- 1School of Public Health, Wannan Medical College, Wuhu, China
- 2Department of Clinical Medicine, Anhui College of Traditional Chinese Medicine, Wuhu, China
Objective: To systematically review the prevalence of anxiety and depression among frontline healthcare workers during the coronavirus disease 2019 (COVID-19) pandemic.
Methods: Computers were used to search CNKI, VIP, WanFang Data, PubMed, and other Chinese and English databases. The search period was limited to December 2019 to April 2022. Cross-sectional studies collected data on the prevalence of anxiety and depression among frontline healthcare workers since the onset of COVID-19. The STATA 15.1 software was used for the meta-analysis of the included literature.
Results: A total of 30 studies were included, with a sample size of 18,382 people. The meta-analysis results showed that during the COVID-19 pandemic, the total prevalence of anxiety among frontline healthcare workers was 43.00%, with a 95% confidence interval (CI) of 0.36–0.50, and the total prevalence of depression was 45.00%, with a 95% CI of 0.37–0.52. The results of the subgroup analysis showed that prevalence of anxiety and depression in women, married individuals, those with children, and nurses was relatively high. Frontline healthcare workers with a bachelor's degree or lower had a higher prevalence of anxiety. The prevalence of depression was higher among frontline healthcare workers with intermediate or higher professional titles.
Conclusion: During the COVID-19 pandemic, the prevalence of anxiety and depression among frontline healthcare workers was high. In the context of public health emergencies, the mental health status of frontline healthcare workers should be given full attention, screening should be actively carried out, and targeted measures should be taken to reduce the risk of COVID-19 infection among frontline healthcare workers.
Systematic review registration: http://www.crd.york.ac.uk/PROSPERO/, identifier: CRD42022344706.
Introduction
At the end of 2019, the corona virus disease 2019 (COVID-19) caused by the SARS-CoV-2 virus, appeared and rapidly developed into a major international public health emergency. In the early days of the outbreak, because of the high risk, contagiousness, and lack of awareness about COVID-19, many areas stopped production and work and adopted home isolation measures to reduce the spread of the virus and the risk of infection. After unremitting efforts, China is currently in the stage of normalized prevention and control of the new crown pneumonia (1–3).
Since the outbreak of COVID-19, healthcare workers have been the core force in fighting the pandemic and are also a high-risk group for viral infection. Among them, frontline healthcare workers must always face the virus directly, mostly in a high-pressure environment, to carry out rescue and other work. People have exhibited a trend of increased mental health issues during the COVID-19 pandemic (4). Due to this type of work, the mental health of frontline healthcare workers may be more vulnerable. At the beginning of the pandemic, owing to a lack of relevant experience, anti- pandemic materials, and effective treatment methods, frontline healthcare workers were under enormous psychological pressure (5, 6). Therefore, attention should be paid to the mental health of healthcare workers, especially frontline workers. By providing them with targeted assistance and enlightenment, their psychological burden can be reduced. This will not only maintain frontline healthcare workers' mental health but will also help patients receive better treatment, and is thus, conducive to the development of follow-up pandemic prevention and control work (7, 8). Therefore, it is necessary to explore the mental health status and negative emotions of frontline healthcare workers during COVID-19, including the prevalence of anxiety and depression. This could provide data to help control the global COVID-19 pandemic (9).
Among the various possible psychological problems of frontline healthcare workers, anxiety and depression are the most common, and the situation is similar to previous public health emergencies encountered by such workers (10–12). Among healthcare workers, an existing meta-analysis (13) showed that during the COVID-19 period, the prevalence of anxiety and depression was 24.94 and 24.83%, respectively, while another meta-analysis (6) evaluated the same prevalence in designated hospitals during the COVID-19 period, which was 44 and 31%, respectively. However, there has been no meta-analysis of such prevalence among frontline healthcare workers since the COVID-19 outbreak. Therefore, this study focused on the prevalence of anxiety and depression among frontline healthcare workers.
According to other studies, differences in gender and occupation may affect the prevalence of anxiety and depression (14). Based on these two possible factors, this study adds other potential factors to the analysis. The aim was to obtain additional results to provide a reference for subsequent targeted interventions.
This study systematically evaluated the risk of anxiety and depression among frontline healthcare workers during the COVID-19 pandemic. We further explored the possible potential influencing factors. The results can guide the the allocation of mental health services for healthcare workers and the implementation of targeted interventions. Thereby, reducing the prevalence of anxiety and depression amid the COVID-19 pandemic.
Materials and methods
Search strategy
A computer search of the CNKI, VIP, WanFang Data, and PubMed databases collected cross-sectional studies on the prevalence of anxiety and depression among frontline healthcare workers since the onset of COVID-19. The search period was limited to December 2019 to April 2022. A combination of subject headings and free words were used to search, and the search terms included COVID-19, anxiety, depression, healthcare workers, etc.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) research objects: frontline healthcare workers since the onset of COVID-19, (2) type of research: cross-sectional study, (3) research outcome: sample size and prevalence of anxiety and depression; and (4) language: Chinese or English. The exclusion criteria were as follows: (1) the research subject is part of other hospital populations, including non-frontline healthcare workers, administrative staff, interns, patients, and infected healthcare workers, (2) the same research or literature published repeatedly, (3) incorrect or incomplete data or inability to extract or convert required data, (4) lack of measurement tools featuring good reliability and validity used in assessing anxiety and depression; and (5) the research period did not coincide with the COVID-19 pandemic.
