Published online Aug 6, 2020. doi: 10.12998/wjcc.v8.i15.3156
Peer-review started: April 30, 2020
First decision: May 21, 2020
Revised: May 22, 2020
Accepted: July 22, 2020
Article in press: July 22, 2020
Published online: August 6, 2020
The current pandemic of coronavirus disease 2019 (COVID-19) which was first detected in Wuhan, China in December 2019 is caused by the novel coronavirus named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The virus has quickly spread to a large number of countries leading to a great number of deaths. Unfortunately, till today there is no specific treatment or vaccination for SARS-CoV-2. Most of the suggested treatment medications are based on in vitro laboratory investigations, experimental animal models, or previous clinical experience in treating similar viruses such as SARS-CoV-1 or other retroviral infections. The running of any clinical trial during a pandemic is affected at multiple levels. Reasons for this include patient hesitancy or inability to continue investigative treatments due to self-isolation/quarantine, or limited access to public places (including hospitals). Additional barriers relate to health care professionals being committed to other critical tasks or quarantining themselves due to contact with COVID-19 positive patients. The best research approaches are those that adapt to such external unplanned obstacles. Ongoing clinical trials before COVID-19 pandemic have the potential for identifying important therapies in the long-term if they can be completed as planned. However, these clinical trials may require modifications due a pandemic such as this one to ensure the rights, safety, and wellbeing of participants as well as medical staff involved in the conduction of clinical trials. Clinical trials initiated during the pandemic must be time-efficient and flexible due to high contagiousness of severe acute respiratory syndrome coronavirus 2, the significant number of reported deaths, and time constraints needed to perform high quality clinical trials, enrolling adequate sample sizes. Collaboration between different countries as well as implementation of innovative clinical trial designs are essential to successfully complete such initiatives during the current pandemic. Studies looking at the long term sequalae of COVID-19 are also of importance as recent publications describe multi-organ involvement. Long term follow-up of COVID-19 survivors is thus also important to identify possible physical and mental health sequellae.
Core tip: Clinical research during coronavirus disease 2019 (COVID-19) is essential to provide high-quality timely critical diagnostic and therapeutic information. Collaborative work is encouraged to support limited resources countries and overcome public health crises in the future. Preventative and interventional measures should be prioritized. Ongoing studies having been initiated before the pandemics arise should be rigorously evaluated by trial sponsors. Priority during the pandemic should be given to completing timely clinical trials focusing on the management of COVID-19 patients.
- Citation: AlNaamani K, AlSinani S, Barkun AN. Medical research during the COVID-19 pandemic. World J Clin Cases 2020; 8(15): 3156-3163
- URL: https://www.wjgnet.com/2307-8960/full/v8/i15/3156.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i15.3156
The number of infectious diseases outbreaks over the past few decades have increased. This has created an enormous additional burden on the health systems of many countries around the world. As a majority of research activities during outbreaks targeting the causal organism must be completed in a timely fashion, it is of no surprise that effective preventative measures such as vaccination or therapies have not been available for many previous pandemic infectious diseases; in fact most of the previously used medications during past outbreaks have not been based on high quality evidence[1].
Despite the dedication of enormous resources, the advancement in health care systems and collaboration between different investigators across the world, only a small number of patients over the last decade have in fact benefited from clinical research performed during different outbreaks of respiratory viruses such as was the case for the severe acute respiratory syndrome (SARS), the HIN1 flu virus (swine flu) or the Middle East Respiratory Syndrome. Most of the medical research allocated resources and funding tend to happen during the disease outbreak. Unfortunately lack of continuation of funding once the outbreak is over has led to disruption of many clinical trials assessing preventative, diagnostic, and therapeutic strategies[2].
The current pandemic of coronavirus disease 2019 (COVID-19) which was first detected in Wuhan, China in December 2019 is caused by the novel coronavirus named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)[3]. The virus eventually spread to different regions of China and to the rest of the world leading to more than three million confirmed cases and hundreds of thousands of deaths at the time of writing of this manuscript[4].
