, the use of big data sets and AI to make better logistics decisions or healthcare recommendations, the use of healthcare wearables that can track body sensors and health values or even physically track if people are committed to quarantine or self-isolation.
Telemedicine was a great innovation, which gave the opportunity for patients who were still in need of healthcare but could not personally come for appointments to benefit from remote medical care. Also, telemedicine has helped in keeping in touch with patients suffering mild symptoms of COVID- 19 (Zimmerling, A. & Chen, X., 2021).
The Internet of Things, or IoT, is about creating a connected world where different devices communicate with each other and share information to create efficiencies and end to end holistic experiences. IoT has played a great role during COVID-19 through the technology of connecting patients’ data from smart sensors (e. g.: temperature, blood oxygen levels, blood pressure, sugar levels, etc.), medical appointment reminders, exercise applications and even the development of smart hospitals. This has helped doctors create a centralized information system for monitoring, which provides patients with the best treatment services (Javaid, M. and Khan, I. H., 2021).
A different aspect connected to innovation during COVID-19 and how technologies, best practices and out of the box ideas are developed, is the focus on leadership trainings, courses and competences as a means to adapt fast to different situations. The focus on agility, learning through experimentation and continuous iterations are leading the way on how successful companies and businesses run today. However, these concepts are not so widely spread when it comes to competence development programs in public spaces such as hospitals.
Healthcare institutions, which are focusing on the learning of 2020 and offering leadership trainings with the aim to better help healthcare leaders to innovate, start increasing in numbers, Examples of focus areas for such trainings include shared purpose, positive relationship building, focus on empathy, using appreciative enquiry or showing compassion (Graham, R. N. J and Woodhead, T., 2021).
Based on the existing disruptive innovations happening in the medical sector before and especially during the COVID-19 pandemic, the authors of the article have proposed the following possible innovative development and adoption suggestions:
– Remote investigations that go beyond the need to have a centralized unit such as the hospital, but rather a decentralized platform where demand; in this case the patients, meets supply or qualified medical specialists, thus saving time and money. There are already existing solutions that showcase this possibility, where companies like Teladoc Health are leading this space.
– Home ultrasound portable devices attached to smartphones can help patients investigate and see ultrasound scans from their houses, while sharing a live or even a recorded scan with the healthcare doctors via telemedicine. Companies such as Butterfly Network showcase these technologies quite well.
– 3D printing can further facilitate healthcare technology not only by using inorganic materials, but also by using new development techniques to make organic imprints (bioprinting), such as human skin or even entire organs, possible. Companies such as Organovo, Cyfuse biomedical, Cellink or Aspect Biosystems are pioneering this field.
– Leadership development and business courses are perhaps one of the often ignored innovation enablers. Usually, innovation is outsourced from hospitals and health centers, so healthcare specialists are recommended to focus on developing their healthcare expertise only. However, as learned from the COVID-19 pandemic, all organisms and all businesses, whether private or public, need to constantly adapt to a volatile, uncertain, complex and ambiguous (VUCA) world. This can be done by equipping people with relevant leadership, technological and business knowledge.
Conclusions
The COVID pandemic made people see that there are losses to be accepted and there are new perspectives for the future. Thus, the pandemic period fundamentally influenced the economy in all countries worldwide, having a major global impact. Some areas of activity were on the verge of collapse, as in the hotel industry; there were areas of activity that were transposed online, as in the case of education; and there were areas that developed exceptionally, as in the field of online sales or the pharmaceutical industry. The analysis of these aspects can provide us with new perspectives to adapt to and overcome the major emergency crisis of the COVID-19 pandemic. Regardless of the state of emergency or the natural disaster, it is important to realize that the health system is the main pillar that can fight against this phenomenon and that a functional as well as an adequate health system is the only way to minimize losses and protect population in all countries.
(adsbygoogle = window.adsbygoogle || []).push({});
References
- Zimmerling A, Chen X. (2021), ‘Innovation and possible long-term impact driven by COVID-19: Manufacturing, personal protective equipment and digital technologies’, Technology in Society, Volume 65, 101541, ISSN 0160-791X, https://doi.org/10.1016/j.techsoc.2021.101541
- Brem A, Viardot E, Nylund PA., (2021), ‘Implications of the coronavirus (COVID-19) outbreak for innovation: Which technologies will improve our lives?’, Technol Forecast Soc Change. 2021 Feb;163:120451. doi: 10.1016/j.techfore.2020.120451.
- Duran A., Chanturidze T., Gheorghe A. and Moreno A., (2019), ‘Assessment of Public Hospital Governance in Romania: Lessons From 10 Case Studies’, Int J Health Policy Manag., Apr., 8(4), pp:199-210.
- Euronews, ‘EU excess deaths in 2020: Country-by-country breakdown of COVID-19’s impact’. [Online], Euronews, [Retrieved February 17 ,2021], https://www.euronews.com/2021/02/17/eu-excess-deaths-in-2020-country-by-country-breakdown-of-covid-19-s-impact
- Farrugia G., Plutowski R. W. (2020), ‘Innovation Lessons From the COVID-19 Pandemic’, Mayo Clinic Proceedings, Volume 95, Issue 8, Pages 1574-1577, ISSN 0025-6196, https://doi.org/10.1016/j.mayocp.2020.05.024
- Lai L, Wittbold KA, Dadabhoy FZ, Sato R, Landman AB, Schwamm LH, He S, Patel R, Wei N, Zuccotti G, Lennes IT, Medina D, Sequist TD, Bomba G, Keschner YG, Zhang HM. (2020), ‘Digital triage: Novel strategies for population health management in response to the COVID-19 pandemic’. Healthc (Amst). Dec;8(4):100493. doi: 10.1016/j.hjdsi.2020.100493.
- Javaid M., Khan I.H., (2021) ‘Internet of Things (IoT) enabled healthcare helps to take the challenges of COVID-19 Pandemic’, Journal of Oral Biology and Craniofacial Research, Volume 11, Issue 2, Pages 209-214, ISSN 2212-4268, https://doi.org/10.1016/j.jobcr.2021.01.015
- Pamela Tozzo, Caterina Politi, Andrea Gabbin, Luciana Caenazzo, (2020), ‘To take care of those on the front line against Covid-19: Is it possible to limit medical liability?’, Science & Justice Volume 60, Issue 4, July 2020, Pages 311-312.
- Graham R.N.J., Woodhead T., (2021), ‘Leadership for continuous improvement in healthcare during the time of COVID-19’, Clinical Radiology, Volume 76, Issue 1, Pages 67-72, ISSN 0009-9260, https://doi.org/10.1016/j.crad.2020.08.008
- Saha S, Pai M., (2021), ‘Can COVID-19 innovations and systems help low- and middle-income countries to re-imagine healthcare delivery?’ Med (N Y). doi: 10.1016/j.medj.2021.02.008.
- Shahbaz A. Shams, Abid Haleem, Mohd Javaid, (2020), ‘Analyzing COVID-19 pandemic for unequal distribution of tests, identified cases, deaths, and fatality rates in the top 18 countries’, Diabetes & Metabolic Syndrome: Clinical Research & Reviews Volume 14, Issue 5, Pages 953-961.
- The European Commission, (2018) ‘Health at a Glance: Europe 2018 – State of Health in the EU Cycle’, European Commission, Published on November 22, 2018, http://doi.org/10.1787/health_glance_eur-2018-en