Data extraction
Literature screening, data extraction, and cross-checking were performed independently by two trained researchers. Disagreements and doubts were resolved through three or more collective discussions or by consulting third-party experts. By reading the titles and abstracts, the literature that did not meet the requirements was initially excluded, and then the full texts of the remaining literature were read to determine whether they met the inclusion criteria. If the data were incomplete, we contacted the authors to obtain complete data. The extracted data mainly included the following: (1) basic information of the included studies, including the title, first author, time, and region of the study, (2) general information of the research subjects: sample size, age, sex, etc., (3) outcome indicators and outcome measurement data; and (4) key elements required for quality evaluation.
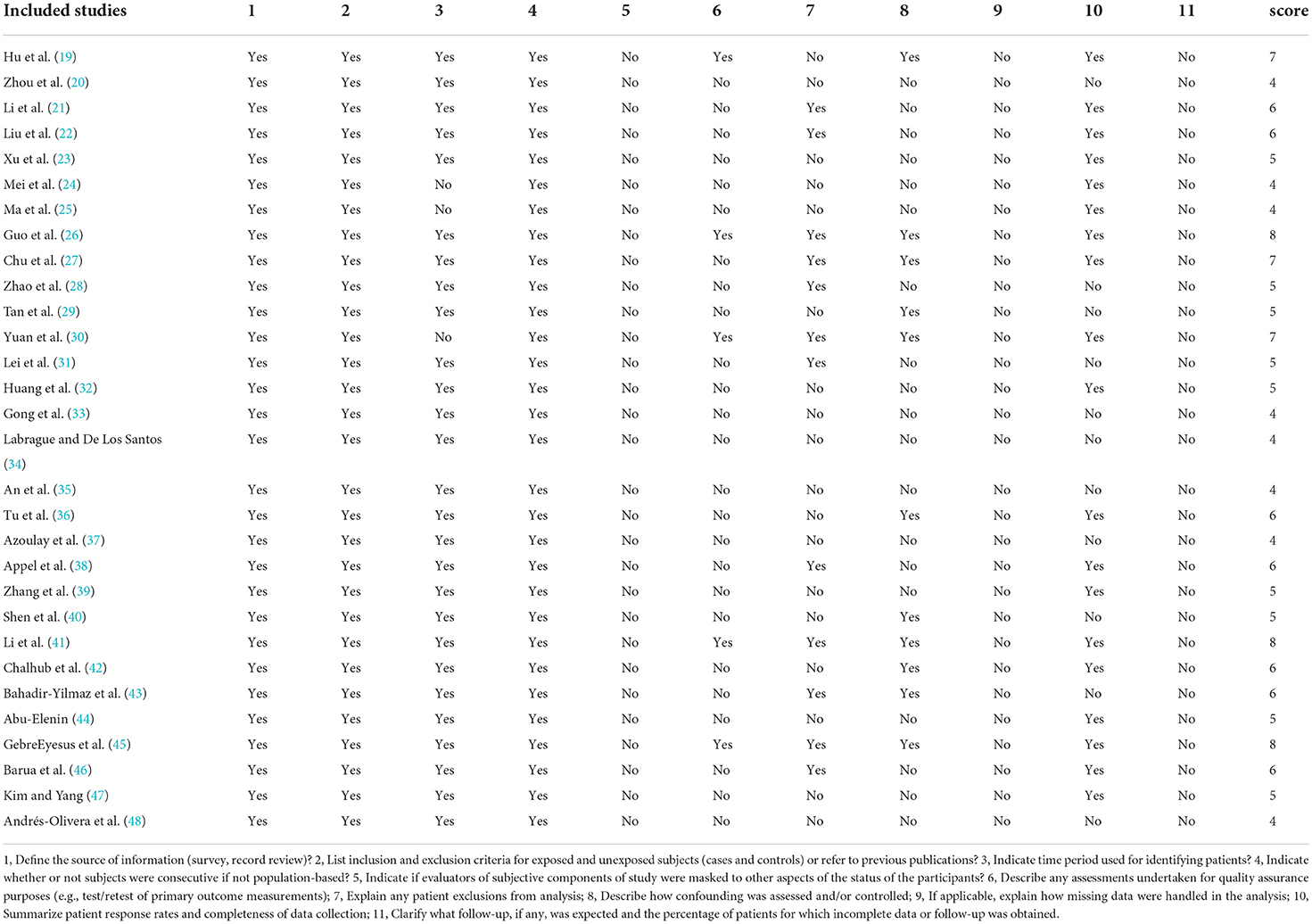
Quality evaluation
The American Agency for Healthcare Research and Quality recommends quality evaluation standards for observational studies. The labels recommended for evaluating cross-sectional studies include 11 items, with responses “yes,” “no,” and “not reported” respectively. Only the answer “yes” scored 1, while “no” and “not reported” scored 0. Scores of 8–11 were regarded as high quality and 4–7 as moderate quality (15). Two researchers independently evaluated and cross-checked the quality of the included studies. In cases of disagreement, a third party was requested to assist in the discussion.