Initial reports from the highly affected three countries China, Italy and Spain suggest that COVID-19 has caused high mortality rate and/or overwhelmed regional intensive care units (ICU) capacity[5,6].
The virus spreads via contact with infected upper respiratory droplets. The clinical presentation varies markedly from asymptomatic carriers to patients with acute respiratory distress syndrome requiring ICU admission and mechanical ventilation[7]. Certain groups of patients are at higher risk for developing complications and death. High mortality rates have been associated with advanced age, presence of underlying disease, presence of secondary infection and elevated inflammatory markers[8].
Medical personnel in many countries have also been affected, leading to absence from work and, tragically, death in some cases.
Unfortunately, till today there is no specific treatment or vaccination for SARS-CoV-2 Reports from initially affected countries describe using different medications such as Hydroxychloroquine with Azithromycin and in some adding anti-viral medications such as Lopinavir/Ritonavir, Remdesivir or Favipiravir for severe cases[9-13]. Other management options include Inter-Leukin 6 and extracted immunoglobulin from recovered patients that have also been used with variable results[14]. Most of the suggested treatment medications are based on in vitro laboratory investigations, experimental animal models, or previous experience in treating similar viruses such as SARS-CoV-1 or other retroviral infections.
It is important to note that in most of these trials there was no control group, therefore the safety profile and effectiveness of the studied medications cannot be accurately determined.
Due to the very contagious nature of SARS-CoV-2, overwhelming the capacity of the health care system including out-patient clinics, in-hospital wards and ICUs, and in light of the significant mortality in the absence of effective treatment or prophylactic vaccination, focused medical research on SARS-CoV-2 is a necessity during this pandemic, with all patients deserving evidence-based care. The entire world needs a coordinated effort of all the available knowledge and resources to fight this pandemic and possibly similar future pandemics.
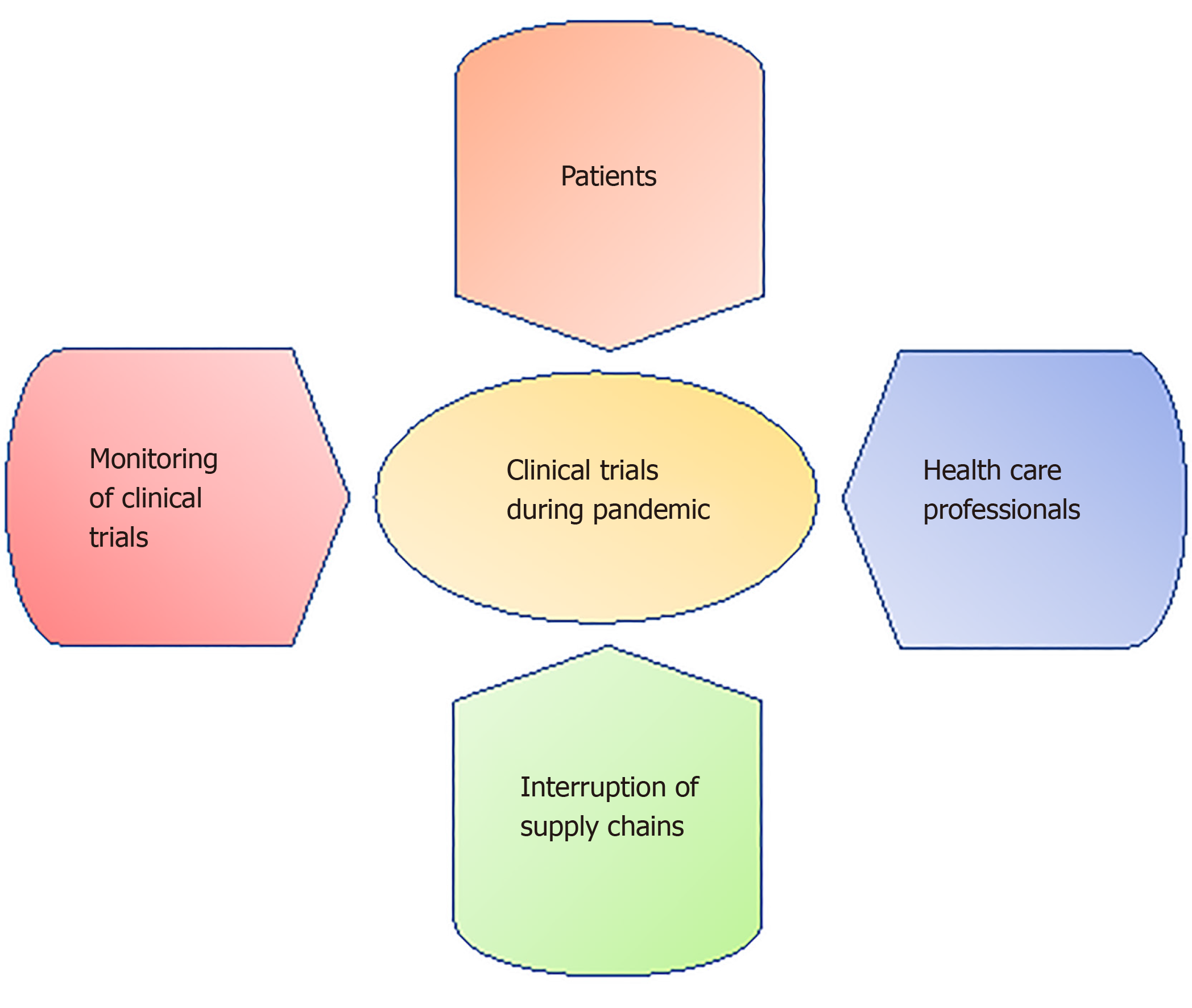
But it is challenging to conduct research during pandemics. Indeed, the running of clinical trials during a pandemic is affected at multiple levels. Reasons for this include patient hesitancy or inability to continue investigative treatments due to self-isolation/quarantine, or limited access to public places (including hospitals). Additional barriers relate to health care professionals being committed to other critical tasks or quarantining themselves due to contact with COVID-19 positive patients[15]. Interruption of supply chains and monitoring of clinical trials are additional obstacles to medical research during pandemics (Figure 1). The best research approaches are those that will adapt to such external unplanned obstacles.
