Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11237
Peer-review started: July 18, 2021
First decision: October 11, 2021
Revised: October 11, 2021
Accepted: November 14, 2021
Article in press: November 14, 2021
Published online: December 26, 2021
The onset symptoms of people infected by Chlamydia psittaci can mimic the coronavirus disease 2019 (COVID-19). However, the differences in laboratory tests and imaging features between psittacosis and COVID-19 remain unknown.
To better understand the two diseases and then make an early diagnosis and treatment.
Six patients from two institutions confirmed as psittacosis by high-throughput genetic testing and 31 patients confirmed as COVID-19 were retrospectively included. The epidemiology, clinical characteristics, laboratory tests and computed tomography (CT) imaging features were collected and compared between the two groups. The follow-up CT imaging findings of patients with psittacosis were also investigated.
The white blood cell count (WBC), neutrophil count and calcium were more likely to be decreased in patients with COVID-19 but were increased in patients with psittacosis (all P = 0.000). Lymphocyte count and platelet count were higher in patients with psittacosis than in those with COVID-19 (P = 0.044, P = 0.035, respectively). Lesions in patients with psittacosis were more likely to be unilateral (P = 0.001), involve fewer lung lobes (P = 0.006) and have pleural effusions (P = 0.002). Vascular enlargement was more common in patients with COVID-19 (P = 0.003). Consolidation in lung CT images was absorbed in all 6 patients.
Psittacosis has the potential for human-to-human transmission. Patients with psittacosis present increased WBC count and neutrophil count and have specific CT imaging findings, including unilateral distribution, less involvement of lung lobes and pleural effusions, which might help us to differentiate it from COVID-19.
Core Tip: In patients with coronavirus disease 2019 (COVID-19) the white blood cell count, neutrophil count and calcium were more likely to be decreased. Lymphocyte count and platelet count were higher in patients with psittacosis than those with COVID-19. Lesions in patients with psittacosis were more likely to be unilateral and involve less lung lobes and have pleural effusions.
- Citation: Zhao W, He L, Xie XZ, Liao X, Tong DJ, Wu SJ, Liu J. Clustering cases of Chlamydia psittaci pneumonia mimicking COVID-19 pneumonia. World J Clin Cases 2021; 9(36): 11237-11247
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11237.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11237
Since the new “unknown viral pneumonia” was detected in Wuhan, later named coronavirus disease 2019 (COVID-19), the outbreak of COVID-19 has rapidly spread to other cities in China and other countries and has posed a huge challenge to the global health system[1]. Many efforts have been made by medical staff worldwide to fight the disease. The situation of COVID-19 has been controlled in China; however, it is still serious in several countries, such as America and Brazil[2]. Considering the potential to import cases, Chinese people and the government are still enacting strict prevention and control measures, especially in hospitals.
The epidemiology, clinical characteristics, and imaging features have been substantially reported recently[3-6], which has helped us to better understand and fight the disease. Fever is one of the most common onset symptoms[5] but is nonspecific. Other infections caused by other viruses, bacteria, and fungi may also present fever in clinical practice, making it difficult to accurately screen out patients with COVID-19. Psittacosis, a zoonotic infectious disease caused by the bacterium Chlamydia psittaci (C. psittaci), is rarely diagnosed in the clinic. Humans can become infected through inhalation of aerosolized bacteria when exposed to infected birds or handling contaminated feathers, fecal material or carcasses[7,8]. The onset symptoms of people infected by C. psittaci include fever, chills, headache, malaise, myalgia, nonproductive coughing and dyspnea[9], which can mimic COVID-19. However, the differences in laboratory tests and imaging features between psittacosis and COVID-19 remain unknown.
Here, we report two clusters of cases with C. psittaci infection mimicking COVID-19 with the aims of better understanding the two diseases, making an early diagnosis and providing treatment. We hope this experience may contribute to fighting the COVID-19 outbreak.
This retrospective study was approved by our Medical Ethical Committee (Approved No. 2020024), which waived the requirement for patients’ informed consent.
Four medical staff members who were working in the emergency rescue area or viewing area in the Second Xiangya Hospital (Cluster 1) and two slaughterhouse staff members treated in the First People’s Hospital of Yueyang (Cluster 2), who were confirmed to have C. psittaci pneumonia, were included in the current study. All of the patients presented onset symptoms of fever and underwent severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing using real-time reverse transcription-polymerase chain reaction (RT-PCR). The IgG and IgM of COVID-19 were also tested. Moreover, the bronchoalveolar lavage fluid (BALF) of four patients was collected to identify suspicious pathogenic microorganisms (PMseq-DNA+RNA respiratory system infection pathogenic microbes high-throughput genetic testing: DNA testing, BGI), including 6350 species of bacteria with known sequences (including 174 species of mycobacteria and 137 species of mycoplasma/chlamydia/rickettsia), 1798 DNA viruses, 1064 fungi and 234 parasites. The number of detected sequences of C. psittaci was also recorded for each patient. The epidemiology, clinical characteristics, and laboratory tests (upon first admission) were also collected. In Cluster 1, one of the four patients had taken medicine before high-throughput genetic testing. Moreover, another patient who presented the same symptoms was identified as suspected patient 0 (patient 0 in Cluster 1). However, this patient only underwent RT-PCR testing for COVID-19 and was not confirmed to have C. psittaci by high-throughput genetic testing. In Cluster 2, one patient confirmed with C. psittaci by high-throughput genetic testing was identified as suspected patient0 (patient 0 in Cluster 2). However, the patient was admitted to another hospital, and the medical history was unavailable.