Statistical methods
Meta-analysis was performed on the collected data using STATA 15.1 software; the prevalence of anxiety and depression and their 95% confidence interval (CI) were used as statistical effect sizes. The χ2 test (test level: α = 0.1) was used to analyze the heterogeneity among the results of the included studies, and the size of the heterogeneity was judged in combination with I2. Different heterogeneity models were used: (1) when I2 <50% and P > 0.10, the study was considered to be homogeneous, and the fixed effect model was used, (2) when I2 ≥ 50% and P ≤ 0.10, the study was considered to be heterogeneous, and a random effect model was used (16). Publication bias was detected using Egger's method. Publication bias refers to the fact that statistically significant research findings are more likely to be reported and published than non-significant and invalid findings (17). The stability and accuracy of the analysis results were evaluated using sensitivity analysis. It was used to assess the reliability of the meta-analysis results, focusing on study characteristics (such as the level of methodological quality). We excluded low-quality studies or adopted different efficacy evaluation standards and statistical methods to explore their influence on the combined effect size. The focus was on the comparison of the pooled effect sizes from repeated meta-analyses with the original effect sizes (18). P < 0.05 indicated that the difference was statistically significant.
Results
Selection of studies
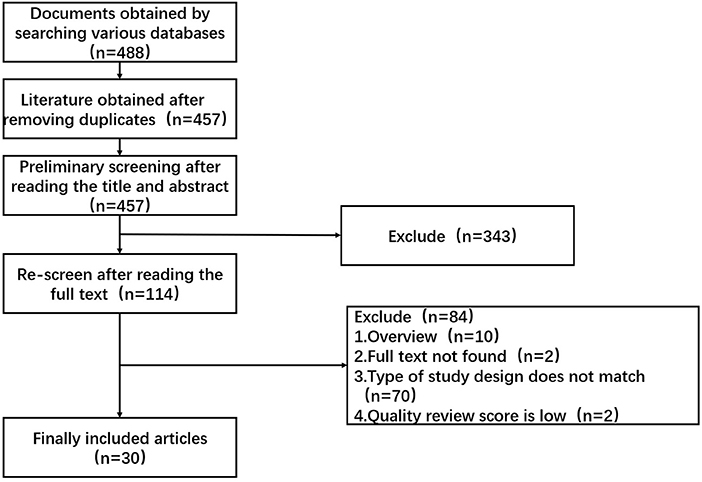
A total of 488 relevant studies were initially screened; after screening according to the inclusion and exclusion criteria, 30 studies were finally included (19–48). The literature screening process is illustrated in Figure 1.
Basic characteristics
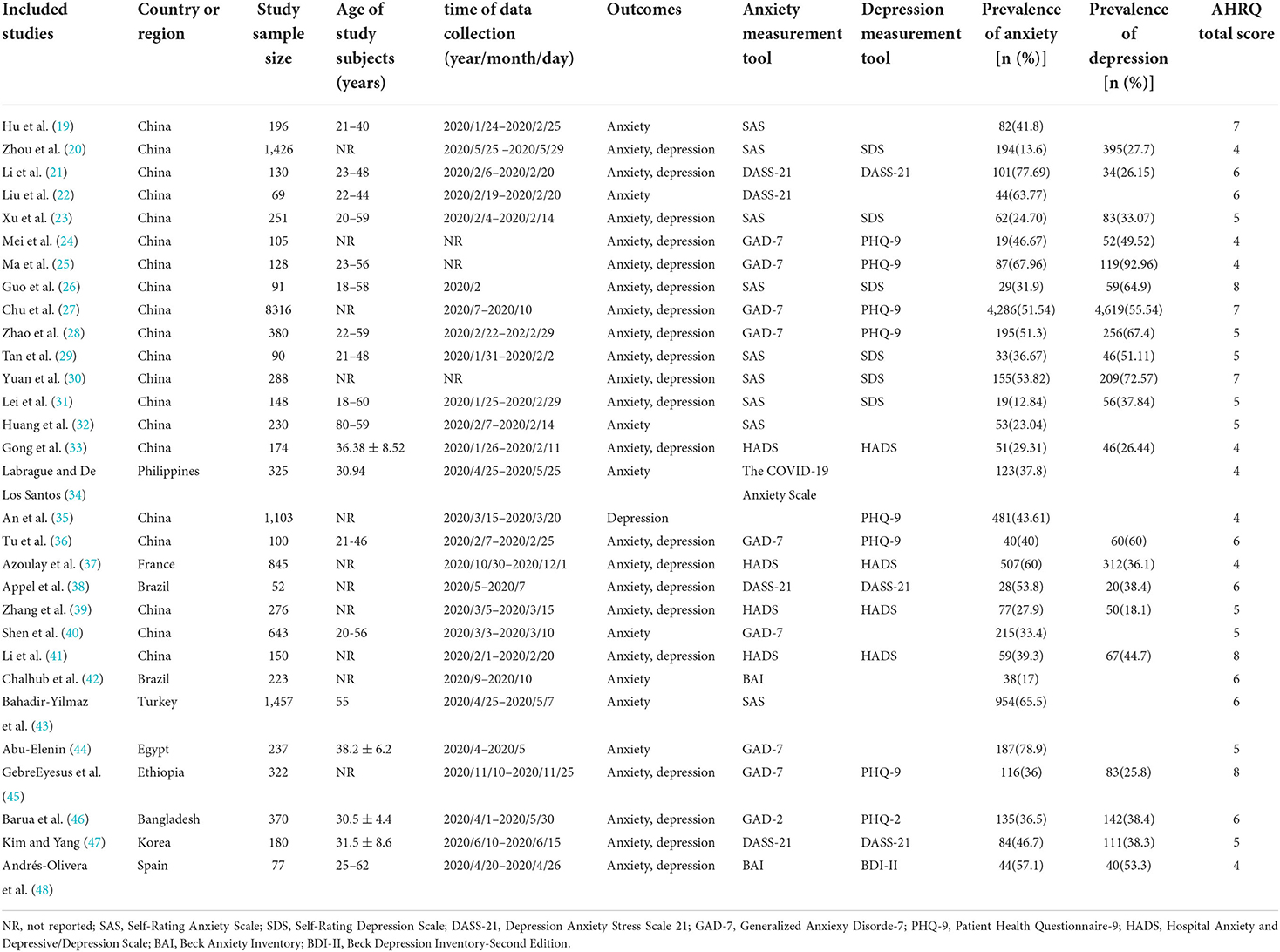
The basic characteristics of the included studies are presented in Table 1. The quality evaluation results showed that all included studies were of medium quality and above, including 3 high-quality articles and 27 medium-quality articles. Further details are provided in Table 2.
Meta-analysis results
Prevalence of anxiety
A total of 29 studies (19–34, 36–48) reported the prevalence of anxiety among frontline healthcare workers. The results showed that the overall prevalence of anxiety was 0.43, with a 95% CI (0.36, 0.50), P < 0.001. The results of subgroup analysis showed that among frontline healthcare workers, females [0.38, 95% CI (0.29, 0.48), P < 0.001], married individuals [0.39, 95% CI (0.26, 0.52), P < 0.001], those with children [0.51, 95% CI (0.47, 0.55), P < 0.001], those with a bachelor's degree or below [0.37, 95% CI (0.26, 0.48), P < 0.001], intermediate and above professional title [0.37, 95% CI (0.23, 0.52), P < 0.001], and nurses [0.45, 95% CI (0.32, 0.59), P < 0.001] had a higher prevalence of anxiety. Further details are provided in Table 3.
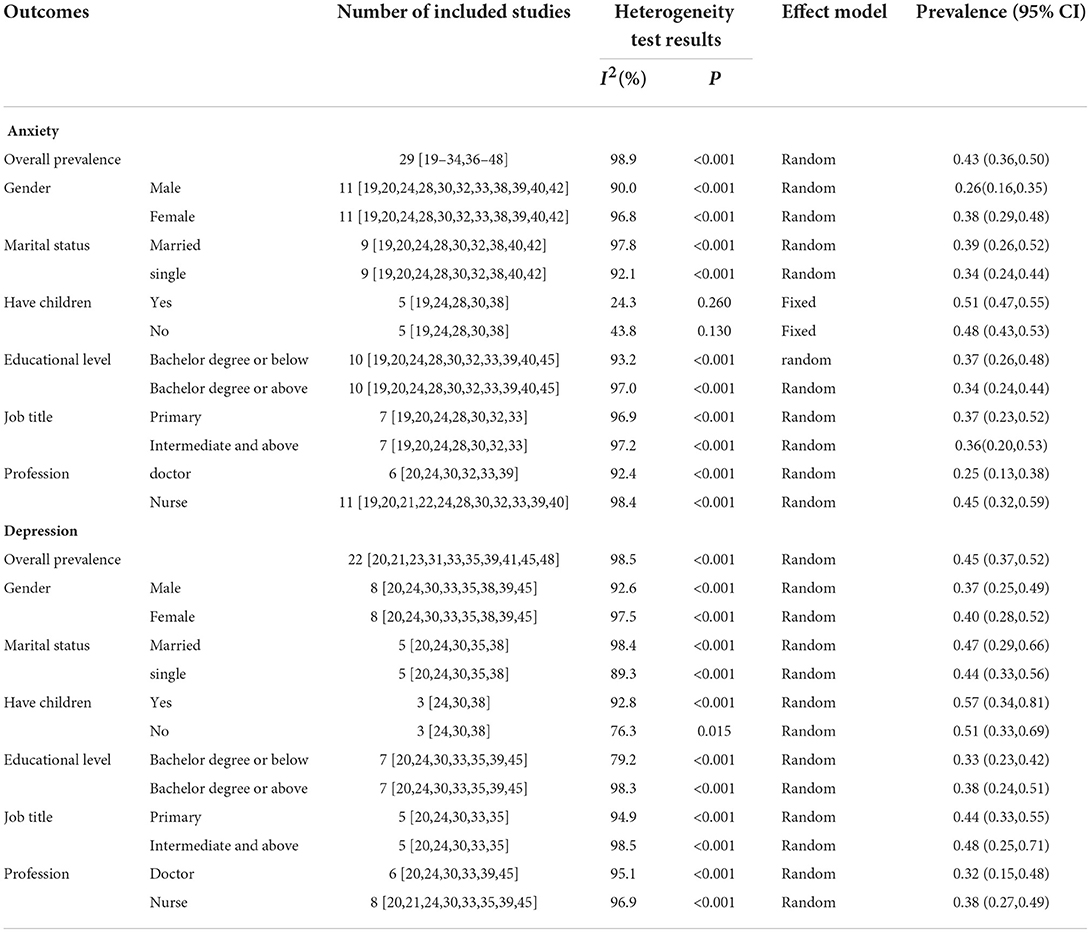
Table 3. Meta-analysis results of anxiety and depression among frontline healthcare workers during COVID-19.