As example, similar to other research institutions, we are facing many challenges and obstacles at our own centers. Perhaps one of the most important barriers are a patient’s understandable anxiety and fear related to the current COVID-19 pandemic. Indeed, they are very hesitant to visit health care facilities to participate in new clinical trials, let alone continue in ongoing ones. Some patients have also been quarantined due to contact with confirmed COVID-19 cases. Investigators at our institutions especially those involved in sponsored clinical trials are also facing challenges related to interruptions in the supply chains for investigational products, coupled to the inability of trial personnel to perform visits and/or investigations on enrolled patients.
Ethics committees must apply rigorous standards to authorize research in accordance with the principles of justice, equity and solidarity. Lapses were reported during previous outbreaks such as in the West Africa Ebola Virus (EV) outbreak leading to incomplete studies and inconclusive results[16-18]. Although we must strive to avoid publication bias (only submitting “positive studies”), the importance of unpublished data or not publishing incomplete data and inconclusive results must also be stressed. Take for example the randomized controlled trial performed during an EV outbreak in 2014 looking at a triple monoclonal antibody cocktail (ZMapp) as treatment for EV. The investigators concluded that the estimated effect of ZMapp appeared to be beneficial, but the results in fact did not meet the prespecified statistical threshold for efficacy, thus leading to an underpowered negative trial[18]. An example of unpublished results that need to be widely acknowledged because of a negative outcome leading to early termination is that of a Brazilian study (CloroCovid-19 ) which was a parallel, double-blind, randomized, phase IIb clinical trial, which started on March 23, 2020, aiming to assess safety and efficacy of Chloroquine diphosphate (CQ) in the treatment of hospitalized patients with severe respiratory syndrome secondary to SARS-CoV-2 infection. The high dose of CQ 600 mg at twice daily for 10 d led to a higher fatality rate (27%) by day 13 of the trial compared to the lower dose group and historical data from similar patients not using CQ[19].