Confirmed COVID-19 patients from January 23, 2020 to February 10, 2020 in the Second Xiangya Hospital were also collected and compared with patients with C. psittaci. The diagnosis of COVID-19 was determined according to at least two positive results by real-time reverse-transcription-polymerase chain reaction (RT-PCR) assay for COVID-19. The epidemiology, clinical characteristics, computed tomography (CT) images, and laboratory tests were collected.
Four patients underwent two CT scans with the Somatom go Now scanner (Siemens Medical, Shanghai, China). The CT images were reviewed blindly and independently by two radiologists (with 5 and 15 years of experience) in consensus. The detailed imaging interpretations were described in our previous studies[6,10].
Continuous variables were compared with the Mann-Whitney U test and are presented as the medians (IQR). Categorical variables are presented as the numbers (%) and were compared by Fisher’s exact test between the psittacosis and COVID-19 groups. A two-sided P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (version 24.0).
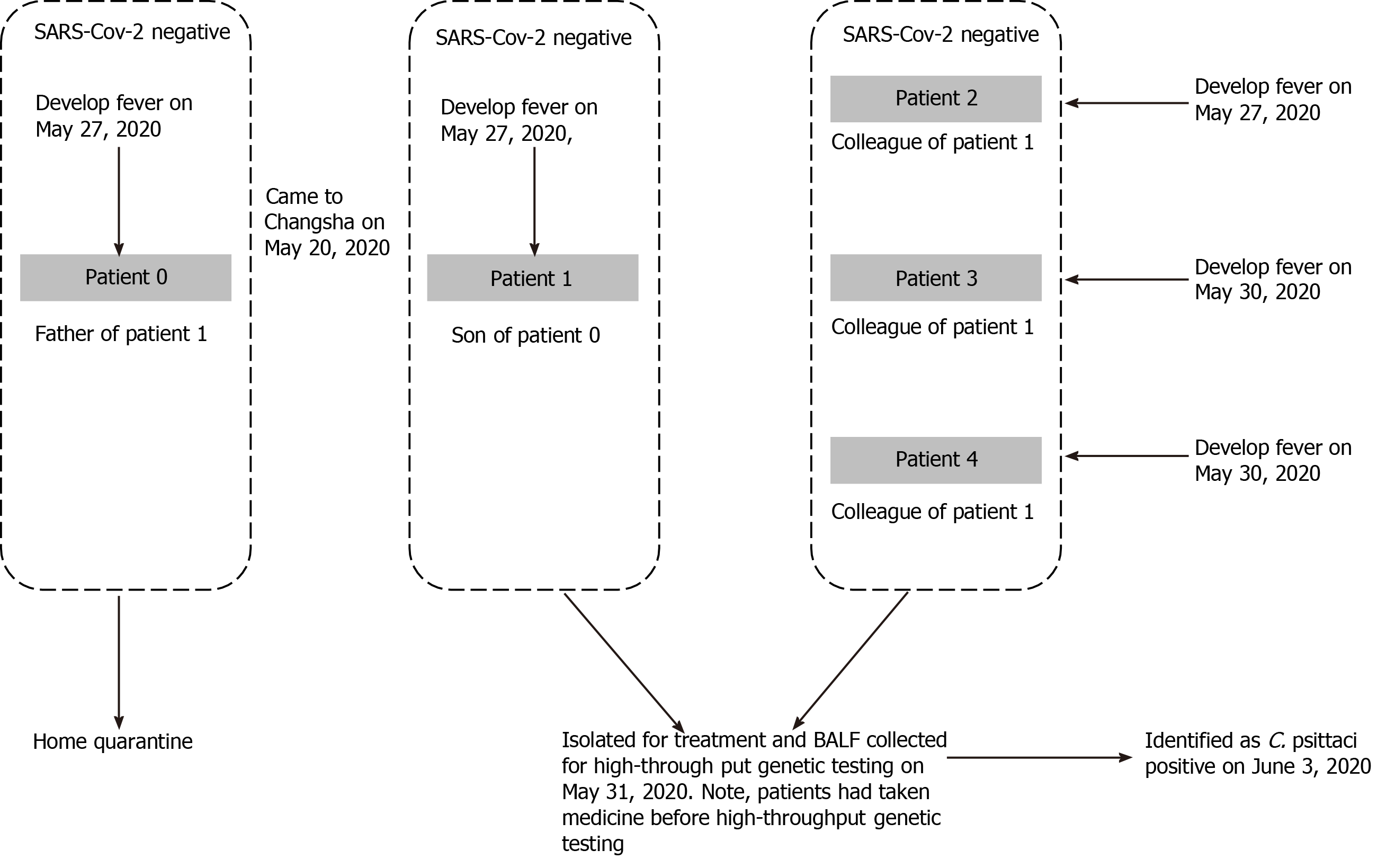
All of the included patients had an onset symptom of fever, and the relationship and chronology of symptom onset in the two clusters are described in Figure 1. In Cluster 1, potential patient 0, who had an exposure history to poultry, visited his son on May 20, 2020. The last time they had been together was May Day. On May 27, 2020, they all developed fever symptoms and went to the fever clinic for COVID-19 screening. On the same day, they underwent chest CT scanning. From May 20 to May 27, Patient 1 worked in our hospital as usual and had direct contact with Patient 2, Patient 3, and Patient 4. Patients 2-4 successively developed fever. All five patients were identified as SARS-CoV-2 negative (all confirmed by RT-PCR and IgG, IgM testing), and the BALF of Patients 1-4 was collected for high-throughput genetic testing; all were identified as C. psittaci-positive. Note that patient 2 had taken medicine before high-throughput genetic testing. In Cluster 2, all patients were slaughterhouse staff and had a direct exposure history to poultry. The potential Patient 0 first developed fever, and Patients1 and Patients2 subsequently developed similar symptoms on April 24 and 27. All three patients were identified as C. psittaci-positive by high-throughput genetic testing.
