Abstract
The COVID-19 pandemic presents significant risks to population mental health. Despite evidence of detrimental effects for adults, there has been limited examination of the impact of COVID-19 on parents and children specifically. We aim to examine patterns of parent and child (0–18 years) mental health, parent substance use, couple conflict, parenting practices, and family functioning during COVID-19, compared to pre-pandemic data, and to identify families most at risk of poor outcomes according to pre-existing demographic and individual factors, and COVID-19 stressors. Participants were Australian mothers (81%) and fathers aged 18 years and over who were parents of a child 0–18 years (N = 2365). Parents completed an online self-report survey during ‘stage three’ COVID-19 restrictions in April 2020. Data were compared to pre-pandemic data from four Australian population-based cohorts. Compared to pre-pandemic estimates, during the pandemic period parents reported higher rates of parent depression, anxiety, and stress (Cohen’s d = 0.26–0.81, all p < 0.001), higher parenting irritability (d = 0.17–0.46, all p < 0.001), lower family positive expressiveness (d = − 0.18, p < 0.001), and higher alcohol consumption (22% vs 12% drinking four or more days per week, p < 0.001). In multivariable analyses, we consistently found that younger parent age, increased financial deprivation, pre-existing parent and child physical and mental health conditions, COVID-19 psychological and environmental stressors, and housing dissatisfaction were associated with worse parent and child functioning and more strained family relationships. Our data suggest wide-ranging, detrimental family impacts associated with the COVID-19 pandemic; and support policy actions to assist families with financial supports, leave entitlements, and social housing.
Similar content being viewed by others
Introduction
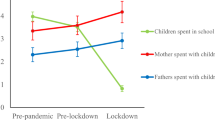
To curb rates of COVID-19 infection in early 2020, many countries adopted social distancing policies. In April 2020, Australia implemented a national lockdown, requiring people to stay at home except for four reasons: essential shopping, caregiving, exercise, and/or permissible work or study [1]. The lockdown was accompanied by a rapid elevation in job loss and unemployment, with two-thirds of Australians having their employment affected [2]. The lockdown also meant that children were unable to access playgrounds, campus-based schooling, and wider social supports, all of which have potential for deleterious effects on child and parent mental health and wellbeing [3]. Early evidence describing the impact of the pandemic has indicated increased rates of family violence and mental health problems in Australia [4, 5] and internationally [6,7,8,9], but to-date, data investigating the mental health outcomes for parents and children specifically has been limited. The current study compares to pre-pandemic Australian data to provide a snapshot of parent and child mental health, parent substance use, couple conflict, parenting, and family functioning, as reported by 2365 Australian parents of a child 0–18 years during the pandemic in April 2020; and seeks to identify families at higher risk of poor outcomes [10].
COVID-19 and increased mental health risks
The COVID-19 pandemic has been associated with increased psychiatric morbidity in adults around the world [8, 9, 11,12,13,14], and also in Australia, specifically [4, 15]. Australian data have shown that approximately one-third of adults were consuming more alcohol during the pandemic [16] and that adults caring for dependent family members were more likely than non-parents to report mental health symptoms in April 2020 [15]. Despite this increased risk to mental health, there is limited research focused specifically on parents’ mental health and wellbeing. Evidence from around the world shows increased rates of child mental health problems in the context of the COVID-19 pandemic [17,18,19,20,21].
COVID-19 and family functioning
The COVID-19 pandemic has exacerbated traditional drivers of parenting stress and couple conflict. A Singaporean study demonstrated concurrent links between work-family conflict and higher levels of parenting stress and couple conflict in parents juggling work while supervising children during lockdown [22]. Spanish data show links between higher levels of parenting distress, less structured parenting, and child mental health problems, in context of strict COVID-19 lockdowns [23]. A study in the USA showed that higher parent anxiety and depression symptoms during the pandemic were associated with higher concurrent parent stress and child abuse potential [24], and a large Canadian study showed that parent depression, number of children, unmet childcare needs, and relationship distress predicted lower-quality parenting [25]. However, these studies examined associations at the time of the pandemic, and did not estimate whether there were changes in family functioning prior to, compared to during, the pandemic.
Pre-existing and COVID-19 related risk factors
Consistent evidence shows that adults experiencing pre-existing socio-economic disadvantage face increased mental health problems related to COVID-19 [5, 19, 20, 26], but to-date, studies focused specifically on child and family outcomes have not investigated the impact of socio-economic inequities. Persistent or acute stressors arising from the COVID-19 pandemic may also amplify distress, including environmental factors, such as job loss, financial insecurity, changes to employment, COVID-19 diagnosis, illness, or hospitalization [22, 26]; psychological factors, such as worry/concern versus optimism about the virus [18, 19, 22, 26,27,28]; and frequency of news media access across different sources [18, 29].