Medical research must therefore be adapted to the new socio-economic reality during the COVID-19 pandemic. Such studies can be divided into three main categories: Ongoing medical research that antedated the pandemic, new research that is initiated during the pandemic, and future research on COVID-19 that will follow it.
Ongoing clinical trials have the potential for benefiting millions of lives in the long-term if they can be completed as planned, for example for certain types of cancers or diseases to which no cure currently exits. Clinical trials in such patients are often the standard of care and may represent a patient’s only hope. Furthermore, discontinuation of ongoing trials represents a waste of resources, and of time and efforts of patients who have completed the trial as well as medical and research personal involved in their design and implementation. Supporting the efforts to continue ongoing clinical trials and modifying them, if necessary, is thus essential.
The COVID-19 pandemic poses significant challenges for many ongoing clinical research trials because of additional challenges. Indeed, examples of barriers faced by sponsors and investigators include interruptions to the supply chains for the investigational products if applicable, the inability of trials personnel to perform visits and/or laboratory or imaging tests on enrolled patients, data entry, serious adverse events notification, and more generally follow various additional aspects of published trials protocols.
Due to above constrains, as a result, a series of measures need to be instituted, ensuring the rights, safety, and wellbeing of participants as well as the medical staff involved in the conduction of clinical trials. Both sponsors and investigators must understand the critical situation faced by the medical authorities around the globe. Fairness is thus a better way of approaching the ethical issues faced by clinical trial staff and regulatory agencies during this pandemic. Fairness refers to the equitable distribution of benefits. It is about meeting everyone’s individual needs; therefore cultural, racial, social or other biases must be avoided. In addition, clinical trials sponsors as well as investigators must uphold the spirit of existing laws while remaining fair to all individuals involved in the clinical trials[20].
Clinical trial sponsors and investigators must decide whether trial subject safety considerations allow continuation of the protocols, or rather temporarily halting administration of the interventional productor patient recruitment. Many research regulatory authorities such as the United States Food and Drug Administration and the Clinical Trials Expert Group at the European Medicines Agency have published statements to regulate medical research during the COVID-19 pandemic in order to ensure the safeguard and preservation of rights of patients, medical staff and personnel involved in conducting, monitoring and the follow-up data collection and analysis of clinical trials[21,22]. Local Institutional Review Boards (IRBs) are also encouraged to revise and modify their policies and procedures to adapt to the current situation without compromising patient care while ensuring the safety of all personnel involved in clinical trials. Additional extensions to study periods beyond those already provided by local IRBs must be allowed in order to accommodate for the unpredictable study operational time lost during this COVID-19 pandemic.
Adopted modifications must not compromise the integrity of the study methodology while the trial must continue to be conducted in accordance with Good Clinical Practices and comply with local and national regulatory requirements. Modifications of protocols such as delaying recruitment of patients, postponing certain assessments and monitoring subjects through phone calls or virtual visits, limiting study visits, and preventing large gathering of study subjects as well as permitting certain tests to be done in nearby clinics rather than centrally, where appropriate, will most likely ensure patient and medical staff safety without compromising progression of the trials. Sponsors as well as investigators should develop a process to identify, document, assess and report all protocol deviations to the sponsor and local IRBs. These protocol deviations must also be documented to better complete and interpret subsequent analyses of the study findings.
As it is not clear when the pandemic will end, it is important that investigators put the aforementioned strategies into place for an adequate period of time.
Medical research during COVID-19 pandemic should focus on the epidemiology of the SARS-CoV-2, its modes of transmission, COVID-19 clinical presentations, effectiveness of preventative measures and possible modalities of treatment. Medical research must be time-efficient and flexible due to high contagiousness of the SARS-CoV-2, the large number of reported deaths, and time constraints needed to perform high quality clinical trials.