From January 23, 2020 to February 10, 2020, 31 patients were confirmed to be COVID-19-positive in our hospital. The clinical characteristics and laboratory tests of patients with COVID-19 and psittacosis are described and compared with those of patients with C. psittaci in Table 1. Due to the uncertain diagnosis for patient 0, we only analyzed the clinical factors of patients 1-4 in Cluster 1 and patients1-2 in Cluster 2. Therefore, the clinical information of patient 01 was only considered as a reference. In terms of age, there were no significant differences between the two groups. The greatest differences between the two groups were the WBC count and neutrophil count (P = 0.000), which presented an opposite change trend. The white blood cell count and neutrophil count were more likely to be decreased in patients with COVID-19 but were increased in patients with psittacosis. Lymphocyte count and platelet count were higher in patients with psittacosis than in those with COVID-19 (P = 0.044, P = 0.035, respectively). C-reactive protein (CRP) was increased in both groups and was more remarkable in patients with psittacosis (P = 0.035). Calcium was higher in patients with COVID-19 than in those with psittacosis (P = 0.000).
| Patient 0 | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient1 | Patient2 | Psittacosis (n = 6) | COVID-19 (n = 31) | P value | |
| Age | 62 | 36 | 29 | 32 | 26 | 47 | 48 | 34.00 (28.25-47.25) | 50.00 (32.00-66.00) | 0.073 |
