Abstract
Purpose
Coronavirus disease 2019 (COVID-19) is creating an unprecedented healthcare crisis. Understanding the determinants of mortality is crucial to optimise intensive care unit (ICU) resource use and to identify targets for improving survival.
Methods
In a multicentre retrospective study, we included 379 COVID-19 patients admitted to four ICUs between 20 February and 24 April 2020 and categorised according to time from disease onset to ICU admission. A Cox proportional-hazards model identified factors associated with 28-day mortality.
Results
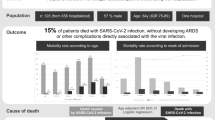
Median age was 66 years (53–68) and 292 (77%) were men. The main comorbidities included obesity and overweight (67%), hypertension (49.6%) and diabetes (30.1%). Median time from disease onset (i.e., viral symptoms) to ICU admission was 8 (6–11) days (missing for three); 161 (42.5%) patients were admitted within a week of disease onset, 173 (45.6%) between 8 and 14 days, and 42 (11.1%) > 14 days after disease onset; day 28 mortality was 26.4% (22–31) and decreased as time from disease onset to ICU admission increased, from 37 to 21% and 12%, respectively. Patients admitted within the first week had higher SOFA scores, more often had thrombocytopenia or acute kidney injury, had more limited radiographic involvement, and had significantly higher blood IL-6 levels. Age, COPD, immunocompromised status, time from disease onset, troponin concentration, and acute kidney injury were independently associated with mortality.
Conclusion
The excess mortality in patients admitted within a week of disease onset reflected greater non-respiratory severity. Therapeutic interventions against SARS-CoV-2 might impact different clinical endpoints according to time since disease onset.
Similar content being viewed by others
Time from COVID-19 viral symptom onset to ICU admission no longer than 7 days is associated with a higher risk of death. A faster onset of critical illness may be associated with kidney and myocardial injury in addition to lung injury, as well as with higher IL-6 concentrations. Interventions that are currently used in COVID-19 patients might impact different clinical endpoints according to time since viral symptom onset. |
Introduction
The COVID-19 pandemic has created an unprecedented healthcare crisis. With more than four million confirmed cases worldwide and nearly 280,000 deaths during the first 4 months of 2020, the number of patients with severe forms requiring critical care has overwhelmed intensive care units (ICUs) in many countries. Respiratory failure is the main source of morbidity and mortality in severe cases.
The causative agent of COVID-19, SARS-CoV-2 (severe acute respiratory syndrome-related coronavirus 2) [1, 2], is the third documented spillover of an animal coronavirus to humans in only two decades [3]. After an incubation period of about 5 days [4], clinical viral symptoms such as a fever, cough, sore throat, nasal congestion, myalgia, fatigue, headaches, and/or diarrhoea occur [5, 6]. Dyspnoea is reported in up to half the patients, and 5–20% of patients require ICU admission for acute respiratory failure [7]. In the earliest descriptions of COVID-19 patients hospitalised in Wuhan, China, time from viral symptom onset to dyspnoea was 5 days and time to hospital admission was 7 days [8, 9].
Understanding the determinants of poor outcomes in COVID-19 patients would help stratify patients at baseline based on a risk assessment to both avoid admitting patients to the ICU if they are at low risk for worsening and promptly admit patients likely to require critical care. Several studies have identified factors associated with mortality in COVID-19 patients. While advanced age has been recognised as a leading determinant of death in several studies [10, 11], little attention has been paid to outcome differences according to the timing of critical illness onset. A two-step model of lung and systemic injury seems involved, with the aggressive inflammation initiated by the viral replication resulting in a cytokine storm [12, 13]. Early after infection, SARS-CoV-2 binds to angiotensin-converting enzyme 2 receptors, multiplies in the cytoplasm, and leads to type II pneumocyte apoptosis [14]. Additionally, SARS-CoV-2 RNA acts as a pathogen-associated molecular pattern that induces a chemokine surge, which causes neutrophil migration and activation [15, 16]. The result is destruction of the alveolar-capillary walls and damage to the intra-alveolar space–stroma interface, causing exudative leakage. In addition to massive epithelial apoptosis, the early onset of rapid viral replication triggers endothelial cells to release pro-inflammatory cytokines and chemokines that cause further lung damage together with a systemic insult [17].