Pre-existing individual factors, such as poorer physical health, a history of chronic illness, or pre-existing mental health problems, have been associated with higher rates of anxiety and depression during COVID-19 [18, 30]. Other individual factors may be important too. For example, introverted individuals are somewhat less likely to have high quality social support systems compared to extraverts [31]. Further, children with neurodevelopmental conditions, such as Attention-Deficit/Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD), may experience symptom deterioration and other adverse mental health outcomes during the pandemic [32,33,34]. Research has yet to comprehensively examine how pre-existing neurodevelopmental conditions are associated with family functioning across multiple domains during the pandemic.
The unique context of COVID-19 distancing restrictions has forced families to spend more time at home and confined to their suburb than usual. Housing is a key determinant of health, and a variety of housing characteristics are associated with poorer parent and child mental health outcomes and/or poorer family functioning, including tenure, i.e., whether families are renting [35], housing type [36], overcrowding [37], availability and size of private outdoor space [38], and satisfaction with housing [39]. It is important to understand whether these housing factors play a role in how families adjust to social distancing restrictions.
The psychological aftermath of the pandemic is likely to be greater for families with pre-existing socio-economic or individual risks, or those experiencing COVID-19 related risk factors. Identifying risk factors is key to providing targeted prevention and intervention approaches in the context of broader population-level care. However, to-date, very few studies have investigated the full breadth of these factors collectively to determine the relative contribution of each risk factor; and internationally, there is little known about these risks and vulnerabilities specifically in regard to parent, child, and family outcomes. Heightened parent or child vulnerability may have cascading effects within families, with potential for direct and indirect effects on couple relationships and parent–child dynamics. Thus, our study investigates the impact of COVID-19 on the health and wellbeing of parents, children, and families, and identifies risk factors that are associated with poorer outcomes in the context of large-scale public health crises.
Specifically, the main aims of this study are three-fold:
-
(1)
To compare parent and child mental health, parent tobacco and alcohol use, couple conflict, parenting practices, and family functioning, in Australian parents of a child 0–18 years during the stage three COVID-19 restrictions in April 2020, with pre-pandemic Australian data.
-
(2)
To examine the extent to which a broad range of pre-existing demographic and socio-economic factors, as well as individual parent and child risk factors (e.g., parent mental health problems, child neurodevelopmental conditions), are associated with parent, child, and family outcomes during the pandemic.
-
(3)
To examine the extent to which COVID-19-related risk factors, including psychological stressors (i.e., attributions and feelings about the pandemic), environmental stressors (i.e., stressful life events), use of news media, having a child at home while working, and housing related factors, are associated with parent, child, and family outcomes during the pandemic.
Method
Design and recruitment
This study uses cross-sectional baseline data from the COVID-19 Pandemic Adjustment Survey (CPAS) [10], a longitudinal study of 2,365 Australian parents of a child 0–18 years. CPAS aims to investigate the impact of the COVID-19 crisis on Australian families via online surveys distributed on a 2–4 weekly basis. Participants were recruited via paid and unpaid social media advertisements using a range of methods to increase the representativeness of the sample. Recruitment occurred over the period 8–28th April, 2020, during a ‘level three’ national lockdown in Australia, requiring that Australians avoid leaving their house except for four reasons: (1) shopping for food and supplies, (2) care and caregiving, (3) exercise, and (4) study or work—if unable to do so from home [1]. Participants were eligible to participate if they resided in Australia and were aged ≥ 18 years, English speaking, and a current parent of a child aged 0–18 years. The study was approved by the Deakin University Human Ethics Advisory Group (HEAG-H 52_2020).
Pre-pandemic Australian datasets
We compared CPAS findings to four studies: (1) Australian published data on parent mental health for 497 parents aged 18–86 years with a dependent child [40]; (2) parent-report of child depression for 349 children aged 12–15 years [41]; (3) baseline data from a subset of Australian parents (N = 1009) from the Child and Parent Emotion Study (CAPES), an age-stratified online sample of parents of children aged 0–9 years, recruited in 2018–2019 [42]; and finally, (4) data from the Longitudinal Study of Australian Children (LSAC), a nationally representative prospective cohort study of Australian children and their families, comprising two cohorts, the Baby Cohort and the Kindergarten Cohort (combined N = 9764) [43, 44]. Ethics approval for CAPES was granted by the Deakin University Human Research Ethics Committee (DUHREC 2018–144; HEAG-H 75_2018). In LSAC, participating children were randomly selected in a two-stage cluster sampling design using Australian postcodes and the Medicare universal healthcare database [43, 44]. We used biennial parent-report data (99% mothers) from three waves of the Baby cohort (N = 5107), covering child ages 0–1 (Wave 1, collected in 2004), 2–3, and 4–5 years; and from five waves of the Kindergarten cohort (4,656), covering child ages 6–7 (Wave 2, collected in 2006), 8–9, 10–11, 12–13, and 14–15 years. LSAC was approved by the Australian Institute of Family Studies Ethics Committee [43, 44].
Measures
See Table 1 for a summary of CPAS study measures.