| Sex | Male | Male | Female | Female | Male | Male | Male | NA | NA | 0.660 |
| Male | 4 | 16 | ||||||||
| Female | 2 | 15 | ||||||||
| Hemoglobin (g/dL); (male normal range 130-175; female normal range 115-150) | 124 | 142 | 135 | 134 | 163 | 157 | 143 | 142.50 (134.75-158.50)a | 135.00 (120.00-141.00) | 0.054 |
| White blood cell count (× 109/L); (normal range 3.5-9.5) | 7.14 | 10.43 | 10.07 | 11.7 | 10.53 | 10.26 | 14.36 | 10.48 (10.21-12.37) | 4.62 (3.31-6.17) | 0.000 |
| Neutrophil count (× 109/L); (normal range 1.8-6.3) | 5.92 | 7.57 | 6.61 | 8.66 | 8.41 | 6.3 | 11.76 | 7.99 (6.53-9.44) | 2.89 (1.95-3.89) | 0.000 |
| Lymphocyte count (× 109/L); (normal range 1.1-3.2) | 0.66 | 2.04 | 2.33 | 2.21 | 1.11 | 1.28 | 1.43 | 1.74 (1.24-2.24) | 1.09 (0.71-1.67) | 0.044 |
| Platelet count (× 109/L); (normal range 125-350) | 186 | 369 | 249 | 241 | 193 | 214 | 204 | 227 (201-279) | 183 (124-227) | 0.035 |
| Eosinophilic count (× 109/L); (normal range 0.02-o.52) | 0 | 0.1 | 0.01 | 0 | 0 | 0 | 0 | 0.000 (0.000-0.325) | 0.100 (0.000-0.400) | 0.265 |
| C-reactive protein (mg/L); (normal range 0.0-5.0) | 127.17 | 12.17 | 31.87 | 50.55 | 58.01 | 112.13 | 141.35 | 54.28 (26.95-119.44) | 15.60 (4.77-47.73) | 0.035 |
| Sodium (mmol/liter) | NA | 140.9 | 1136.2 | 134.2 | 136.1 | 129.7 | 137.4 | 136.15 (133.08-138.28) | 135.90 (133.40-137.40) | 0.857 |
| Potassium (mmol/liter) | NA | 4.09 | 3.42 | 3.42 | 3.94 | 4.11 | 3.52 | 3.73 (3.42-4.10) | 4.02 (3.58-4.37) | 0.302 |