To test the hypothesis that COVID-19-related critical illness differs according to time from viral symptom onset to ICU admission, we assessed patient characteristics and outcomes in a cohort of 379 critically ill patients admitted to four university-affiliated hospitals in Paris.
Patients and methods
This retrospective observational study was performed in four university-affiliated hospitals in Paris. Consecutive patients with laboratory-confirmed SARS-CoV-2 infection admitted to one of the ICUs between 21 February and 24 April 2020 were enrolled. The appropriate ethics committee approved the study and waived the need for informed consent in accordance with French legislation about retrospective studies.
Laboratory confirmation of SARS-Cov-2 was defined as a positive real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasal and pharyngeal swabs [18].
The four participating ICUs applied local (Parisian) guidelines regarding ICU admission, the provision of standard of care (including sedation, and neuromuscular blockade), the use of non-invasive ventilation, antibiotic treatment, as well as the use of rescue therapies for refractory hypoxemia (prone positioning, ECMO, etc.). These guidelines were approved by all and shared on the Health Regional Agency website (https://www.iledefrance.ars.sante.fr/coronavirus-covid-19-information-aux-professionnels-de-sante). There were no guidelines regarding the use of anti-viral agents, steroids, or cytokine-blockade that were mostly used in RCTs, sometimes through TUA (temporary use authorisation) or upon clinician’s decisions.
Data were recorded by the intensivists in each ICU. The variables reported in the tables and figures were abstracted from the medical charts and electronic reports. Chronic obstructive pulmonary disease was defined as previously reported [19] and acute kidney injury according to the operational decision [20]. Causes of immunosuppression included solid tumours, haematological malignancies, solid organ transplantation, long-term immunosuppressive therapy (i.e., high-dose steroids (> 1 mg/kg whatever the duration) or any immunosuppressant for more than 3 months), and HIV infection [21]. Obesity was defined as previously reported [22]. The SOFA score was calculated within 24 h of ICU admission [23].
Time from viral symptom onset to ICU admission was defined as the number of days between the onset of flu-like viral symptoms (fever or chills, cough, sore throat, runny nose, anosmia, muscle pain, body aches, headaches, fatigue, vomiting or diarrhoea) and the day of ICU admission. In patients who were intubated and sedated, and unable to respond, relatives were asked to provide the detailed medical history. Otherwise, data were retrieved from the medical charts from the emergency department, outpatient consults, general practitioner or medicalised ambulances. Time from viral symptom onset to hospitalisation or from hospitalisation to ICU admission was calculated as number of days between viral symptom onset or admission to the hospital, and ICU admission.
Patient status at ICU and hospital discharge was recorded on 15 May 2020. ICU length of stay was recorded.
Statistical analysis
Continuous variables are described as median (interquartile range [IQR]) and compared between groups using the non-parametric Wilcoxon rank-sum test. Categorical variables are described as frequency (percentages) and compared between groups using Fisher’s exact test. Mortality was assessed using survival analysis.
The patients were categorised according to the number of days between disease onset (i.e., the number of days between viral symptoms onset) and ICU admission (< 8, 8–14, and > 14 days).
Independent risk factors for day-28 mortality were identified using a Cox model. Conditional stepwise variable selection was performed with 0.2 as the critical p value for entry into the model and 0.1 as the p value for removal. Interactions and correlations between the explanatory variables, the validity of the proportional hazards assumption, the influence of outliers, and linearity of the relationship between the log hazard and the covariates were carefully checked. For the first step of the variable selection process, age, comorbidities (asthma, diabetes, COPD, hypertension, immunosuppression), time from viral symptom onset to ICU admission, acute kidney injury, and troponin were included in the model.
Kaplan–Meier graphs were used to express the probability of death from ICU admission to day 28. Comparisons were performed using the log-rank test.