Regulatory processes must facilitate the generation of data from observational studies in real world settings that may be very important in better guiding the development of vaccines and therapies of COVID-19 patients, and subsequently informing well designed, adequately powered, and well-funded randomized controlled trials. The latter should take priority, at least temporarily, over other competing clinical trials. Moreover, patients and clinicians should be encouraged to participate in such initiatives[23].
Time limitation is a major factor leading to the incompleteness of clinical trials during infectious diseases outbreaks. During the EV outbreak in 2014, the National Institutes of Health took several months to plan and launch the PREVAIL II trial. Unfortunately, this trial was never completed while drawing on very significant resources[18].
To overcome issues related to research during pandemic crises and to avoid publication bias a group of public health experts have advocated the use of a model called “core protocol”[24]. This model describes the implementation of multiple interventions addressing a single disease at the same time such as using different off label medications to treat COVID-19, or of a single intervention targeting multiple diseases across different outbreaks such as Remdesivir which was used to treat EV and now is being studies in COVID-19. This approach aims to minimize the time required to complete high quality clinical trials during outbreaks, with recognition of the additional important role of timely interim analyses to limit futility or harm and enhance the early recognition of efficacy. Subsequent publication of results would only be carried out if pre-set criteria of efficacy or effectiveness are met (which may not be the case until further enrolment is reached during subsequent pandemics).
The rapid and unpredictable nature of many pandemic infectious diseases such as COVID-19 makes it impossible for a limited number of researchers to produce meaningful clinical results. To overcome such an obstacle, multi-center trials involving different countries with two-way exchange of information, protocols and procedures is an essential part of the global approach to any pandemic situation[25]. Such collaboration should be supported and facilitated by regulators in order to preserve resources and avoid underpowered studies, while achieving the planned outcomes. This will also help countries with limited resources that report on lower numbers of cases due to unavailability of testing. An excellent example of this kind of collaboration is the SOLIDARITY trial–a World Health Organization-funded international study of potential treatments for COVID-19 to be conducted in Asia, South Africa, Europe, and the Americas[26].
In pandemic times, therapeutic priority must be given to research focusing on interventions. Investigators must concentrate on studying the effectiveness of already developed and approved medications used for similar viruses. The development of new drugs and testing through multi-phases during such emergencies may only be of limited benefit for the current pandemic affected patients, however results will of course be of help for similar future pandemics.
As discussed above, modifications of policies and regulations established by local IRBs during COVID-19 to maintain ongoing studies should also be applied to new clinical trial submissions involving COVID-19 patients.
It is essential to discover new drugs to effectively fight what are likely repeated infectious diseases outbreaks in time. Off-label use of available medications has disadvantages such as unknown efficacy, side effects and drug-drug interactions. Therefore, when the pandemic is over, clinical trials that started during the pandemic of COVID-19 should continue with their findings published once the planned accrual and/or efficacy, harm, or futility endpoints have been reached.
Other studies that may have used the earlier described core protocol model should extend across future multiple infectious disease outbreaks[24].
Due to the limited time available to enroll the large sample sizes of patients required for many high-quality clinical trials, and the enormous resources required during emergency pandemic diseases, earlier preparation for future outbreaks is becoming crucial for producing meaningful research findings. Such planning should include multi-center participation from different countries to ensure sufficient sample size and representative diverse patient demographics favoring broad generalizability of results and meaningful, adequately powered subgroup analyses[27]. Such participation requires research capacity building, especially in countries with limited resources as well as support and collaboration from regulatory bodies to ensure success[28].
The rapid action from concept to implementation of clinical studies is crucial during infectious disease outbreaks. This kind of approach will require innovative research designs such as “n of 1” trials[29] adaptive platform trials[30], or ring vaccination designs[31] with pre-outbreak approval, rapid implementation and timely effective methods of data exchange across global collaborations. Continuation of research on banked patient materials such as fluids and tissue samples collected during outbreaks after appropriate consent will likely further enhance diagnostic and therapeutic discoveries.