| Calcium (mmol/liter) | NA | 2.11 | 2.28 | 2.03 | 2 | 2.2 | 2.16 | 2.14 (2.02-2.22) | 1.20 (1.18-1.22) | 0.000 |
| The number of detected sequences of C. psittaci | NA | 274 | 3 | 82 | 254 | NA | NA | NA | NA | NA |
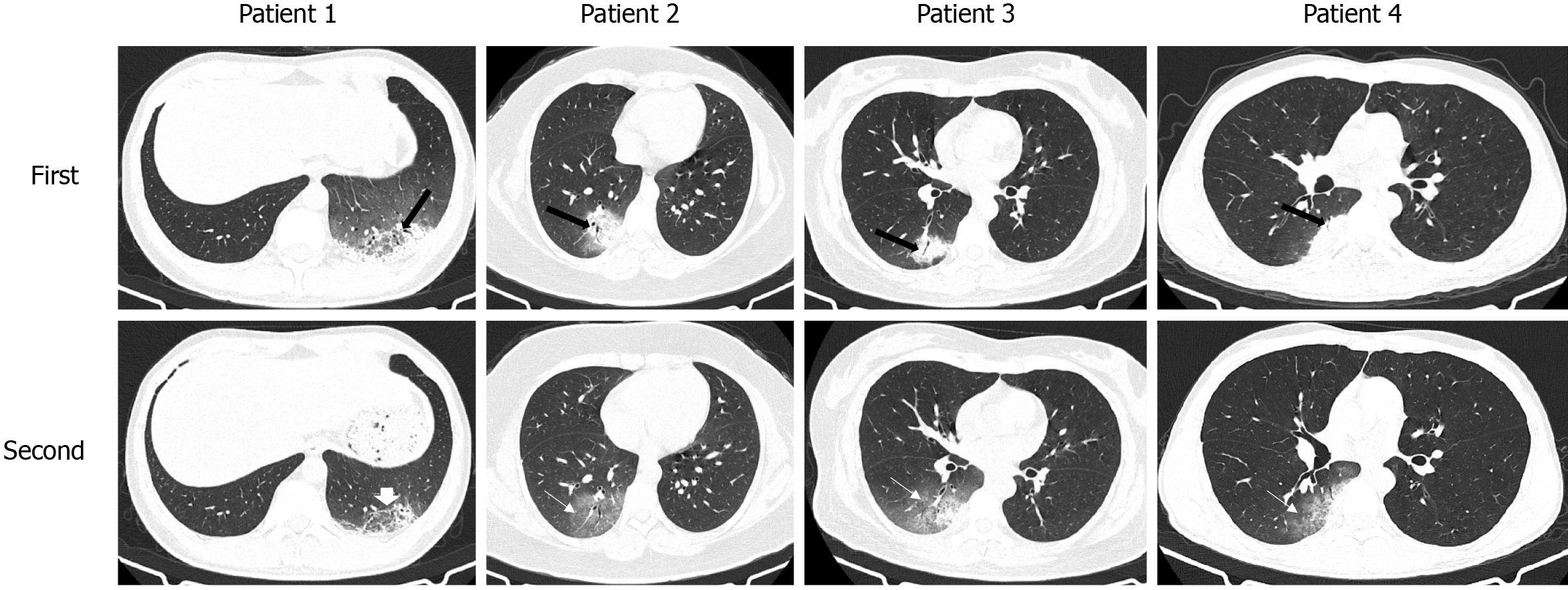
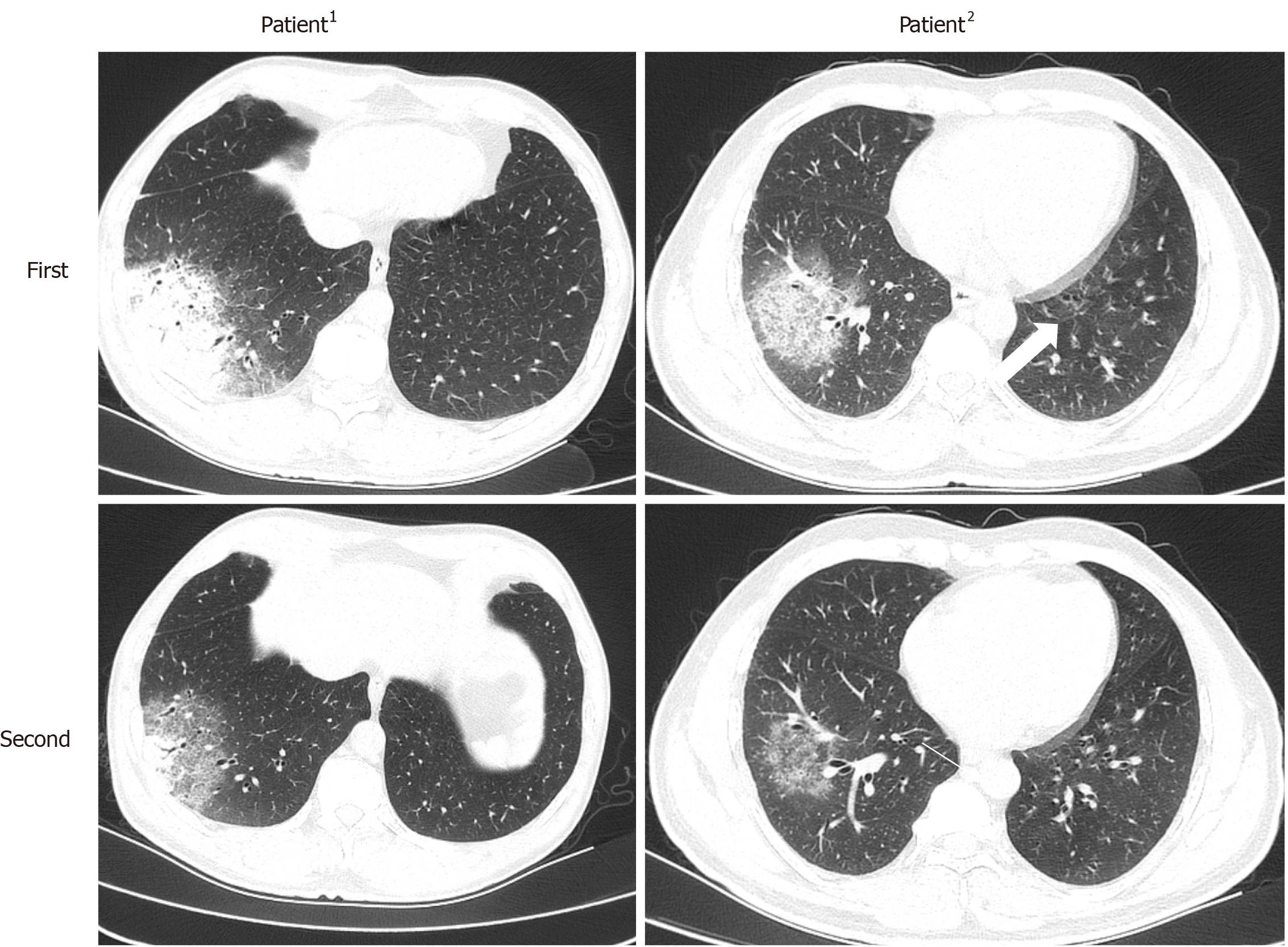
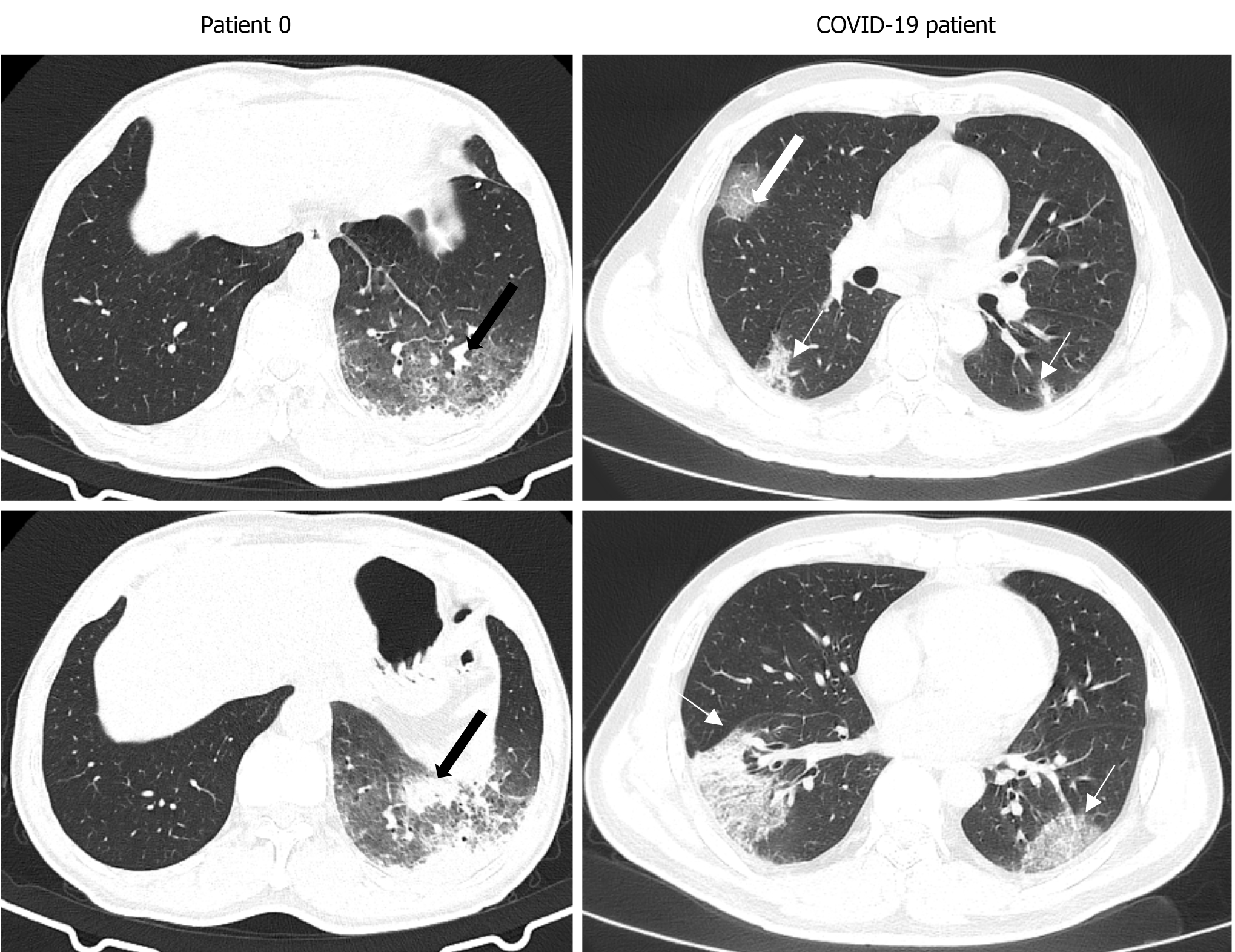
All six confirmed patients underwent CT scanning, and 15 of 31 patients with COVID-19 underwent CT scanning. The imaging findings of the patients in the two groups are presented and compared in Table 2. Note that 2 of 15 patients with COVID-19 presented normal CT findings. Lesions in patients with psittacosis were more likely to be unilateral (P = 0.001) and involve fewer lung lobes (P = 0.006) than those infected by COVID-19 (Figures 2, 3 and 4). Vascular enlargement was more common in patients with COVID-19 (P = 0.003) (Figure 4), whereas pleural effusions were more common in patients with psittacosis (P = 0.002). Although there was no significant difference regarding the predominant lesion type between the two groups, pure ground-glass opacity was not seen in patients with psittacosis. All of the lesions in patients with psittacosis were located in lower lung lobes. The transverse distribution, air bronchogram, margin and reticulation were not significantly different between the two groups. Note that the imaging findings of patient 0 were similar to those of patients 1-4 (Figure 3). Moreover, patients 0 and 1 presented a larger lesion area than patients 2-4.
