Coronavirus Disease (COVID-19) Associated Rhinocerebral Mucormycosis and Complications: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v2i1.102Keywords:
Rhinocerebral mucormycosis, COVID-19, Diabetes mellitus, Glucocorticoids, Opportunistic infectionsAbstract
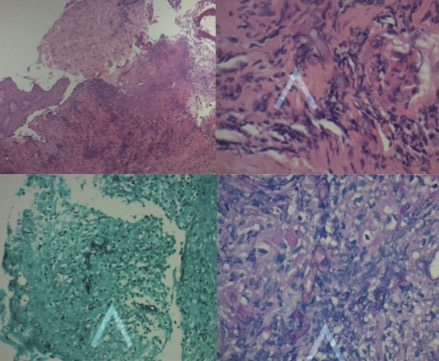
Background: Mucormycosis is a rare fatal infection caused by a ubiquitous fungus from the order of Mucorales, which can have varying clinical presentations. Immunocompromised patients are particularly susceptible to mucormycosis and can suffer fatal consequences if not treated adequately. COVID-19 infection with its immunomodulatory properties has been associated with a wide range of secondary bacterial and fungal infections. We present a case of rapidly progressive rhinocerebral mucormycosis post-COVID-19 infection with the subsequent development of several complications associated with the disease.
Case Report: A 62-year-old male patient with a history of hypertension and diabetes mellitus type II, presented 14 days post-COVID-19 recovery with right facial swelling, erythema, and right eye proptosis. Throughout his disease, the patient developed blindness and cranial nerve palsies. He was also found to have palatal necrotic lesions, consistent with the diagnosis of mucormycosis. The patient’s disease was complicated by Garcin syndrome, meningitis, orbital apex syndrome, cavernous sinus thrombosis, brain infarction, and hemorrhage. Despite all measures and interventions, the patient died.
Conclusion: COVID-19 infection and its treatments are associated with an increased risk of secondary fungal infections like mucormycosis. As such, a high index of suspicion is needed amongst healthcare workers for the early diagnosis and treatment of such opportunistic infections since prompt treatment is associated with a marked improvement in outcome. Furthermore, optimal glucose control and judicious use of corticosteroids in COVID-19 patients decreases the risk of developping such life threatening superinfections.
References
Song G, Liang G, Liu W. Fungal Co-infections Associated with Global COVID-19 Pandemic: A Clinical and Diagnostic Perspective from China. Mycopathologia. 2020;185(4):599-606. PMID: 32737747. https://doi.org/10.1007/s11046-020-00462-9
Moorthy A, Gaikwad R, Krishna S, et al. SARS-CoV-2, Uncontrolled Diabetes and Corticosteroids-An Unholy Trinity in Invasive Fungal Infections of the Maxillofacial Region? A Retrospective, Multi-centric Analysis [published online ahead of print, 2021 Mar 6]. J Maxillofac Oral Surg. 2021;20(3):1-8. PMID: 33716414. https://doi.org/10.1007/s12663-021-01532-1
Kwon-Chung KJ. Taxonomy of fungi causing mucormycosis and entomophthoramycosis (zygomycosis) and nomenclature of the disease: molecular mycologic perspectives. Clin Infect Dis. 2012;54 Suppl 1(Suppl 1):S8-S15. PMID: 22247451. https://doi.org/10.1093/cid/cir864
Mertens A, Barche D, Scheinpflug L, et al. Rhinocerebrale Mucormykose [Rhinocerebral Mucormycosis]. Laryngorhinootologie. 2018;97(8):550-554. PMID: 29768642. https://doi.org/10.1055/a-0619-5143
Morales-Franco B, Nava-Villalba M, Medina-Guerrero EO, et al. Host-Pathogen Molecular Factors Contribute to the Pathogenesis of Rhizopus spp. in Diabetes Mellitus [published online ahead of print, 2021 Jan 22]. Curr Trop Med Rep. 2021;1-12. PMID: 33500877. https://doi.org/10.1007/s40475-020-00222-1
Chakrabarti A, Das A, Mandal J, et al. The rising trend of invasive zygomycosis in patients with uncontrolled diabetes mellitus. Med Mycol. 2006;44(4):335-342. PMID: 16772227. https://doi.org/10.1080/13693780500464930
Chegini Z, Didehdar M, Khoshbayan A, Rajaeih S, Salehi M, Shariati A. Epidemiology, clinical features, diagnosis and treatment of cerebral mucormycosis in diabetic patients: A systematic review of case reports and case series. Mycoses. 2020;63(12):1264-1282. PMID: 32965744. https://doi.org/10.1111/myc.13187
Liu J, Li S, Liu J, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763. PMID: 32361250. https://doi.org/10.1016/j.ebiom.2020.102763
Potenza L, Vallerini D, Barozzi P, et al. Mucorales-specific T cells emerge in the course of invasive mucormycosis and may be used as a surrogate diagnostic marker in high-risk patients. Blood. 2011;118(20):5416-5419. PMID: 21931119. https://doi.org/10.1182/blood-2011-07-366526
Hosseini SM, Borghei P. Rhinocerebral mucormycosis: pathways of spread. Eur Arch Otorhinolaryngol. 2005;262(11):932-938. PMID: 15891927. https://doi.org/10.1007/s00405-005-0919-0
Balai E, Mummadi S, Jolly K, Darr A, Aldeerawi H. Rhinocerebral Mucormycosis: A Ten-Year Single Centre Case Series. Cureus. 2020;12(11):e11776. Published 2020 Nov 29. PMID: 33409023. https://doi.org/10.7759/cureus.11776
Beiglboeck FM, Theofilou NE, Fuchs MD, et al. Managing mucormycosis in diabetic patients: A case report with critical review of the literature [published online ahead of print, 2021 Feb 14]. Oral Dis. 2021;10.1111/odi.13802. PMID: 33583133. https://doi.org/10.1111/odi.13802
Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634-653. PMID: 16080086. https://doi.org/10.1086/432579
Hoang K, Abdo T, Reinersman JM, Lu R, Higuita NIA. A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Med Mycol Case Rep. 2020;29:22-24. PMID: 32547914. https://doi.org/10.1016/j.mmcr.2020.05.008
Ferguson AD. Rhinocerebral mucormycosis acquired after a short course of prednisone therapy. J Am Osteopath Assoc. 2007;107(11):491-493. PMID: 18057223
RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693-704. PMID: 32678530. https://doi.org/10.1056/nejmoa2021436
Canhão P, Cortesão A, Cabral M, et al. Are steroids useful to treat cerebral venous thrombosis?. Stroke. 2008;39(1):105-110. PMID: 18063833. https://doi.org/10.1161/strokeaha.107.484089
Koc Z, Koc F, Yerdelen D, Ozdogu H. Rhino-orbital-cerebral mucormycosis with different cerebral involvements: infarct, hemorrhage, and ophthalmoplegia. Int J Neurosci. 2007;117(12):1677-1690. PMID: 17987470. https://doi.org/10.1080/00207450601050238
Yang H, Wang C. Looks like Tuberculous Meningitis, But Not: A Case of Rhinocerebral Mucormycosis with Garcin Syndrome. Front Neurol. 2016;7:181. PMID: 27822198. https://doi.org/10.3389/fneur.2016.00181
Published
How to Cite
Issue
Section
Copyright (c) 2021 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







