Abstract
Coronavirus disease 2019 (COVID-19) is a viral disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). While evaluating nasopharyngeal swabs by real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) is diagnostic, thorax computed tomography (CT) findings are also guiding in diagnosis. The association of pneumothorax and pleural effusion is not common in coronavirus disease. We presented the nucleic acid detection by a pleural swab sample in a COVID-19 patient with ground-glass opacity appearance and spontaneous pneumothorax.
Similar content being viewed by others
Introduction
Nasopharyngeal swabs are the main means of detecting SARS-CoV-2. Although the virus is found to be positive in the stool especially after the 2nd week of the disease, this transmission has been reported as a possibility suggests that fecal-oral transmission is unlikely. The virus is rarely found positive in blood and urine, and it is accepted that the virus does not pose a security problem in terms of blood banking. Besides, the virus was not detected in breast milk, vaginal swabs, and sperm samples. Pleural involvement is less common and a poor prognosis indicator. We presented a rare case that we found SARS-Cov-2 positivity in the pleural swap sample by an rRT-PCR in a COVID-19 patient who had a pneumothorax.
Case Report
A 61-year-old man was admitted to the emergency department with a cough, high fever, shortness of breath, and chest pain. There was no known systemic disease. The general health condition was poor. In his physical examination, breathing sounds could not be obtained in the left hemithorax. In vital signs, he had a fever of 39°C, blood pressure was 116/70 mmHg, heart rate was 120 beats per minute, respiratory rate was 22 breaths per minute, and oxygen saturation was 90% in pulse oximetry with an oxygen mask at 60% of fraction inhaled oxygen.
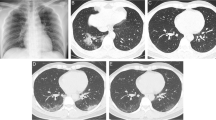
Chest CT scans showed bilateral infiltrates and pneumothorax in the left hemithorax (Fig. 1). A chest tube was placed with attention to contamination precautions after a pleural swab sample was taken through the tube thoracostomy. Subsequently, a nasopharyngeal swab sample was taken routinely. Chest X-ray radiography showed the re-expanded left lung by the placed chest tube (Fig. 2). The patient’s both swab sample results were positive for SARS-Cov-2.
Discussion
The nasopharyngeal area, where the agent is frequently obtained, is the most frequently used sampling site where the swabs are performed, due to its relatively easier application. While trying to diversify the sample locations, Jiufeng Sun et al. obtained 490 specimens including throat swab, sputum, nasopharyngeal swab, and fecal samples from their 49 cases with COVID-19 for evaluation of the SARS-CoV-2 RNA positivity in body fluids. They found the positivity of the test results as 16, 38, 89, and 28, respectively [1].
Yang et al. performed 205 throat swabs, 490 nasal swabs, and 142 sputum samples and used an rRT-PCR test in their 213 COVID-19 patients. Within the first 7 days of the disease, 11% of sputum, 27% of nasal, and 40% of throat samples were considered falsely negative [2]. Negative results cannot rule out infection if disease probability is high, so unexpected negative results should not be relied upon [3].
Positive sampling with pleural swabs has been rarely shown in the literature. Federico et al. presented the first positive sampling in pleural fluid in a 72-year-old patient [4]. They advocated also that pleural swab sampling would be helpful in diagnostic evaluation in patients with negative upper respiratory tract rRT-PCR.
Thorax CT is a sensitive diagnostic approach in the early period in patients with a negative rRT-PCR test COVID-19. Thorax CT is recommended to support the faster triage of these patients. If pre-diagnosed, patients with bilateral infiltrations on chest radiography or bilateral multilobar ground-glass opacities with multifocal consolidations on CT should be considered as patients with a high probability of COVID.
The percentage of ground-glass opacities or consolidation or both of them was reported in 80% and pneumothorax was in 1% of the studies [5]. Our case was a rare condition due to the development of spontaneous pneumothorax due to SARS-CoV-2 infection.
In conclusion, in suspicious cases, in all patients with pneumothorax or pleural effusion, pleural swab sampling should also be performed while inserting a chest tube by tube thoracostomy in case of the possibility of missing the diagnosis of coronavirus disease 2019 with a falsely negative nasopharyngeal swab. Testing samples from multiple regions can increase sensitivity and reduce false-negative test results. While sampling, contamination protection measures should be taken meticulously. The collection of radiological findings of the coronavirus infection and sampling styles in diagnosis are still areas where new studies are ongoing.
References
Sun J, Xiao J, Sun R, Tang X, Liang C, Lin H, Zeng L, Hu J, Yuan R, Zhou P, Peng J, Xiong Q, Cui F, Liu Z, Lu J, Tian J, Ma W, Ke C (2020) Prolonged persistence of SARS-CoV-2 RNA in body fluids. Emerging Infectious Diseases 26(8):1834–1838. https://doi.org/10.3201/eid2608.201097
Yang Y, Yang M, Shen C et al (2020) Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. https://doi.org/10.1101/2020.02.11.20021493
Woloshin S, Patel N, Kesselheim AS (2020) False negative tests for SARS-CoV-2 infection - challenges and implications. N Engl J Med 383(6):e38. https://doi.org/10.1056/NEJMp2015897
Mei F, Bonifazi M, Menzo S, di Marco Berardino A, Sediari M, Paolini L, Re A, Gonnelli F, Duranti C, Grilli M, Vennarucci GS, Latini MA, Zuccatosta L, Gasparini S (2020) First detection of SARS-CoV-2 by real-time reverse transcriptase-polymerase chain reaction assay in pleural fluid. Chest S0012-3692(20):31660–31663. https://doi.org/10.1016/j.chest.2020.05.583
Sun Z, Zhang N, Li Y, Xu X (2020) A systematic review of chest imaging findings in COVID-19. Quant Imaging Med Surg 10(5):1058–1079. https://doi.org/10.21037/qims-20-564
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keskin, H., Ulas, A.B., Aydin, Y. et al. Detection of SARS-CoV-2 RNA in the Pleural Swab of a COVID-19 Patient with a Pneumothorax. Indian J Surg 84, 386–388 (2022). https://doi.org/10.1007/s12262-021-02960-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-021-02960-6