| Psittacosis (n = 6) | COVID-19 (n = 13) | P value | |
| Predominant lesion type | 0.221 | ||
| GGO | 0 (0) | 5 (38.5) | |
| Consolidation | 3 (50) | 5 (38.5) | |
| Mixed GGO and consolidation | 3 (50) | 3 (23.1) | |
| Air bronchogram | 6 (100) | 8 (61.5) | 0.128 |
| Vascular enlargement | 1 (16.7) | 12 (92.3) | 0.003 |
| Margin (uneasily differentiated) | 6 (100) | 8 (61.5) | 0.128 |
| Reticulation | 5 (75) | 9 (69.2) | 1.000 |
| Pleural effusions | 6 (100) | 1 (7.7) | 0.002 |
| Craniocaudal distribution | 0.026 | ||
| Upper lung predominant | 0 (0) | 2 (15.4) | |
| Lower lung predominant | 6 (100) | 4 (30.8) | |
| No craniocaudal distribution | 0 (0) | 7 (53.8) | |
| Transverse distribution | 0.255 | ||
| Central | 0 (0) | 0 (0) | |
| Peripheral | 6 (100) | 9 (69.2) | |
| No transverse distribution | 0 (0) | 4 (30.8) | |
| Lung region distribution | 0.001 | ||
| Unilateral | 6 (100) | 2 (15.4) | |
| Bilateral | 0 (0) | 11 (84.6) | |
| Number of involved lung lobes | 0.006 | ||
| 1 | 6 (100) | 2 (15.4) | |
| 2 | 0 (0) | 3 (23.1) | |
| 3 | 0 (0) | 0 (0) | |
| 4 | 0 (0) | 5 (38.5) | |
| 5 | 0 (0) | 5 (38.5) |
All patients with psittacosis were treated with piperacillin and moxifloxacin, and the symptoms were relieved. Consolidation in lung CT images was absorbed in all 6 patients; however, patients 2-4 had an increased involvement area and presented with ground-glass opacity (GGO) (Figures 2 and 3). Other people who had close contact with patients 1-4 excluded C. psittaci infection based on clinical symptoms. No further similar cases were found in any of the staff in the screening ward and their family members, nor did nosocomial infection related to the six cases occur.
In this study, we report a cluster of 4 cases (medical staff) confirmed with psittacosis. The clinical characteristics, laboratory tests and CT imaging findings were investigated and compared with patients confirmed to have COVID-19. Patients with psittacosis were more likely to present increased WBC count and neutrophil count and have specific CT imaging findings, including unilateral distribution and less involvement of lung lobes and pleural effusions.
The outbreak of COVID-19 is still ongoing around the world and threatens global public health. Although recent studies have made progress on vaccines for SARS-CoV-2[11,12], early diagnosis, which could prevent the spread of the virus, avoid cross-infection and promote early treatments, remains the best strategy to fight the disease. Fever, clustering outbreaks and pneumonia all favor potential infection by SARS-CoV-2. However, infections caused by other pathogenic factors also need attention. Psittacosis is a sporadic disease in clinical practice, with a rare incidence of human-to-human transmission[13,14]. The symptoms of psittacosis are nonspecific[15], but fever is usually the onset symptom[16], which can mimic COVID-19. In our study, four medical staff members who presented the onset symptom of fever were successively diagnosed with psittacosis by high-throughput genetic testing, indicating potential human-to-human transmission. All 4 confirmed patients with psittacosis were young (aged 26-48), which is consistent with a previous study[17]. However, COVID-19 has not shown an age preference[3].
The laboratory tests of patients with psittacosis also have clinically important differences regarding the WBC count and lymphocyte count compared with patients with COVID-19. Decreased WBC count and lymphocyte count are considered specific clinical presentations of COVID-19[18,19]. However, the two laboratory indices were both increased in all 6 patients. Moreover, the neutrophil count and platelet count were higher in patients with psittacosis than in patients with COVID-19 (P = 0.000, P = 0.035). The abovementioned differences may be attributed to the different reactions against viral and bacterial infections. Viral infection may generate a series of immune responses and cause changes in peripheral WBCs and immune cells, such as lymphocytes[19]. In contrast, bacterial infection usually causes an increased WBC count[20,21]. A higher level of CRP is more often seen in bacterial infections than in viral infections[22], which was also observed in our study (P = 0.035). Another interesting result is that calcium was lower in patients with COVID-19 than in those with psittacosis, which is supported by previous studies[23,24].