In a sensitivity analysis, a double adjustment was performed. First, patients were matched on risk factors for ICU admission within the first 7 days of COVID-19. Then, a propensity score (PS)-matched analysis was performed on the risk of ICU admission within 7 days after viral symptom onset. Variables were selected to the PS model if associated with p < 0.2; they included comorbidities (asthma, hypertension, heart failure), body temperature at admission, and acute kidney injury. Case-matching was with a 1:1 ratio, without replacement, and according to the nearest neighbour method. Adequacy of the matching procedure was assessed by plotting PS across groups and computing the standardised mean difference. A univariate analysis was performed, and a Cox model was then built with double adjustment on relevant variables that were associated with the outcome and poorly matched.
Centre effect was assessed by a random effects model
The missing data rate was 7.3% overall and < 5% for major outcomes or covariates. Imputation of missing data was not performed.
Statistical analyses were performed with R statistical software, version 3.4.3 (available online at https://www.r-project.org/), using the ‘Survival’ and ‘MatchIt’ packages. Values of p < 0.05 were considered significant.
Results
We included 379 patients admitted between February 21 and April 24 2020. Table 1 reports their main features. All but 35 (9.2%) patients had at least one comorbidity, and the main comorbidities were obesity and overweight (31.2 and 36%, respectively), hypertension (49.6%), and diabetes (30.1%). Time from viral symptom onset to ICU admission had a median of 8 [6–11] days overall and was ≤ 7 days in 161 (42.5%) patients, 8–14 days in 173 (45.6%) patients, and more than 14 days in 42 (11.1%) patients. The information was missing for three patients. At ICU admission, digestive viral symptoms were present in 99 (26.1%) patients.
At ICU admission, temperature was 38 °C [37–38.7], oxygen flow was 15 [9–15] L/min, and the SOFA score was 5 [3–8]. The number of quadrants involved on the chest radiograph was 4 [2–4]. Initial computed tomography angiography disclosed pulmonary embolism in 42 (14%) patients. Initial oxygenation management included continuous positive airway pressure in six (1.6%) patients, noninvasive ventilation in 27 (7.1%) patients, high-flow nasal oxygen in 146 (38.5%) patients, and standard oxygen in the remaining 200 patients. Overall, 257 (67.8%) patients were intubated (at a median time from ICU admission of 0 days [0–1]). The median PaO2/FiO2 ratio on day 1 was 127 [89–193]. Extracorporeal membrane oxygenation was needed in 25 (6.6%) patients. Clinically or microbiologically documented bacterial infection developed in 63 (19.8%) patients. Vasopressors were used in 165 (43.8%) patients. Among the 195 (51.5%) patients with acute kidney injury, 74 (19.5%) required renal replacement therapy. ICU stay length was 10 [5–21] days. ICU, hospital, and day-28 mortality rates were 31% (n = 98), 39% (n = 103), and 26% (n = 100), respectively. On 15 May 2020, 103 (27%) patients were still hospitalised.
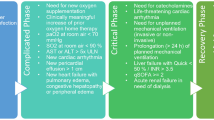
As shown in Fig. 1, day-28 mortality decreased with increasing time from viral symptom onset to ICU admission. Patients admitted within a week after viral symptom onset had a higher day-28 mortality rate than did those admitted in the second or third week after viral symptom onset (Figs. 2 and 3). Tables 1 and 2 compare patient characteristics across the three groups. Patients admitted within the first week were more often treated for hypertension and more often febrile at ICU admission; also, their radiographic lung involvement was more limited compared to that in the other two groups. Patients admitted in the first week less often received high-flow nasal oxygen; they had a higher prevalence of acute kidney injury and more often required renal replacement therapy during the ICU stay.
Among the 379 patients, 30% had an associate bacterial infection, including 9.4% with a SARS-CoV-2 superinfection and 20% with hospital acquired infections. Superinfections were diagnosed at the time of SARS-CoV-2 diagnosis in 50 patients and were related to S aureus (n = 16), other Staphylococcus sp. (n = 5), H. influenzae (n = 5), E Coli (n = 4), K. pneumonia (n = 5), P. aeruginosa (n = 3), Enterobacter sp. (n = 2), Citrobacter sp. (n = 3), Serratia sp. (n = 3), and M. catarrhalis (n = 4).