Population weights
Post-stratification weights in the CPAS dataset were derived to compensate for differences between the final sample and the national subpopulation of Australian adults (i.e., parents of a child 0–18 years, estimated N = 8.4 M) [45]. Weights were produced through a raking approach [46] using six demographic factors: (1) geographic location (major city, inner and outer regional areas, and remote areas); (2) child age-groups (0–4, 5–9, 10–12, 13–14, and 15–18 years); (3) parent gender (male, female); (4) family structure (single parent, couple family); (5) parent high school non-completion (yes/no); and (6) pre-pandemic parent employment (employed, unemployed).
Missing data
Item-level missing data on individual variables was 0–8% in the CPAS study, 0–29% in LSAC, and 0–20% in CAPES. Missing data were replaced using multivariate multiple imputation by chained equations for each study separately. All variables from the final analytic models and weights were included in the multiple imputation model to create 50 imputed datasets. We report pooled results from these multiply imputed datasets.
Data analysis
Analyses were conducted in Stata version 16. To address Aim 1, unweighted descriptive statistics were calculated for each outcome variable in the CPAS and CAPES datasets. For LSAC, descriptive statistics were calculated using all available time-points for each measure and averaged across waves within each imputation model. Estimates were then combined across the Baby and Kindergarten cohorts using a fixed effects meta-analysis with the ‘metafor’ package in R software [47]. We conducted a series of independent samples t tests and chi-squared tests to assess unweighted differences between pre-pandemic data and matched CPAS data. We also conducted a series of sensitivity analyses which: (1) included the full available CPAS dataset (i.e., rather than matching to ages of the comparison study samples); (2) used LSAC Wave 1 and CPAS weights; and (3) excluded high-risk families, including those with a child with ADHD or ASD, and parents with mental health conditions (post hoc analysis).
To address Aims 2 and 3, separate linear regressions were conducted whereby each parent, child, and family outcome was regressed onto risk factors, both in an unadjusted and adjusted (multivariable) model. To aid interpretability, all continuous variables were z score standardized before entry into regression models. In line with Perneger [48], we report results without adjusting for multiple comparisons. Effect size estimates are based on guidelines for population studies [49].
Results
Sample characteristics
Unweighted descriptive statistics for the COVID-19 Pandemic Adjustment Survey (CPAS) sample are presented in Table 2. On average parents were 38 years, children were 9 years. Most participants were cisgender women, and half of children were cisgender girls. Participants were primarily living in major Australian cities and were born in Australia; few participants were Aboriginal or Torres Strait Islander. CPAS had a lower representation of families with a low income, speaking a language other than English, and low education, compared to the Australian population, but had a representative number of single parent families [45]. One-third of parents reported a chronic physical health condition, 40% reported a mental health condition, and 15% had a child with ADHD or ASD. Half the participants had a child at home while working from home.
Comparisons with pre-pandemic Australian data
Table 3 presents comparisons between CPAS parent and child and family outcomes compared to pre-pandemic data. Parents reported higher levels of depression, anxiety, and stress during the pandemic compared to pre-pandemic data. There were no differences between pandemic and pre-pandemic datasets for parent emotion dysregulation or depression in children 12–15 years. However, parents of a child 0–9 years reported higher parenting irritability during the pandemic, compared to CAPES and LSAC pre-pandemic samples. Parents reported more couple conflict during the pandemic compared to LSAC parents, but not compared to CAPES. For children 0–9 years, parents reported lower family positive expressiveness during the pandemic than CAPES parents, but there were no differences in family negative expressiveness. Finally, parents reported higher rates of smoking and alcohol consumption during the pandemic compared to LSAC parents. Sensitivity analyses results are presented in Supplementary Tables 1–3 and were consistent with the primary analyses.
Pre-existing demographic and socio-economic factors
Figure 1 presents a summary of the associations between parent, child, and family outcomes during the pandemic and both pre-pandemic and COVID-19-related risk factors in the adjusted models (for more detail see Supplementary Tables 4–7 for adjusted associations, and Supplementary Tables 8–11 for unadjusted associations).
Regarding demographic factors, we found that women reported somewhat higher levels of anxiety than men, but were much less likely to smoke or consume alcohol at higher levels. Women also were somewhat or moderately more likely to report higher levels of child anxiety, child depression, and family positive expressiveness, than men. There were mixed effects for parent age with small associations between older parent age and lower parent depression, anxiety, stress, emotion dysregulation, and parenting irritability, a very small association with lower family positive expressiveness, and a moderate association with more frequent alcohol consumption. Older child age had small associations with higher parent anxiety and lower child anxiety, and a moderate association with higher levels of smoking. Parents from larger families with more children reported very small/small associations with lower child anxiety, more parenting irritability, and higher levels of family negative expressiveness.