CT plays an important role in screening, diagnosing and evaluating the treatment response of COVID-19. It also has the advantage of differentiating COVID-19 pneumonia from other viral-infected pneumonias[25]. In the current study, several imaging features could differentiate COVID-19 pneumonia from psittacosis. Specifically, lesions in patients with psittacosis were more likely to be unilateral (P = 0.001), involve fewer lung lobes (P = 0.006) and present pleural effusions (P = 0.002). These aforementioned imaging features are uncommon in patients with COVID-19[6,26]. The follow-up CT changes of patients with psittacosis are also reported in the current study. Our results showed that the consolidations on CT images were absorbed after the treatment but with an increased involvement area, and GGOs were present in 3 patients. However, the follow-up CT imaging features are different in patients with COVID-19, which mostly present GGO lesions on the initial CT images and then change into consolidations on subsequent CT scans[27].
The clinical factors, laboratory tests and imaging features of patients who had not been diagnosed with psittacosis (patient 0) were similar to those of patients 1-4. Moreover, patient 0 had an exposure history to poultry. Therefore, there is reason to suspect that Patient 0 might be patient 0 in Cluster 1 and have transmitted the virus to patients 1-4. Other evidence of potential human-to-human transmission was obtained in Cluster 2. Patient0 developed fever first and transmitted the virus to his neighbors (Patients1 and Patients2 ). Of course, there is no robust evidence to directly support the view of human-to-human transmission. Further and deeper analyses should be performed.
The current study has several limitations. First, the included sample size was small, especially for patients with psittacosis. The statistical analyses between the two groups are only for reference. However, psittacosis is indeed a rarely diagnosed disease. Only 72 human cases were diagnosed and reported to the Centers for Disease Control and Prevention (CDC) in the United States during 2005-2012[28]. Clustering outbreaks of psittacosis are rare in clinical practice. Second, we only included two successive CT scans for patients with psittacosis. The CT changes over the entire course of treatment were not investigated.
Psittacosis has the potential for human-to-human transmission. Patients with psittacosis present increased WBC count and neutrophil count and have specific CT imaging findings, including unilateral distribution, less involvement of lung lobes and pleural effusions, which might help us to differentiate it from COVID-19 in clinical practice.
Psittacosis, a zoonotic infectious disease caused by the bacterium Chlamydia (C.) psittaci, is rarely diagnosed in clinical and can mimic the coronavirus disease 2019 (COVID-19). However, the differences in laboratory tests and imaging features between psittacosis and COVID-19 remain unknown.
We want to share the experiences of two clusters of cases with C. psittaci infection and hope the experience may contribute a little to fight the outbreak of COVID-19.
Here we report two clusters of cases with C. psittaci infection which mimicking COVID-19 with the aim to better understand the two diseases and then make an early diagnosis and treatment.
We reported a cluster of 4 cases (medical staffs) confirmed with psittacosis. The clinical characteristics, laboratory tests and CT imaging findings were comprehensively investigated and compared with patients confirmed as COVID-19.
The two diseases have different characteristics regarding lab tests and imaging features. In patients with COVID-19, the white blood cell count (WBC), neutrophil count and calcium were more likely to be decreased and have vascular enlargement. In patients with psittacosis. Lymphocyte count and platelet count were higher and lesions presented on CT images were more likely to be unilateral, involve fewer lung lobes and have pleural effusions.
Psittacosis has the potential ability of human-to-human transmission. Patients with psittacosis present increased WBC count, neutrophil count and have specify CT imaging findings, including unilateral distribution, less involvement lung lobes and pleural effusions, which might help us to differentiate it from COVID-19 in clinical practice.
Firstly, including more samples to further investigate the two diseases and support the conclusion. Secondly, including more kinds of pneumonia caused by other viruses to better diagnose the COVID-19.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lozada-Martinez I S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470-473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4848] [Cited by in F6Publishing: 4152] [Article Influence: 1038.0] [Reference Citation Analysis (1)] |
| 2. | World Health Organization website. WHO Coronavirus (COVID-19) Dashboard. [cited 15 July 2021]. Available from: https://covid19.who.int/. [Cited in This Article: ] |
| 3. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19202] [Cited by in F6Publishing: 17996] [Article Influence: 4499.0] [Reference Citation Analysis (5)] |
| 4. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6231] [Cited by in F6Publishing: 6354] [Article Influence: 1588.5] [Reference Citation Analysis (0)] |
| 5. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32663] [Cited by in F6Publishing: 28482] [Article Influence: 7120.5] [Reference Citation Analysis (3)] |
| 6. | Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol. 2020;214:1072-1077. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 665] [Cited by in F6Publishing: 681] [Article Influence: 170.3] [Reference Citation Analysis (0)] |