Factors associated with day-28 mortality included time since viral symptom onset: 36.7% vs. 20.8% vs. 11.9% patients died in the groups admitted within 0–7 days, 8–14 days, or > 14 days after viral symptom onset, respectively (p < 0.0001); other factors were older age (66 y [57–72] in patients who died vs. 60 y [52–67] in patients who survived, p < 0.0001), COPD (12% vs. 2.9%, p = 0.001), hypertension (65% vs. 44%, p = 0.001), diabetes (45% vs. 25%, p < 0.0001), immunodeficiency (29% vs. 14%, p = 0.001), heart failure (14% vs. 6%, p = 0.03), chronic kidney disease (30% vs. 12%, p < 0.0001), SOFA score at ICU admission (7 [5–10] vs. 4 [3–7], p < 0.0001), acute kidney injury (73% vs. 44%, p = 0.001), platelet count (166 × 109/L [135–236] vs. 221 × 109/L [168–284], p < 0.0001), procalcitonin (0.72 ng/mL [0.40–1.57] vs. 0.42 ng/mL [0.18–1.06], p = 0.001), normal troponin concentration at admission (41% vs. 68%, p < 0.0001), need for invasive mechanical ventilation (80% vs. 61%, p < 0.0001), need for vasopressors (69% vs. 34%, p = 0.001), and need for renal replacement therapy (39% vs. 12%, p = 0.001).
By multivariable Cox proportional analysis, factors independently associated with day-28 mortality were age, COPD, immunocompromised status, time from viral symptom onset to ICU admission, normal troponin at ICU admission, and acute kidney injury (Table S1).
There was no centre effect in this study. For instance, when adding to our final model in the whole population a random effects model for the centre effect, our results were unchanged (HR for time since viral symptom onset 8–14 days: 0.51; 95% CI 0.32–0.80; HR for time > 14 days: 0.39; 95% CI 0.15–0.98).
In the paired matched analysis, 140 patients admitted within the first week after viral symptom onset were matched to 140 controls. Day-28 mortality was 36.4% in the group admitted within a week after disease onset and 21.4% in the group of patients admitted later (Fig. S1, p = 0.001). The multivariable Cox proportional model in the 280 paired patients showed that determinants of day-28 mortality were age (hazard ratio [HR], 1.04/year; 95% confidence interval [95% CI] 1.01–1.06, p = 0.0004), ICU admission more than 7 days after disease onset (HR 0.53; 95% CI 0.34–0.84; p = 0.007), SOFA score at ICU admission (HR, 1.11/point; 95% CI, 1.03–1.19; p = 0.006), and normal troponin (HR 0.64; 95% CI 0.39–1.06; p = 0.05).
In an exploratory analysis in 100 patients from our cohort (Table S2), concentrations of cytokines including IL6 and IL8 varied significantly across the three patient groups.
Discussion
Identifying the determinants of outcomes of critically ill patients with severe COVID-19 is vital to optimise the use of ICU and other hospital resources. This study collecting data from 379 COVID-19 patients showed that mortality decreased with increasing time from viral symptom onset to ICU admission. Mortality was significantly higher in patients admitted to the ICU within a week after viral symptom onset, independently from acute illness severity at ICU admission. These findings may help to guide the clinical management. They may also be useful for the identification and rational design of effective therapies.
Interestingly, apart from the prevalence of hypertension, the baseline patient characteristics (age, sex, body mass index, hypoxaemia severity at admission, and inflammation) were mostly similar across the three patient groups defined by viral symptom duration at ICU admission. The severity of respiratory failure as assessed by the PaO2/FiO2 ratio at admission was not significantly different across the three groups. In contrast, the group with early ICU admission had a worse SOFA score value and a higher prevalence of acute kidney injury, suggesting that the increased mortality was related to early multi-organ dysfunction, as opposed to only severe lung involvement. The significantly smaller number of lung quadrants involved in the early admission group supports this possibility. SARS-CoV-2 can bind to many target organs via the angiotensin-converting enzyme 2 receptor. The virus predominantly infects airway and alveolar epithelial cells, but can also infect vascular endothelial cells and macrophages [24]. SARS-CoV-2 viral particles and genome have been detected in monocytes and lymphocytes [25]. The aggressive inflammation induced by viral replication not only generates type II pneumocyte apoptosis and severe respiratory distress related to cytokine-induced fluid leakage, but also induces a cytokine storm with multi-organ failure.
Three lines of evidence seem to support a two-hit model in which an initial insult related to viral replication and responsible for inflammation and injury to multiple organs is followed by a second insult related to exaggerated cytokine production by both epithelial and endothelial cells. First, in a study of 476 patients admitted in Wuhan, Shanghai, and Anhui, the time from viral symptom onset to the first positive RT-PCR test was shorter in the group with critical illness than in the groups with moderate or severe illness [9]. Second, virus-induced alveolar cell death and the accumulation of apoptotic and necrotic cellular debris have been reported to first elicit a pro-inflammatory response from the macrophages then to result in the production of large amounts of eicosanoids, which in turn stimulate the production of pro-inflammatory cytokines by immune cells such as macrophages [26]. Thus, the eicosanoid storm induces a cytokine storm, which promotes further leucocytosis and immune-cell infiltration. Last, a study of 150 patients from Wuhan showed that the survival time from viral symptom onset to death had two peaks, at about 14 and 22 days, respectively, in keeping with our findings in patients having a length of stay of about 10 days [27]. Strikingly, 40% of the patients who died had myocardial damage [27], a finding consistent with the higher troponin levels in the patients who died compared to survivors in our study. The contribution of fulminant myocarditis to increased mortality in patients admitted within a week of disease viral symptoms deserves further investigation.
This study has several limitations. First, the retrospective design limits the interpretation of the findings. However, few data were missing (7.3%). Moreover, with 379 critically ill patients managed in four centres, this study is among the largest to date. The largest study to date of critically ill COVID-19 patients [10] emphasised the association of older age with short-term mortality, but did not separate outcomes according to time since viral symptom onset. Second, the excess mortality in patients admitted to the ICU within 7 days after viral symptom onset was associated with an increased prevalence of non-respiratory injury and, more specifically, of acute kidney and myocardial injury. However, we did not specifically assess causes of death. Third, although markers for inflammation were available for all 379 patients, cytokine and lymphocyte typing data were obtained in only 100 patients. Our results suggest that targeting IL-6 might be most effective in patients admitted earlier after viral symptom onset. However, this possibility requires further assessment. Moreover, sensitivity analyses of the results of ongoing anti-IL6 trials should also explore whether IL6 blockade is most beneficial in those patients admitted to the ICU within a week after viral symptom onset.
In summary, excess mortality occurred in patients admitted to the ICU within a week after COVID-19 onset. This excess mortality was not related to more severe respiratory disease but, instead, to worse dysfunction of other organs and, more specifically, to acute kidney and myocardial injury. Studies to investigate the extent of organ injuries at each stage of the disease are warranted. Interventions including antiviral, anti-inflammatory, or targeted therapies that are currently used in patients with SARS-CoV-2 might impact different clinical endpoints according to time since viral symptom onset.