Prevalence of depression
A total of 22 studies (20, 21, 23–31, 35–39, 41, 45–48) reported the prevalence of depression among frontline healthcare workers. The results showed that the overall prevalence of depression was 0.45, with a 95% CI (0.37, 0.52), P < 0.001. The results of subgroup analysis showed that among frontline healthcare workers, females [0.40, 95% CI (0.28, 0.52), P < 0.001], married individuals [0.47, 95% CI (0.29, 0.66), P < 0.001], those with children [0.57, 95% CI (0.34, 0.81), P < 0.001], those with a bachelor's degree or above [0.38, 95% CI (0.24, 0.51), P < 0.001], intermediate and above professional title [0.48, 95% CI (0.25, 0.71), P < 0.001], and nurses [0.38, 95% CI (0.27, 0.49), P < 0.001] had a higher prevalence of depression. Further details are provided in Table 3.
Sensitivity analysis
Sensitivity analysis was carried out by excluding the included studies individually. It was found that the prevalence of anxiety was 35–52%, and the prevalence of depression was 36–54%; the gap was not large compared to the overall prevalence rate. This suggests that the results of this study were stable.
Publication bias analysis
The Egger test was used to evaluate publication bias, and the results showed that anxiety (P = 0.661) and depression (P = 0.266) all indicated that the possibility of publication bias was small.
Discussion
Anxiety and depression are common but easily overlooked diseases (49). If patients with anxiety and depression are not properly treated, their quality of life may be affected. This study systematically evaluated the prevalence of anxiety and depression among frontline healthcare workers since the onset of COVID-19, which can be used to evaluate the impact of COVID-19 on their mental health. The results of the meta-analysis showed that the total prevalence of anxiety among frontline healthcare workers was 43% and the total prevalence of depression was 45%. The results of subgroup analysis showed that the prevalence of anxiety and depression in women, married individuals, those with children, and nurses was relatively high; the prevalence of anxiety was higher in those with a bachelor's degree or below, and the prevalence of depression was higher among those with intermediate professional titles and above.
This study reported that the overall prevalence of anxiety and depression among frontline healthcare workers during the COVID-19 pandemic was 43 and 45%, respectively, which was higher than the prevalence of anxiety (31.9%) and depression (33.7%) in the general population during the COVID-19 pandemic reported by Marvaldi et al. (50), which was also higher than the prevalence of anxiety (24.94%) and depression (24.83%) among healthcare workers during the COVID-19 pandemic reported by Sahebi et al. (13). In the early stages of the virus outbreak, lack of experience, and anti-pandemic materials, as well as long-term high-intensity work, may have caused higher rates of anxiety and depression among frontline healthcare workers than among the general population and healthcare workers. Simultaneously, frontline healthcare workers have a higher risk of infection, and the serious consequences of infection usually make people feel nervous and frightened. The physical and mental health of frontline healthcare workers becomes impaired, which in turn induces anxiety and depression. Lai et al. (51) also showed that the front-line work environment increases the risk of psychological problems for healthcare workers. Mental health quality levels should be properly assessed when selecting frontline healthcare workers. In addition, an existing study (52) found that direct exposure to COVID-19 also affected frontline healthcare workers' sleep quality. Good sleep quality protects against anxiety and depression. Therefore, providing adequate protective equipment and psychological support to frontline healthcare workers can improve their resilience. This will effectively reduce the risk of anxiety and depression, improve work status and efficiency, and provide favorable conditions for better anti-pandemic work. The prevalence of anxiety and depression has decreased with the normalization of infection prevention and control measures (53). Poor mental health can still have a negative impact on frontline healthcare workers. Therefore, it is necessary to regularly monitor the potential risks of anxiety and depression among frontline healthcare workers. This also provides effective interventions to improve their poor state, thereby reducing the related negative effects.
The results of the subgroup analysis showed that the prevalence of anxiety and depression was relatively high among women and nurses, which is consistent with the previous findings of Pappa (14). Previous studies (54) have shown that women are more likely to develop psychological disorders than men, which may be related to physiological factors such as hormone levels (55). Under normal circumstances, women's physical strength is not as great as that of men. When facing a long-term high-intensity workload, they may develop conflicted psychology, which may induce psychological problems, such as anxiety and depression. The prevalence of anxiety and depression among nurses is higher than that among doctors, which may be influenced by the fact that the majority of nurses are female. In addition, nurses spend more time in the ward providing direct care to patients than doctors and are more at risk of contracting the virus than doctors, so they are more prone to psychological problems. The prevalence of anxiety and depression among frontline healthcare workers who are married or have children is higher, which may be related to family burden (56). Owing to the special nature of their work, frontline healthcare workers may not be able to obtain information about their family members in a timely manner. Concerns about family cause them to devote part of their energy to worrying about the safety of their family members; therefore, psychological problems such as anxiety and depression may be more likely to occur.
This study's results are inconsistent regarding academic qualifications and professional titles. Changes in academic qualifications and professional titles had different effects on the prevalence of anxiety and depression, and further research is required. However, other studies (6) have proved that healthcare workers with lower professional titles and higher education have higher prevalence rates of anxiety and depression than those with higher professional titles and lower education, which provides a reference. Owing to the differences in the prevalence of anxiety and depression in different populations, we should formulate and provide corresponding preventive and intervention measures according to different types of needs.
This study has some limitations. First, the included studies were all cross-sectional, and some studies had small sample sizes. Second, the included studies were heterogeneous. Third, the number of included studies in some subgroups was small, which may have affected the results' accuracy to some extent.
In summary, since the onset of COVID-19, the prevalence of anxiety and depression among frontline healthcare workers has been relatively high, with obvious population differences. This group remains on the front line of the fight against the pandemic, and faces constant psychological pressure; therefore, attention should be paid to the anxiety and depression screening of frontline healthcare workers. Targeted measures should be taken to provide professional psychological intervention when necessary. Greater attention must now be paid to developing and evaluating the effectiveness of different interventions and initiatives to support the mental health of healthcare Workers during this pandemic (57). Simultaneously, domestic and international healthcare authorities and policymakers should take steps to reduce these mental illnesses among frontline healthcare workers. This could improve the efficiency of the hospital staff, accelerate pandemic control, and provide more effective treatments for COVID-19 patients.
Improving the medical security system, formulating targeted intervention measures, strengthening the training of healthcare workers, and providing professional psychological counseling can help improve mental health and avoid the emergence of serious psychological problems, such as anxiety and depression.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession numbers can be found in the article/supplementary materials.
Author contributions
YuC conceived and designed the study and wrote the paper. YuC and JW collected data and conducted the follow-up work. YuC and YG performed the statistical analysis. ZF and LZ conducted the format and tables. YanC and YY directed the conduct of the study. All authors have read and approved the final manuscript.
Funding
This work was supported by the Fifth Batch of Talents Selected under the Special Support Plan in Anhui Provence (Organization Department of Anhui Provincial Party Committee [2019] No. 14; T000516), Major Natural Science Research Projects in Universities of Anhui Province (No. KJ2020ZD69), and Anhui Province Social Science Innovation and Development Research Project (2021CX105).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sohrabi C, Alsafi Z, O'neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.02.034
2. Liu C, Chen LJ, Zeng Y, Cai WP, Guo Y, Li LH. Mental health status among people living with HIV in Guangzhou during the COVID-19 outbreak. Chin J AIDS STD. (2021) 27:1263–7. doi: 10.13419/j.cnki.aids.2021.11.15
3. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A Nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
4. Heitzman J. Impact of COVID-19 pandemic on mental health. Psychiatr Pol. (2020) 54:187–98. doi: 10.12740/PP/120373
5. Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 13:132–7. doi: 10.1016/j.jpsychires.2020.09.007
6. Liu XY, Wang GP, Zhang J, Wang SH. Prevalence of depression and anxiety among health care workers in designated hospitals during the COVID-19 epidemic: a meta-analysis. Chin J Evidence-Based Med. (2021) 21:1035–42. doi: 10.1186/s12888-021-03459-w
7. Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain. Behav Immun. (2020) 87:23–4. doi: 10.1016/j.bbi.2020.03.032
8. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732–8. doi: 10.7150/ijbs.45120
9. Zhang Y, Bao X, Yan J, Miao H, Guo C. Anxiety and depression in chinese students during the COVID-19 pandemic: a meta-analysis. Front Public Health. (2021) 9:697642. doi: 10.3389/fpubh.2021.697642
10. Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): a systematic review with meta-analysis. PLoS ONE. (2016) 11:e0155431. doi: 10.1371/journal.pone.0155431
11. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
12. Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. (2012) 53:15–23. doi: 10.1016/j.comppsych.2011.02.003
13. Sahebi A, Nejati-zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
14. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
15. Zeng XT, Liu H, Chen X, Leng WD. Meta-analysis series four: quality assessment tools for observational studies. Chin J Evidence-Based Cardiovascular Med. (2012) 4:297–9. doi: 10.3969/j.1674-4055.2012.04.004
16. Lee KW, Ching SM, Ramachandran V, Yee A, Hoo FK, Chia YC, et al. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2018) 18:494. doi: 10.1186/s12884-018-2131-4
17. Chen X. Investigation and reflection on publication bias of medical journals in China. Chin J Sci Tech Periodicals. (2019) 30:715–20. doi: 10.11946/cjstp.201902260126
18. Zhang S. Subgroup analysis and sensitive analysis should be set up reasonably in Meta?analysis. Chin J Contemporary Neurol Neurosurg. (2016) 16:1–2. doi: 10.3969/j.issn.1672?6731.2016.01.001
19. Hu J, Li Y, Li WW, Zhang JX. Anxiety status and its influencing factors of nurses fighting COVID-19. Chin Tropical Med. (2020) 20:1188–92. doi: 10.13604/j.cnki.46-1064/r.2020.12.15
20. Zhou XP, Huang JZ, Ren AK, Luo TD, Han MF, Ma HQ. Psychological coping ability of 1426 health care workers participating in first-line anti-epidemic of COVID-19 in a city. Chin J Infect Control. (2021) 20:320–6. doi: 10.12138/j.issn.1671-9638.20216699
21. Li Z, Shi HR, Chen JF, Shi YF, Feng LH, Cui YY, et al. Investigation and analysis on the mental health status and coping style of first-line nurses of Shanxi Province During the outbreak of COVID-19. J Changzhi Med College. (2020) 34:87–91.
22. Liu JR, Shi CQ, Wang N. A study on the psychological status of frontline nurses in sudden public health incidents. Psychol Monthly. (2021) 16:85–87+95. doi: 10.19738/j.cnki.psy.2021.20.028
23. Xu S, Wu JJ, Xu C, Peng L, Li Y, Li M. Survey of mental health status of first - line healthcare workers in designated hospitals for COVID-19 in Wuhan. J Army Med Univer. (2020) 42:1830–5. doi: 10.16016/j.1000-5404.202003221
24. Mei L, Mei P, Li Q. Investigation on the mental state and coping methods of the first batch of front-line medical staff under the new crown pneumonia epidemic. J Qilu Nurs. (2020) 26:40–3. doi: 10.3969/j.issn.1006-7256.2020.13.011
25. Ma Mf, Xiao J, Xin X. Analysis and coping strategies of mental health status of first - line medical staff under COVID-19. Chin Med Ethics. (2021) 34:496–500. doi: 10.12026/j.issn.1001-8565.2021.04.17
26. Guo XD, Liu ZH, Yu KH, Zhang H. The study on the status and influencing factors of depression,anxiety and irritability in high-risk medical staff working at the frontline against the Pneumonia infected by 2019-nCoV. Modern Nurse. (2022) 29:32–7. doi: 10.19791/j.cnki.1006-6411.2022.07.008
27. Chu JX, Xu L, Feng XY, Xiong Z. Influence of COVID-19 epidemic on psychology and physical health of medical staff in Tianjin. Occupation and Health. (2022) 38:640–4. doi: 10.13329/j.cnki.zyyjk.2022.0097
28. Zhao YP, Yan XW. Investigation on status and influencing factors of anxiety of nurses from high-risk departments during pandemic period of novel coronavirus pneumonia. Henan J Prevent Med. (2020) 31:561–66. doi: 10.13515/j.cnki.hnjpm.1006-8414.2020.08.001
29. Tan J, Guo LH, Feng SP, Wen Q, Tian F. Correlation between psychological resilience and anxiety depression of the medical staffs in the fight against Novel coronavirus pneumonia. Modern Nurse. (2021) 28:30–4. doi: 10.19792/j.cnki.1006-6411.2021.11.010
30. Yuan J, Chen YM, Mou XH, Qi DP, Min WJ, Zhou Y, et al. Study of anxiety and depression levels and their influencing factors in medical staff working in anti-Covid-19 front line. J Huaihai Med. (2021) 39:132–7. doi: 10.14126/j.cnki.1008-7044.2021.02.007
31. Lei Y, Wang N, Zhai H. Analysis of the psychological status of medical staff in the centralized medical observation point of new coronary pneumonia. J Modern Med Health. (2021) 37:1600–3. doi: 10.3969/j.issn.1009-5519.2021.09.051
32. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in designated hospitals for novel coronavirus pneumonia. Chin J Industrial Hygiene Occupational Dis. (2020) 3:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063