| 7. | West A. A Brief Review of Chlamydophila psittaci in Birds and Humans. J Exot Pet Med. 2011;1:18-20. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Hogerwerf L, DE Gier B, Baan B, VAN DER Hoek W. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: a systematic review and meta-analysis. Epidemiol Infect. 2017;145:3096-3105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 113] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 9. | Rybarczyk J, Versteele C, Lernout T, Vanrompay D. Human psittacosis: a review with emphasis on surveillance in Belgium. Acta Clin Belg. 2020;75:42-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Zhao W, Zhong Z, Xie X, Yu Q, Liu J. CT Scans of Patients with 2019 Novel Coronavirus (COVID-19) Pneumonia. Theranostics. 2020;10:4606-4613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 11. | Wang H, Zhang Y, Huang B, Deng W, Quan Y, Wang W, Xu W, Zhao Y, Li N, Zhang J, Liang H, Bao L, Xu Y, Ding L, Zhou W, Gao H, Liu J, Niu P, Zhao L, Zhen W, Fu H, Yu S, Zhang Z, Xu G, Li C, Lou Z, Xu M, Qin C, Wu G, Gao GF, Tan W, Yang X. Development of an Inactivated Vaccine Candidate, BBIBP-CorV, with Potent Protection against SARS-CoV-2. Cell. 2020;182:713-721.e9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 461] [Cited by in F6Publishing: 520] [Article Influence: 130.0] [Reference Citation Analysis (0)] |
| 12. | Gao Q, Bao L, Mao H, Wang L, Xu K, Yang M, Li Y, Zhu L, Wang N, Lv Z, Gao H, Ge X, Kan B, Hu Y, Liu J, Cai F, Jiang D, Yin Y, Qin C, Li J, Gong X, Lou X, Shi W, Wu D, Zhang H, Deng W, Lu J, Li C, Wang X, Yin W, Zhang Y. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369:77-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1106] [Cited by in F6Publishing: 972] [Article Influence: 243.0] [Reference Citation Analysis (0)] |
| 13. | Wallensten A, Fredlund H, Runehagen A. Multiple human-to-human transmission from a severe case of psittacosis, Sweden, January-February 2013. Euro Surveill. 2014;19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Ito I, Ishida T, Mishima M, Osawa M, Arita M, Hashimoto T, Kishimoto T. Familial cases of psittacosis: possible person-to-person transmission. Intern Med. 2002;41:580-583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Balsamo G, Maxted AM, Midla JW, Murphy JM, Wohrle R, Edling TM, Fish PH, Flammer K, Hyde D, Kutty PK, Kobayashi M, Helm B, Oiulfstad B, Ritchie BW, Stobierski MG, Ehnert K, Tully TN Jr. Compendium of Measures to Control Chlamydia psittaci Infection Among Humans (Psittacosis) and Pet Birds (Avian Chlamydiosis), 2017. J Avian Med Surg. 2017;31:262-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 16. | Knittler MR, Sachse K. Chlamydia psittaci: update on an underestimated zoonotic agent. Pathog Dis. 2015;73:1-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 17. | Shaw KA, Szablewski CM, Kellner S, Kornegay L, Bair P, Brennan S, Kunkes A, Davis M, McGovern OL, Winchell J, Kobayashi M, Burton N, de Perio MA, Gabel J, Drenzek C, Murphy J, Holsinger C, Forlano L. Psittacosis Outbreak among Workers at Chicken Slaughter Plants, Virginia and Georgia, USA, 2018. Emerg Infect Dis. 2019;25:2143-2145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 18. | COMMISSION. Diagnosis and treatment of pneumonitis caused by new coronavirus (trial version 7). Beijing: China National Health Commission, 2020. [cited 12 June 2020]. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. [Cited in This Article: ] |
| 19. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13871] [Cited by in F6Publishing: 12369] [Article Influence: 3092.3] [Reference Citation Analysis (1)] |
| 20. | Bhuiyan MU, Blyth CC, West R, Lang J, Rahman T, Granland C, de Gier C, Borland ML, Thornton RB, Kirkham LS, Martin A, Richmond PC, Smith DW, Jaffe A, Snelling TL. Combination of clinical symptoms and blood biomarkers can improve discrimination between bacterial or viral community-acquired pneumonia in children. BMC Pulm Med. 2019;19:71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Karakonstantis S, Kalemaki D. Correspondence to "Role of neutrophil to lymphocyte and monocyte to lymphocyte ratios in the diagnosis of bacterial infection in patients with fever". Infection. 2018;46:139-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 22. | Don M, Valent F, Korppi M, Canciani M. Differentiation of bacterial and viral community-acquired pneumonia in children. Pediatr Int. 2009;51:91-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 231] [Cited by in F6Publishing: 239] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 23. | Lippi G, South AM, Henry BM. Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19). Ann Clin Biochem. 2020;57:262-265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 185] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 24. | Cappellini F, Brivio R, Casati M, Cavallero A, Contro E, Brambilla P. Low levels of total and ionized calcium in blood of COVID-19 patients. Clin Chem Lab Med. 2020;58:e171-e173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 25. | Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie FF, Li S, Healey T, Atalay MK, Liao WH. Performance of Radiologists in Differentiating COVID-19 from Non-COVID-19 Viral Pneumonia at Chest CT. Radiology. 2020;296:E46-E54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 726] [Cited by in F6Publishing: 695] [Article Influence: 173.8] [Reference Citation Analysis (0)] |
| 26. | Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, Ling Y, Jiang Y, Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020;295:210-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 839] [Cited by in F6Publishing: 761] [Article Influence: 190.3] [Reference Citation Analysis (0)] |
| 27. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1617] [Cited by in F6Publishing: 1665] [Article Influence: 416.3] [Reference Citation Analysis (0)] |
| 28. | Adams DA, Jajosky RA, Ajani U, Kriseman J, Sharp P, Onwen DH, Schley AW, Anderson WJ, Grigoryan A, Aranas AE, Wodajo MS, Abellera JP; Centers for Disease Control and Prevention (CDC). Summary of notifiable diseases--United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;61:1-121. [PubMed] [Cited in This Article: ] |