Studies looking at the long term sequalae of COVID-19 are also of importance. As recent publications describe multi-organ involvement, long term follow-up of COVID-19 survivors can assist in identifying possible physical and mental health sequellae.
Laboratory based research such as life-saving vaccines and therapies, particularly against the new coronavirus must continue. Cell lines research are essential for the production of vaccines, as are testing drug metabolism, cytotoxicity and antibody production during a pandemic[32-34]. Maintenance of cell lines requires uninterrupted examination of cell morphology and periodic change of medium[35]. This kind of maintenance could be affected during COVID-19 pandemic due to reduction of research laboratory staff and interruption in supply chains.
Currently, millions of animals are used in research laboratories around the globe[36]. Indeed, animals need to be looked after, and breeding lines must be kept intact. However, in some laboratories the work force has been reduced with researchers asked to stay away from their laboratories to minimize their risk of exposure to SARS-COV-2. These understandable measures have nonetheless affected the care and wellbeing of experimental animals. Some researchers were even asked to dispose of animals while others had to interrupt their research in a way that will likely require the use of another animals once back to work[37].
To minimize the impact of COVID-19 on laboratory-based research, researchers should follow local institutions’ safety regulations.
Many laboratory-based research institutions have established new regulation to ensure safety of investigators and continuity of work[38]. Some of these new regulations include reducing laboratory workforce to those conducting essential work, establishing a system of reporting symptoms and signs suggestive of COVID-19, working in small groups and keeping a distance of at least two meters between staff while also implementing working shifts.
Clinical research plays a primordial societal role during pandemic emergencies. Collaborative work with participation from different countries including the adequate support of limited resources countries are important elements that will help deal with and overcome such public health crises in the future. Preventative, diagnostic, and interventional measures should be prioritized. Ongoing studies before the pandemics arise should be rigorously evaluated by trials sponsors, investigators and local IRBs. Modifications of existing protocols to ensure the safety of patients and medical personnel is essential. Continuation of research and long term follow-up studies are required to discover therapies and to support survivors of infectious disease outbreaks.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang MLC, Zhang H S-Editor: Zhang L L-Editor: A E-Editor: Xing YX
| 1. | Mehand MS, Al-Shorbaji F, Millett P, Murgue B. The WHO R&D Blueprint: 2018 review of emerging infectious diseases requiring urgent research and development efforts. Antiviral Res. 2018;159:63-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 197] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 2. | Jia HP, Min Wu, Sustained research fund and dedicated research center for preparing next pandemic, Precision Clinical Medicine, pbaa012. . [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Zheng J. SARS-CoV-2: an Emerging Coronavirus that Causes a Global Threat. Int J Biol Sci. 2020;16:1678-1685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 650] [Cited by in F6Publishing: 537] [Article Influence: 134.3] [Reference Citation Analysis (0)] |
| 4. | Deng CX. The global battle against SARS-CoV-2 and COVID-19. Int J Biol Sci. 2020;16:1676-1677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 5. | Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20:773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 711] [Cited by in F6Publishing: 664] [Article Influence: 166.0] [Reference Citation Analysis (0)] |
| 6. | Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2713] [Cited by in F6Publishing: 2658] [Article Influence: 664.5] [Reference Citation Analysis (0)] |
| 7. | Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1854] [Cited by in F6Publishing: 1941] [Article Influence: 485.3] [Reference Citation Analysis (0)] |