References
Wu F, Zhao S, Yu B et al (2020) A new coronavirus associated with human respiratory disease in China. Nature 579:265–269. https://doi.org/10.1038/s41586-020-2008-3
Zhu N, Zhang D, Wang W et al (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733. https://doi.org/10.1056/NEJMoa2001017
Chen Y, Liu Q, Guo D (2020) Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol 92:418–423. https://doi.org/10.1002/jmv.25681
Nie X, Fan L, Mu G et al (2020) Epidemiological characteristics and incubation period of 7015 confirmed cases with coronavirus disease 2019 outside Hubei Province in China. J Infect Dis. https://doi.org/10.1093/infdis/jiaa211
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet Lond Engl 395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Guan W-J, Ni Z-Y, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. n Engl J Med 382:1708–1720. https://doi.org/10.1056/NEJMoa2002032
Phua J, Weng L, Ling L et al (2020) Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. https://doi.org/10.1016/S2213-2600(20)30161-2
Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 hospitalized patients With 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323:1061–1069. https://doi.org/10.1001/jama.2020.1585
Feng Y, Ling Y, Bai T et al (2020) COVID-19 with different severity: a multi-center study of clinical features. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.202002-0445OC
Grasselli G, Zangrillo A, Zanella A et al (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 323:1574–1581. https://doi.org/10.1001/jama.2020.5394
Du RH, Liu LM, Yin W et al (2020) Hospitalization and critical care of 109 decedents with COVID-19 pneumonia in Wuhan, China. Ann Am Thorac Soc. https://doi.org/10.1513/AnnalsATS.202003-225OC
Fu Y, Cheng Y, Wu Y (2020) Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin. https://doi.org/10.1007/s12250-020-00207-4
Sun X, Wang T, Cai D et al (2020) Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. https://doi.org/10.1016/j.cytogfr.2020.04.002
Andersson U, Ottestad W, Tracey KJ (2020) Extracellular HMGB1: a therapeutic target in severe pulmonary inflammation including. Mol Med Camb Mass 26:42. https://doi.org/10.1186/s10020-020-00172-4
Mo P, Xing Y, Xiao Y et al (2020) Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis Off Publ Infect Dis Soc Am. https://doi.org/10.1093/cid/ciaa270
Barnes BJ, Adrover JM, Baxter-Stoltzfus A et al (2020) Targeting potential drivers of COVID-19: neutrophil extracellular traps. J Exp Med. https://doi.org/10.1084/jem.20200652
Chen X, Zhao B, Qu Y et al (2020) Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clin Infect Dis Off Publ Infect Dis Soc Am. https://doi.org/10.1093/cid/ciaa449
Alhazzani W, Møller MH, Arabi YM et al (2020) Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. https://doi.org/10.1007/s00134-020-06022-5
Rennard SI, Drummond MB (2015) Early chronic obstructive pulmonary disease: definition, assessment, and prevention. Lancet Lond Engl 385:1778–1788. https://doi.org/10.1016/S0140-6736(15)60647-X
Thomas ME, Blaine C, Dawnay A et al (2015) The definition of acute kidney injury and its use in practice. Kidney Int 87:62–73. https://doi.org/10.1038/ki.2014.328
Azoulay E, Mokart D, Kouatchet A et al (2019) Acute respiratory failure in immunocompromised adults. Lancet Respir Med 7:173–186. https://doi.org/10.1016/S2213-2600(18)30345-X
Kass DA, Duggal P, Cingolani O (2020) Obesity could shift severe COVID-19 disease to younger ages. Lancet Lond Engl. https://doi.org/10.1016/S0140-6736(20)31024-2
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Zhang Y, Geng X, Tan Y et al (2020) New understanding of the damage of SARS-CoV-2 infection outside the respiratory system. Biomed Pharmacother 127:110195. https://doi.org/10.1016/j.biopha.2020.110195
Merad M, Martin JC (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. https://doi.org/10.1038/s41577-020-0331-4
Panigrahy D, Gilligan MM, Huang S et al (2020) Inflammation resolution: a dual-pronged approach to averting cytokine storms in. Cancer Metastasis Rev. https://doi.org/10.1007/s10555-020-09889-4
Ruan Q, Yang K, Wang W et al (2020) Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 46:846–848. https://doi.org/10.1007/s00134-020-05991-x
Acknowledgements
The SARS-CoV-2 outbreak has been particularly challenging for patients, relatives, healthcare providers, and all others involved. We are indebted to all for their willingness to participate in combatting this health disaster.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
EA, AD, AVB and MF have designed the study and guided the analyses. All authors have significantly contributed to the research, have discussed the results of the analyses, have edited the final version of the manuscript and have agreed with the submitted version.
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors has any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2020_6202_MOESM1_ESM.docx
Supplementary file1 (DOCX Supplemental Fig. 1: Survival probability in patients admitted before or after 7 days since viral symptom onset in a matched paired cohort of 308 patients 102 kb)
Rights and permissions
About this article
Cite this article
Azoulay, E., Fartoukh, M., Darmon, M. et al. Increased mortality in patients with severe SARS-CoV-2 infection admitted within seven days of disease onset. Intensive Care Med 46, 1714–1722 (2020). https://doi.org/10.1007/s00134-020-06202-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-06202-3