33. Gong L, Li CJ, Wang H, Feng K. Investigation on anxiety and depression of first-line medical staff in designated hospitals under COVID-19 epidemic situation. Word Latest Med Informa. (2021) 21:309–11. doi: 10.3969/j.issn.1671-3141.2021.25.136
34. Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J Nurs Manag. (2020) 28:1653–61. doi: 10.1111/jonm.13121
35. An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. (2020) 276:312–5. doi: 10.1016/j.jad.2020.06.047
36. Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine (Baltimore). (2020) 99:e20769. doi: 10.1097/MD.0000000000020769
37. Azoulay E, Pochard F, Reignier J, Argaud L, Bruneel F, Courbon P, et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave a cross-sectional study. Chest. (2021) 160:944–5. doi: 10.1016/j.chest.2021.05.023
38. Appel AP, Carvalho A, Santos RPD. Prevalence and factors associated with anxiety, depression and stress in a COVID-19 nursing team. Rev Gaucha Enferm. (2021) 42:e20200403. doi: 10.1590/1983-1447.2021.20200403
39. Zhang XB, Xiao W, Lei J, Li MX, Wang X, Hong YJ, et al. Prevalence and influencing factors of anxiety and depression symptoms among the first-line medical staff in Wuhan mobile cabin hospital during the COVID-19 epidemic: a cross-sectional survey. Medicine (Baltimore). (2021) 100:e25945. doi: 10.1097/MD.0000000000025945
40. Shen Y, Zhan Y, Zheng H, Liu H, Wan Y, Zhou W. Anxiety and its association with perceived stress and insomnia among nurses fighting against COVID-19 in Wuhan: A cross-sectional survey. J Clin Nurs. (2021) 30:2654–64. doi: 10.1111/jocn.15678
41. Li L, Sun N, Fei S, Yu L, Chen S, Yang S, et al. Current status of and factors influencing anxiety and depression in front-line medical staff supporting Wuhan in containing the novel coronavirus pneumonia epidemic. Jpn J Nurs Sci. (2021) 18:e12398. doi: 10.1111/jjns.12398
42. Chalhub RA, Menezes MS, Aguiar CVN, Santos-Lins LS, Netto EM, Brites C, et al. Anxiety, health-related quality of life, and symptoms of burnout in frontline physicians during the COVID-19 pandemic. Braz J Infect Dis. (2021) 25:101618. doi: 10.1016/j.bjid.2021.101618
43. Bahadir-Yilmaz E, Yuksel A. State anxiety levels of nurses providing care to patients with COVID-19 in Turkey. Perspect Psychiatr Care. (2021) 57:1088–94. doi: 10.1111/ppc.12661
44. Abu-Elenin MM. Immediate psychological outcomes associated with COVID-19 pandemic in frontline physicians: a cross-sectional study in Egypt. BMC Psychiatry. (2021) 21:215. doi: 10.1186/s12888-021-03225-y
45. Gebreeyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PLoS ONE. (2021) 16:e0259906. doi: 10.1371/journal.pone.0259906
46. Barua L, Zaman MS, Omi FR, Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Res. (2020) 9:1304. doi: 10.12688/f1000research.27189.2
47. Kim MY, Yang YY. Mental health status and its influencing factors: the case of nurses working in COVID-19 Hospitals in South Korea. Int J Environ Res Public Health. (2021) 18: e18126531. doi: 10.3390/ijerph18126531
48. Andrés-Olivera P, García-Aparicio J, Lozano López MT, Benito Sánchez JA, Martín C, Maciá-Casas A, et al. Impact on sleep quality, mood, anxiety, and personal satisfaction of doctors assigned to COVID-19 Units. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph19052712
49. Tao JQ, Gong JR, Lu JY, Liang LY, Liao XM. Meta—analysis on the prevalence of depressive and /or anxiety disorder in general hospitals in China. Sichuan Menta Health. (2018) 31:73–8. doi: 10.11886/j.issn.1007-3256.2018.01.018
50. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
51. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al Factors associated with mental health outcomes among health care workers exposed to coronavirus Disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
52. Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. (2020) 70:124. doi: 10.1016/j.sleep.2020.04.019
53. Zhang ZS, Zou SM, Wang M, Li CL. Investigation and analysis of mental health status of medical staff in designated hospitals during COVID-19 normalized epidemic prevention and control. Psychological Monthly. (2020) 15:54–5. doi: 10.19738/j.cnki.psy.2020.18.020
54. Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. (2017) 4:146–58. doi: 10.1016/S2215-0366(16)30263-2
55. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
56. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 Epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
Keywords: COVID-19, frontline healthcare workers, anxiety, depression, prevalence, meta-analysis
Citation: Chen Y, Wang J, Geng Y, Fang Z, Zhu L, Chen Y and Yao Y (2022) Meta-analysis of the prevalence of anxiety and depression among frontline healthcare workers during the COVID-19 pandemic. Front. Public Health 10:984630. doi: 10.3389/fpubh.2022.984630
Received: 02 July 2022; Accepted: 15 August 2022;
Published: 13 September 2022.
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Sarvodaya Tripathy, Independent Researcher, Lucknow, IndiaKun-Shan Wu, Tamkang University, Taiwan
Copyright © 2022 Chen, Wang, Geng, Fang, Zhu, Chen and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Chen, chenyan2010@wnmc.edu.cn; Yingshui Yao, yingshuiyao@163.com
 Yu Chen
Yu Chen Jing Wang
Jing Wang Yujie Geng2
Yujie Geng2 Yan Chen
Yan Chen