| 8. | Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846-848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2604] [Cited by in F6Publishing: 3048] [Article Influence: 762.0] [Reference Citation Analysis (0)] |
| 9. | Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. 2020;14:72-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1597] [Cited by in F6Publishing: 1561] [Article Influence: 390.3] [Reference Citation Analysis (0)] |
| 10. | Chen Z, Hu J, Zhang Z, Jiang S, Han S, Yan D, Zhuang R, Hu B, Zhang Z. Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. 2020 Preprint. [DOI] [Cited in This Article: ] |
| 11. | Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;105949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3242] [Cited by in F6Publishing: 3180] [Article Influence: 795.0] [Reference Citation Analysis (0)] |
| 12. | Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4289] [Cited by in F6Publishing: 4373] [Article Influence: 1093.3] [Reference Citation Analysis (0)] |
| 13. | Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov. 2020;19:149-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1082] [Cited by in F6Publishing: 1058] [Article Influence: 264.5] [Reference Citation Analysis (0)] |
| 14. | Michot JM, Albiges L, Chaput N, Saada V, Pommeret F, Griscelli F, Balleyguier C, Besse B, Marabelle A, Netzer F, Merad M, Robert C, Barlesi F, Gachot B, Stoclin A. Tocilizumab, an anti-IL-6 receptor antibody, to treat COVID-19-related respiratory failure: a case report. Ann Oncol. 2020;31:961-964. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 221] [Cited by in F6Publishing: 236] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 15. | McDermott MM, Newman AB. Preserving Clinical Trial Integrity During the Coronavirus Pandemic. JAMA. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 132] [Cited by in F6Publishing: 128] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 16. | Kennedy SB, Neaton JD, Lane HC, Kieh MW, Massaquoi MB, Touchette NA, Nason MC, Follmann DA, Boley FK, Johnson MP, Larson G, Kateh FN, Nyenswah TG. Implementation of an Ebola virus disease vaccine clinical trial during the Ebola epidemic in Liberia: Design, procedures, and challenges. Clin Trials. 2016;13:49-56. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Samai M, Seward JF, Goldstein ST, Mahon BE, Lisk DR, Widdowson MA, Jalloh MI, Schrag SJ, Idriss A, Carter RJ, Dawson P, Kargbo SAS, Leigh B, Bawoh M, Legardy-Williams J, Deen G, Carr W, Callis A, Lindblad R, Russell JBW, Petrie CR, Fombah AE, Kargbo B, McDonald W, Jarrett OD, Walker RE, Gargiullo P, Bash-Taqi D, Gibson L, Fofanah AB, Schuchat A; STRIVE Study Team. The Sierra Leone Trial to Introduce a Vaccine Against Ebola: An Evaluation of rVSV∆G-ZEBOV-GP Vaccine Tolerability and Safety During the West Africa Ebola Outbreak. J Infect Dis. 2018;217:S6-S15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 18. | PREVAIL II Writing Group. Multi-National PREVAIL II Study Team, Davey RT Jr, Dodd L, Proschan MA, Neaton J, Neuhaus Nordwall J, Koopmeiners JS, Beigel J, Tierney J, Lane HC, Fauci AS, Massaquoi MBF, Sahr F, Malvy D. A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. N Engl J Med. 2016;375:1448-1456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 361] [Cited by in F6Publishing: 356] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 19. | Borba M, Val F, Sampaio V, Alexandre M, Melo G, Brito M, Mourao M, De Brito Sousa, Jose D, Baia-da-Silva D, Guerra M, Hajjar L, Pinto R, Balieiro A, Naveca F, Xavier M, Salomao A, Siqueira A, Schwarzbolt A, Croda J, Lacerda M. Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study). 2020 Preprint. [DOI] [Cited in This Article: ] |
| 20. | Byrd GD, Winkelstein P. A comparative analysis of moral principles and behavioral norms in eight ethical codes relevant to health sciences librarianship, medical informatics, and the health professions. J Med Libr Assoc. 2014;102:247-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic: guidance for industry, investigators, and institutional review boards. US Food and Drug Administration. Published March 2020. Accessed March 18, 2020. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fda-guidance-conduct-clinical-trials-medical-products-during-covid-19-pandemic. [Cited in This Article: ] |