Parents who spoke a language other than English were much more likely to report lower levels of parent alcohol consumption and higher couple conflict, and moderately more likely to report higher parenting irritability. Aboriginal or Torres Strait Islander parents rated themselves much higher on anxiety, and consumed alcohol much less regularly than other parents. Single parents also consumed alcohol much less regularly, were much more likely to smoke, and reported moderately higher child anxiety than other parents. Parents who did not complete high school reported somewhat higher levels of anxiety and were much more likely to smoke. Financial deprivation was consistently associated with poorer functioning, showing small associations with higher parent depression, anxiety, stress, emotion dysregulation, very small associations with child anxiety, couple conflict, and more family negative expressiveness, and moderately large associations with higher levels of parent tobacco smoking. There was also a small association between deprivation and less regular parent alcohol use. Parents in inner regional areas reported lower family positive expressiveness compared to families in major cities.
Pre-existing individual factors
There were very small associations between higher parent introversion (i.e., lower parent extraversion) and higher levels of parent depression, anxiety and emotion dysregulation, child anxiety, and less regular alcohol consumption. Parents with a chronic physical condition reported a very small/small association with higher parent anxiety and stress, and child anxiety, and very large associations with less frequent consumption of alcohol and smoking. Parents with a pre-existing mental health diagnosis reported large/very large associations with higher levels of depression, anxiety, stress, and emotion dysregulation, and small to moderate associations with higher child anxiety and depression, couple conflict, and family negative expressiveness. Parents with a child with ADHD or ASD reported moderate-large associations with higher child anxiety and depression, lower family positive expressiveness/higher negative expressiveness, and higher parenting irritability, and a small association with higher couple conflict.
COVID-19 pandemic stressors
There were small/very small associations between higher reported levels of COVID-19 psychological stressors (i.e., negative attributions and feelings about the pandemic) and a range of outcomes, including higher levels of parent depression, anxiety, stress, emotion dysregulation, child anxiety and depression, higher levels of parenting irritability, and family negative expressiveness. Higher report of COVID-19-related environmental stressors (job loss, employment changes, etc.), had small/very small associations with higher parent depression, anxiety, stress, smoking, emotion dysregulation, higher child anxiety and depression, higher levels of couple conflict, less family positive expressiveness, and more family negative expressiveness. There were very small associations between more frequent use of multiple sources of news media and higher parent anxiety and stress, and higher parenting irritability. Having a child to supervise at home while parents juggled paid work was associated with a mixture of negative outcomes, including small/very small associations with higher parent depression, child anxiety, and parenting irritability, a very large association with a lower likelihood of smoking, and a small association with higher family positive expressiveness.
Regarding housing variables, renting had small associations with higher child depression and lower couple conflict. Although outdoor space was not associated with any outcomes, parents’ level of satisfaction with their home had small/very small protective effects, associated with lower parent depression, anxiety, stress, and emotion dysregulation, lower child depression, parenting irritability, couple conflict, and family negative expressiveness, and higher levels of family positive expressiveness. Finally, there were very small associations between equivalized number of bedrooms and higher levels of parent stress and child depression, and lower levels of family positive expressiveness.
Discussion
Our findings suggest that the COVID-19 pandemic restrictions had wide-ranging, negative impacts for Australian families. Parents participating in the CPAS study had worse functioning across multiple domains compared to Australian pre-pandemic data, including worse parent mental health (i.e., depression, anxiety, and stress) and increased alcohol use. There was also evidence of more strained family relationships, with levels of parenting irritability and couple verbal conflict higher in the CPAS cohort compared to in pre-pandemic data, while family positive expressiveness was lower. Although findings varied depending on the domain examined, we consistently found that younger parent age, increased financial deprivation, pre-existing parent physical and mental health conditions, COVID-19 psychological and environmental stressors, and housing dissatisfaction were associated with worse parent functioning and more strained family relationships. Regarding child mental health, parent pre-existing health conditions and COVID-19 psychological and environmental stressors were consistently associated with higher child anxiety and depressive symptoms, in addition to the child having an ADHD or ASD diagnosis.
COVID-19 and increased mental health risks
Parents in this study had higher levels of depression, anxiety, and stress compared to Australian pre-pandemic data. This is consistent with study findings related to general adult samples [4, 5, 8, 9, 11,12,13,14]. Our findings extend this literature by focusing on parents specifically, by comparing mental health symptoms to pre-pandemic data, and by demonstrating important associations with pandemic stressors. We similarly found that parent alcohol use was higher than pre-pandemic data, consistent with an Australian study of adults [16]. Our finding of lower smoking rates reflect known reductions in tobacco use in the Australian population over time [50], but may also reflect opportunities for smokers to quit. However, we also found that COVID-19 environmental stressors were associated with increased parent smoking. Positively, our analysis suggests few differences in parent emotion regulation between participants in the CPAS study and pre-pandemic data, which may indicate stability in these skills over time.
We compared depressive symptoms in our sample to an Australian study of 349 children aged 12–15 years, and found no differences [41]. However, a number of studies have identified higher mental health difficulties in children and adolescents in the context of COVID-19, although they did not systematically compare to pre-pandemic data [12, 18,19,20, 26, 27, 51, 52]. Our finding may be due to only having a small matched sample (17% aged 12–15 years). Future studies should collect child self-report measures that can be compared to pre-pandemic data, or use prospective designs. Further, except for where we matched to child ages in comparison samples, we examined child outcomes for children 0–18 years. Given considerable differences in child development, as well as differences in the context of parenting infants, young children and adolescents, future research should examine child age effects.
COVID-19 and family functioning
Our findings point to differences in the functioning of families during the pandemic. Higher levels of parenting irritability and lower levels of family positive expressiveness were observed. The evidence for couple verbal conflict was mixed. Minimal differences were evident in the comparison to the CAPES cohort, which was recruited via online methods very similar to the CPAS cohort, and more proximally in time (2018–2019); compared to the LSAC study, collected 2004–2018.
Pre-existing and COVID-19 related risk factors
We found that pre-pandemic financial deprivation was consistently associated with worse parent, child, and family functioning outcomes. Vulnerable families already struggling with socio-economic disadvantage prior to the pandemic were those who suffered most during the pandemic. Geographic remoteness was mostly not associated with outcomes. However, the number of children in the household was somewhat protective for child anxiety symptoms, but was associated with greater parenting irritability, and more negative family expressiveness. It is possible that larger household sizes mitigate some of the negative effects of social isolation, but contribute to greater burden on parents overall, leading to poorer family dynamics. Renting compared to owning a house was associated with higher child depression, and housing dissatisfaction was associated with worse parent functioning and more strained family relationships, in line with previous pandemic [53] and pre-pandemic research [35]. These associations may be due to poorer quality environments in rental homes [54], or perhaps relate to unmeasured socio-economic risk. Housing effects on child outcomes and parent–child relationships have also been shown to be exacerbated by the quantity of time children spend at home [35], which was dramatically increased during the pandemic. Finally, we found that parents living in homes with higher levels of overcrowding reported higher levels of parent stress and child depression, and lower levels of family positive expressiveness, also consistent with pre-pandemic evidence showing associations between crowding and child psychological health [36].
Parents who had a pre-existing mental and/or physical health condition had worse outcomes, consistent with one other COVID-19 study, showing that adults with pre-existing mental health conditions were at greater risk of relapse or new episodes of mental illness [55]. In addition, prior parent mental health difficulties were associated with higher couple conflict and family negative expressiveness. Parents with a prior chronic physical health condition had increased anxiety and stress symptoms, and reported their child as having worse anxiety symptoms.
15% of our sample was reported to have a child with ADHD or ASD. Given that these conditions are associated with increased child and parent mental health symptoms [56, 57], and that these rates appear higher than other Australian population estimates [58, 59], we conducted sensitivity analyses excluding children with ADHD or ASD from the sample. We found that excluding these children had minimal influence on our comparisons to pre-pandemic data. However, we found that having a child with ADHD or ASD was a unique predictor of increased child anxiety and depressive symptoms during the COVID-19 pandemic. This is consistent with pre-pandemic studies that have linked neurodevelopmental conditions such as ADHD and ASD to increased child and depressive symptoms [56, 60]. Similarly, we found that having a child with ADHD and/or ASD was associated with higher levels of parenting irritability, couple conflict, and family positive/negative expressiveness. The associations between ADHD/ASD and more strained family relationships are well-established [57], thus it is unclear whether these findings reflect pre-pandemic patterns or were strengthened during COVID-19.
We consistently found that COVID-19 related psychological and/or environmental stressors were uniquely associated with worse outcomes, with increased risk spanning across most parent, child, and family functioning domains. These findings are consistent with a growing body of research suggesting that COVID-19 related worries and stressors appear to be associated with worse functioning [18,19,20, 27]. Our measure of COVID-19 psychological stress assessed participants’ feelings about being exposed to coronavirus and their ability to cope with COVID-19. Given the association between COVID-19 psychological stress and child mental health, it is possible that children may be attuned to their parents’ concerns. However, it is also possible that this association reflects parents providing severe ratings of child’s symptoms in context of their own symptoms [61]. The collection of child-reported data is important in future research and will address this issue.
Parents who had children at home while they juggled paid work from home reported more strain, including higher parent depression, child anxiety, and parenting irritability. There is a well-established body of longitudinal evidence showing that increases in conflict between parents’ work and family roles lead to parent mental health problems, more irritable parenting, couple conflict, and child mental health problems [62, 63]. During the pandemic, these associations are likely to be compounded by restrictions that prevent children from accessing playgrounds, campus-based schooling, and other social supports.
Recommendations
Overall, this study underscores the importance of considering the mental health of parents and children in the context of the whole family unit. Thus, we consider levers for intervention that are focused on improving both parent and child mental health via providing parents with additional support. Given that the stress and mental health concerns of parents were associated with greater couple conflict and negative family expressiveness, providing programs to vulnerable parents that focus on family relationships may be especially important. There is a wealth of evidence to suggest that strengthening family relationships not only attenuates the negative effects of external stressors and vulnerabilities on relationship outcomes [64], but also can aide in reducing parent and child mental health symptoms [65]. Further, steps to alleviate the stress of working parents are critical, such as dedicated leave entitlements for parents juggling work with home-schooling or caring for children [66], and workplace interventions improving managerial support and flexible work arrangements throughout the pandemic. Given we identified poorer outcomes associated with structural inequalities, our findings support calls for (1) additional financial supports for financially stressed parents during and in the wake of the pandemic [66]; and (2) the need for investment in high quality social housing.
The current study identified an association between parents’ news media consumption, COVID-19 psychological stressors, and mental health problems. Advising parents to avoid news media may be challenging, given their need for social connection during lockdown and the changing public health advice across the pandemic period. Instead, parents could be advised to seek health information directly from government public health sources, thereby reducing exposure to sensationalized or panic-inducing headlines [29]. Parents may also need more support in how to best communicate with their child about the COVID-19 pandemic, as well as about future stressful world events, in a way that provides factual information without increasing worry in children; for example, via short stories or cartoons, such as those used by headtohealth.gov.au.
Strengths and limitations
This study has a number of strengths, including the large, population-weighted sample and the direct comparison to pre-pandemic data via a rigorous meta-analytic approach. Although our measures were brief, we used well-validated tools and examined family functioning across a broad range of domains. There are a number of limitations that also need to be taken into account. For practical reasons, we were unable to collect child-reported data in this study, thus all measures are parent-reported. Our assessment of parent and child mental health problems were based on survey responses, without an objective confirmation from other sources (e.g., from clinical records or direct assessment). Data were cross-sectional, and although they were compared to pre-pandemic samples, the study design was not longitudinal. Our results may have been influenced by underlying differences between the samples rather than purely relating to the impact of the COVID-19 pandemic. Further, we recruited a large sample with the intention of being as population-representative as possible, and examined both population-weighted and unweighted data. Nonetheless, our online-recruited, self-selecting sample had some differences compared to the Australian population, and was not truly representative. The comparisons with a pre-pandemic cohort also recruited online (i.e., minimizing sampling differences) add confidence to our findings. Future longitudinal studies with nationally representative samples are needed to replicate findings. Finally, although fairly evenly spread across age-groups, our numbers of adolescents were lower compared to children aged, and this may limit the generalizability of findings specific to adolescent-aged children. Future research could also compare differences in children versus adolescents.
Concluding comments
Our findings indicate that the COVID-19 pandemic and associated social distancing restrictions in place across Australia in April 2020 were associated with poorer parent and child mental health, and poorer family functioning. We identified several factors connected with poorer outcomes, most notably COVID-19 psychological and environmental stressors, pre-existing health conditions, and pre-existing or COVID-19 related financial deprivation. Our findings build empirical evidence for a number of policy actions to support and protect families from the likely adverse impacts of the pandemic. These include additional financial supports for non-employed and low-income parents, dedicated leave entitlements for parents juggling work with home-schooling or caring for children, and investment in high quality social housing. Our data also support increased investment in evidence-based and flexibly delivered mental health interventions for children and families, targeted to areas of need.
Availability of data and material
On paper acceptance, data will be made available by application to the Australian Data Archive.
Code availability
On paper acceptance, code will be posted to the OSF to the study page https://osf.io/78g5t/.
References
Department of Health. Coronavirus (COVID-19) current situation and case numbers: Australian Government; 2020 Available from: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-current-situation-and-case-numbers
Morgan R, Article No. 8383 (2020) Over two-thirds of working Australians have had their employment impacted by the ‘Coronavirus Crisis’
Leigh-Hunt N, Bagguley D, Bash K et al (2017) An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 152:157–171
Newby J, O’Moore K, Tang S et al (2020) Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 15:e0236562
Fisher JR, Tran TD, Hammargerg K et al (2020) Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Austr 10(1):458–464
Boserup B, McKenney M, Elkbuli A (2020) Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med 38:2753
Usher K, Bhullar N, Durkin J et al (2020) Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs 29(4):549–552
Nelson BW, Pettitt AK, Flannery J, et al. (2020) Psychological and Epidemiological Predictors of COVID-19 Concern and Health-Related Behaviors. PsyArXiv2020
Rajkumar RP (2020) COVID-19 and mental health: A review of the existing literature. Asian J Psychiatry 52:102066
Westrupp E, Karantzas GC, Macdonald JA et al (2020) Study protocol for the COVID-19 pandemic adjustment survey (CPAS): a longitudinal study of Australian parents of a child 0–18 years. Front Psychiatry Public Health 11:903
Tull MT, Edmonds KA, Scamaldo KM et al (2020) Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res 289:113098
Liu CH, Zhang E, Wong GTF et al (2020) Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res 290:113172
Twenge J, Joiner TE (2020) Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol 76:2170
Pierce M, Hope H, Ford T et al (2020) Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7:883
Fisher JR, Tran TD, Hammargerg K et al (2020) Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust 213:1
Neill E, Meyer D, Toh WL et al (2020) Alcohol Use in Australia during the early days of the COVID-19 Pandemic: Initial results from the COLLATE project. Psychiatry Clin Neurosci 74:542
Racine N, Cooke JL, Eirich R et al (2020) Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res 292:113307
Rosen Z, Weinberger-Litman SL, Rosenzweig C, Rosmarin DH, Muennig P, Carmody ER, Rao ST, Litman L (2020) Anxiety and distress among the first community quarantined in the US due to COVID-19: Psychological implications for the unfolding crisis. Available from: https://doi.org/10.31234/osf.io/7eq8c
Oosterhoff B, Palmer CA, Wilson J et al (2020) Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health 67:179
Patrick SW, Henkhaus LE, Zickafoose JS et al (2020) Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics 146:e2020016824
Meherali S, Punjani N, Louie-Poon S et al (2021) Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health 18(7):3432
Chung SKG, Chan XW, Lanier P, Wong P (2020) Associations Between Work-Family Balance, Parenting Stress, and Marital Conflicts During COVID-19 Pandemic in Singapore. Available from: https://doi.org/10.31219/osf.io/nz9s8
Romero E, López-Romero L, Domínguez-Álvarez B et al (2020) Testing the effects of COVID-19 confinement in Spanish children: the role of parents’ distress, emotional problems and specific parenting. Int J Environ Res Public Health 17(19):6975
Brown SM, Doom JR, Lechuga-Peña S et al (2020) Stress and parenting during the global COVID-19 pandemic. Child Abuse Neglect 110:104699
Roos LE, Salisbury M, Penner-Goeke L et al (2021) Supporting families to protect child health: parenting quality and household needs during the COVID-19 pandemic. PLoS ONE 16(5):e0251720
Duan L, Shao X, Wang Y et al (2020) An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord 275:112–118
Xie X, Xue Q, Zhou Y et al (2020) Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr 174:898
Liu S, Liu Y, Liu Y (2020) Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res 289:113070
Riehm KE, Holingue C, Kalb LG et al (2020) Associations between media exposure and mental distress among US adults at the beginning of the COVID-19 pandemic. Am J Prevent Med 59:630
Wang C, Pan R, Wan X et al (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17(5):1729
Harris K, English T, Harms PD et al (2017) Why are extraverts more satisfied? Personality, social experiences, and subjective well-being in college. Eur J Pers 31(2):170–186
Cortina MA, Gilleard A, Deighton J (2020) Emerging evidence: coronavirus and children and young people’s mental health. Evidence Based Practice Unit, London
Türkoğlu S, Uçar HN, Çetin FH et al (2020) The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol Int 37:1–7
Colizzi M, Sironi E, Antonini F et al (2020) Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci 10(6):341
Cairney J (2005) Housing tenure and psychological well-being during adolescence. Environ Behav 37(4):552–564
Evans GW, Lercher P, Kofler WW (2002) Crowding and children’s mental health: the role of house type. J Environ Psychol 22(3):221–231
Barnes M, Cullinane C, Scott S, Silvester S (2013) People living in bad housing: numbers and health impacts. University of London, London, UK
Brindley P, Jorgensen A, Maheswaran R (2018) Domestic gardens and self-reported health: a national population study. Int J Health Geogr 17(1):31
Knöchelmann A, Seifert N, Günther S et al (2020) Income and housing satisfaction and their association with self-rated health in different life stages. A fixed effects analysis using a German panel study. BMJ Open 10(6):e034294
Crawford J, Cayley C, Wilson P et al (2011) Percentile norms and accompanying interval estimates for self report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychol 46(1):3–14
Cardamone-Breen MC, Jorm AF, Lawrence KA et al (2018) A single-session, web-based parenting intervention to prevent adolescent depression and anxiety disorders: randomized controlled trial. J med Internet Res 20(4):e148
Westrupp E, Karantzas GC, Macdonald JA, Olive L, Youssef G, Greenwood C, Sciberras E, Fuller-Tyszkiewicz M, Evans S, Mikocka-Walus A et al (2020) Study protocol for the COVID-19 Pandemic Adjustment Survey (CPAS): A longitudinal study of Australian parents of a child 0-18 years. Frontiers In Psychiatry - Public Health, 2020. 11
Soloff C, Lawrence D, Johnstone R (2005) Sample Design (LSAC Technical Paper No.1). Melbourne: Australian Institute of Family Studies
Gray M, Sanson A (2005) Growing up in Australia: the Longitudinal study of Australian children. Fam Matters 72:4–9
Australian Bureau of Statistics (2016) Census of Population and Housing: General Community Profile Catalogue number 2001.0 2017; Available from: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/communityprofile/036?opendocument
Kolenikov S (2014) Calibrating survey data using iterative proportional fitting (raking). Stata J 14(1):22–59
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36(3):1–48
Perneger TV (1998) What’s wrong with Bonferroni adjustments. BMJ 316(7139):1236
Funder DC, Ozer DJ (2019) Evaluating effect size in psychological research: sense and nonsense. Adv Methods Pract Psychol Sci 2(2):156–168
Wilkinson AL, Scollo MM, Wakefield MA et al (2019) Smoking prevalence following tobacco tax increases in Australia between 2001 and 2017: an interrupted time-series analysis. Lancet Public Health 4(12):e618–e627
Jiao WY, Wang LN, Liu J et al (2020) Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr 221:264
Zhou S-J, Zhang L-G, Wang L-L et al (2020) Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 29:1–10
Amerio A, Brambilla A, Morganti A et al (2020) COVID-19 lockdown: housing built environment’s effects on mental health. Int J Environ Res Public Health 17(16):5973
Evans GW, Saegert S, Harris R (2001) Residential density and psychological health among children in low-income families. Environ Behav 33(2):165–180
Asmundson GJG, Paluszek MM, Landry CA et al (2020) Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J Anxiety Disord 74:102271
Skokauskas N, Gallagher L (2012) Mental health aspects of autistic spectrum disorders in children. J Intellect Disabil Res 56(3):248–257
Craig F, Operto FF, De Giacomo A et al (2016) Parenting stress among parents of children with neurodevelopmental disorders. Psychiatry Res 242:121–129
Efron D, Mulraney M, Sciberras E et al (2020) Patterns of long-term ADHD medication use in Australian children. Arch Dis Child 105(6):593–597
May T, Sciberras E, Brignell A et al (2017) Autism spectrum disorder: updated prevalence and comparison of two birth cohorts in a nationally representative Australian sample. BMJ Open 7(5):e015549
Joseph CI, Evans S, Youssef GJ et al (2019) Characterisation of depressive symptoms in young children with and without attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 28(9):1183–1192
Becker-Haimes EM, Jensen-Doss A, Birmaher B et al (2018) Parent–youth informant disagreement: Implications for youth anxiety treatment. Clin Child Psychol Psychiatry 23(1):42–56
Vahedi A, Krug I, Westrupp EM (2019) Crossover of parents’ work-family conflict to family functioning and child mental health. J Appl Dev Psychol 62:38–49
Westrupp EM, Strazdins L, Martin A et al (2015) Maternal work-family conflict and psychological distress: Reciprocal relationships over 8 years. J Marriage Fam 78:107
Braithwaite S, Holt-Lunstad J (2017) Romantic relationships and mental health. Curr Opin Psychol 13:120–125
Beach S (2014) The couple and family discord model of depression. Interpers Relationsh Health Soc Clin Psychol Mech 1:133–155
Broadway B, Méndez S, Moschion J. (2020) Behind closed doors: The surge in mental distress of parents. Melbourne: Applied Economic & Social Research, University of Melbourne. Contract No.: 21/20
Merikangas K, Milham M, Stringaris A. The CoRonavIruS Health Impact Survey (CRISIS) V0.1 2020 Available from: https://github.com/nimh-mbdu/CRISIS
Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther 33(3):335–343
Bjureberg J, Ljótsson B, Tull MT et al (2016) Development and validation of a brief version of the Difficulties in emotion regulation scale: the DERS-16. J Psychopathol Behav Assess 38(2):284–296
Sharp C, Goodyer IM, Croudace TJ (2006) The Short Mood and Feelings Questionnaire (SMFQ): a unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7-through 11-year-old children. J Abnorm Child Psychol 34(3):365–377
Reardon T, Spence SH, Hesse J et al (2018) Identifying children with anxiety disorders using brief versions of the Spence Children’s Anxiety Scale for children, parents, and teachers. Psychol Assess 30(10):1342
Zubrick S, Lucas N, Westrupp E, et al. (2014) Parenting measures in the Longitudinal Study of Australian Children: construct validity and measurement quality, Waves 1 to 4. Canberra: Australian Government
Westrupp EM, Rose N, Nicholson JM et al (2015) Exposure to inter-parental conflict across 10 years of childhood: data from the longitudinal study of Australian children. Matern Child Health J 19(9):1966–1973
Halberstadt AG, Cassidy J, Stifter CA et al (1995) Self-expressiveness within the family context: Psychometric support for a new measure. Psychol Assess 7(1):93
Acknowledgements
EW, AM, and GK were supported by Deakin Faculty of Health Mid-Career Fellowships. DH was supported by a NHMRC Investigator Grant (1197488). ES was supported by an NHMRC Career Development Fellowship (1110688), a Medical Research Future Fund Investigator Grant (1194297) and a veski Inspiring Women’s Fellowship. LO was supported by an NHMRC Early Career Fellowship (1158487).
Funding
The current study was supported by funding from the Centre for Social and Early Emotional Development, School of Psychology, Victoria, Australia.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EW, CB, TB, and CG. The first draft of the manuscript was written by EW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None to disclose.
Ethical approval
The study was approved by the Deakin University Human Ethics Advisory Group (HEAG-H 52_2020).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Westrupp, E.M., Bennett, C., Berkowitz, T. et al. Child, parent, and family mental health and functioning in Australia during COVID-19: comparison to pre-pandemic data. Eur Child Adolesc Psychiatry 32, 317–330 (2023). https://doi.org/10.1007/s00787-021-01861-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01861-z