| 22. | EMA Guidance on the Management of Clinical Trials during the COVID-19 (Coronavirus) pandemic. The European Medicines Agency. Published March 2020. Accessed March 27, 2020 Available from: https://ec.europa.eu/health/sites/health/files/files/eudralex/vol-10/guidanceclinicaltrials _covid19_en.pdf. [Cited in This Article: ] |
| 23. | Kalil AC. Treating COVID-19-Off-Label Drug Use, Compassionate Use, and Randomized Clinical Trials During Pandemics. JAMA. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 302] [Cited by in F6Publishing: 321] [Article Influence: 80.3] [Reference Citation Analysis (0)] |
| 24. | Dean NE, Gsell PS, Brookmeyer R, Crawford FW, Donnelly CA, Ellenberg SS, Fleming TR, Halloran ME, Horby P, Jaki T, Krause PR, Longini IM, Mulangu S, Muyembe-Tamfum JJ, Nason MC, Smith PG, Wang R, Henao-Restrepo AM, De Gruttola V. Creating a Framework for Conducting Randomized Clinical Trials during Disease Outbreaks. N Engl J Med. 2020;382:1366-1369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 25. | Rojek AM, Horby PW. Modernising epidemic science: enabling patient-centred research during epidemics. BMC Med. 2016;14:212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | WHO. Director-Generalâs opening remarks at the media briefing on COVID-19. March 18, 2020. Available from: https://www.who.int/dg/speeches/detail/who- director-general-s-opening-remarks-at-the-media-briefing-on-covid-19. [Cited in This Article: ] |
| 27. | Gobat N, Amuasi J, Yazdanpanah Y, Sigfid L, Davies H, Byrne JP, Carson G, Butler C, Nichol A, Goossens H. Advancing preparedness for clinical research during infectious disease epidemics. ERJ Open Res. 2019;5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 28. | Lurie N, Manolio T, Patterson AP, Collins F, Frieden T. Research as a part of public health emergency response. N Engl J Med. 2013;368:1251-1255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 148] [Cited by in F6Publishing: 142] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 29. | Lillie EO, Patay B, Diamant J, Issell B, Topol EJ, Schork NJ. The n-of-1 clinical trial: the ultimate strategy for individualizing medicine? Per Med. 2011;8:161-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 455] [Cited by in F6Publishing: 385] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 30. | Brueckner M, Titman A, Jaki T, Rojek A, Horby P. Performance of different clinical trial designs to evaluate treatments during an epidemic. PLoS One. 2018;13:e0203387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Rid A, Miller FG. Ethical Rationale for the Ebola "Ring Vaccination" Trial Design. Am J Public Health. 2016;106:432-435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Genzel Y. Designing cell lines for viral vaccine production: Where do we stand? Biotechnol J. 2015;10:728-740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 33. | Gomez-Lechon MJ, Donato MT, Lahoz A, Castell JC, Cell Lines: A Tool for In Vitro Drug Metabolism Studies. Current Drug Metabolism. 2008;9:1. [DOI] [Cited in This Article: ] [Cited by in Crossref: 210] [Cited by in F6Publishing: 216] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 34. | Li F, Vijayasankaran N, Shen AY, Kiss R, Amanullah A. Cell culture processes for monoclonal antibody production. MAbs. 2010;2:466-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 522] [Cited by in F6Publishing: 460] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 35. | Geraghty RJ, Capes-Davis A, Davis JM, Downward J, Freshney RI, Knezevic I, Lovell-Badge R, Masters JR, Meredith J, Stacey GN, Thraves P, Vias M, Cancer Research UK. Guidelines for the use of cell lines in biomedical research. Br J Cancer. 2014;111:1021-1046. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 36. | Akhtar A. The flaws and human harms of animal experimentation. Camb Q Healthc Ethics. 2015;24:407-419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 205] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 37. | Pullium JK. Care for laboratory animals during COVID-19 crisis. Nature. 2020;579:497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Powell K. Science-ing from home. Nature. 2020;580:419-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |