Abstract
Background:
Pregnancy and childbirth do not increase the risk of COVID-19 infection, but the clinical complications and worsening are more severe than in non-pregnant women.Objectives:
The aim of this study was to determine the clinical epidemiology of mothers with COVID-19 hospitalized in Ardabil province.Methods:
In this cross-sectional descriptive study, the medical records of 20193 women of childbearing age from March 2020 to August 20 were reviewed. Gestational age, cause of hospitalization, the trend of disease and pregnancy, and possible and non-obstetric complications were evaluated. Data were analyzed by using statistical tests in SPSS version 21.Results:
In this study, 9942 childbirths were performed, of which 5965 cesarean sections, 3977 normal deliveries, 6990 preterm deliveries, and 72 women had stillbirths. Also, 73 (0.73%) pregnant women had early symptoms of COVID-19. The highest age range was 25 - 30 years, mostly in the first pregnancy (41.9%) and the third trimester of pregnancy (61.6%) and with symptoms of persistent dry cough, shortness of breath, fever, muscle pain, chills, decreased arterial oxygen saturation and they were dizzy. Among all infected mothers, 20.5% had a preterm delivery, and 8.2% had a stillbirth. 0.36% of mothers with symptoms and 0.46% of mothers were PCR positiveConclusions:
Pregnant women do not show clinical periods, and the result is comparable to non-pregnant women of childbearing age when infected with SARS-CoV-2. 0.3% of pregnant mothers were infected, which is not a high rate. Complications of pregnancy, such as preterm delivery and IUFD, are more common in involved pregnant women.Keywords
1. Background
The SARS-CoV-2 virus has been detected in Wuhan, China, since December 2019 and has caused widespread pandemics. The virus causes widespread involvement in the body and causes respiratory failure and various renal and systemic complications (1). It continues to cause thousands of deaths worldwide (2). Pregnancy and childbirth do not generally increase the risk of COVID-19 infection, but the clinical course appears to be worse than in non-pregnant women of the same sex and age, and clinical deterioration may be rapid (3). The symptoms of the disease in pregnant women are similar to those of non-pregnant women (with a lower incidence) (4). However, more than 90% of infected people recover without giving birth. Symptoms include cough, headache, muscle aches, fever, sore throat, shortness of breath, loss of taste or smell, nausea or vomiting, fatigue, diarrhea, and rhinorrhea (5, 6). Laboratory findings include lymphopenia, leukocytosis, elevated procalcitonin levels, abnormal liver tests, and thrombocytopenia. Chest radiographs may be normal early in the disease or mild. Laboratory findings in a systematic review of pregnant and recently pregnant women with suspected or confirmed COVID-19, including lymphopenia (35%), leukocytosis (27%), elevated procalcitonin levels (21%), abnormal liver function tests (11%), thrombocytopenia (8%). Laboratory and imaging findings are similar to those of non-pregnant women (6, 7).
The US National Institutes of Health classifies the severity of the disease in non-pregnant people as follows: A symptomatic infection: Positive test for SARS-CoV-2; but a symptomatic, mild illness: Any signs and symptoms (such as fever, cough, sore throat, lethargy, headache, muscle aches) without shortness of breath or abnormal chest imaging; moderate disease: Evidence of inferior respiratory disease in clinical evaluation or imaging and oxygen saturation less than or equal to 94% in room air; severe illness: Tachypnea, a respiratory rate greater than 30 breaths per minute, hypoxia (less than 94% oxygen saturation in room air), the ratio of relative arterial pressure of oxygen to tail oxygen fraction (PaO2 / FiO2) < 300 or more than 50% of lung involvement in imaging; critical disease: Respiratory failure, septic shock, or dysfunction of several organs (6).
Pregnant women have a special immunological adaptation essential for preserving fetal semi-allograft tissue. This transiently suppressed immune system is modulated by suppressing T cell activity, and therefore, pregnant women are prone to viral and bacterial infections. Physiological changes in their respiratory and circulatory systems may worsen clinical outcomes when infected with the virus during pregnancy. These changes not only cause obstetric complications in them but may also be caused developmental damage to the fetus (8).
Important questions arise because of the prevalence of COVID-19: Are the symptoms of pneumonia different in pregnant women than in non-pregnant women? What is the probability of maternal and infant mortality? (9) What is the probability of maternal and infant mortality? Does it cause complications of pregnancy or premature birth? How much COVID-19 is transmitted to the baby? (10).
Considering the importance of maternal and child health, according to the World Health Organization, countries should have programs to deal with infectious and non-infectious diseases in order to improve the health of mothers and children. In the current pandemic, extensive studies have been performed on pregnant women with COVID-19 to study risk factors, clinical signs, the severity of symptoms, hospitalization, and treatment.
2. Methods
The present descriptive cross-sectional study was performed on all mothers with clinical symptoms of COVID 19 admitted to hospitals in Ardabil state from 2020/03/02 to 2020/08/10, and the data collection tool included a checklist. The type of sampling was simple. The total number of pregnant mothers referred in 2019 was 73, and the number of mothers hospitalized with COVID-19. Data collection tools included a questionnaire containing research variables completed for each patient. This information included the mother’s calendar age, gestational age, place of residence, type of hospitalization in the general or intensive care unit, laboratory abnormalities, PCR test results, and CT scan results if recorded, and pregnancy results and obstetric complications, including abortion, intrauterine death, stillbirth, preterm delivery, normal term delivery or cesarean section were also recorded. In patients admitted to the intensive care unit, hospitalization results, the need for mechanical ventilation, recovery, or death were recorded and followed up. The extracted statistics and information were analyzed with the concurrent statistics of non-corona pregnant women. The data was analyzed using statistical tests with SPSS23 software.
3. Results
In the present study (144 days), 20193 pregnant mothers have been referred to the medical centers of the province. Termination of pregnancy was according to Table 1. Of these pregnant women, 73 were hospitalized with early signs of corona heart disease. The highest age group was 25 - 30 years, and most were 61.6% in the third trimester of pregnancy. Forty-one point nine percent of pregnant mothers had their first pregnancy, 32.4% their second pregnancy, 9.5% their third pregnancy, 13.5% their fourth pregnancy, and the rest had their fifth and sixth pregnancies. Clinical signs include dry cough at 51.4%, shortness of breath at 40.5%, fever at 29.7%, muscle pain at 6.8%, chill at 5.4%, decreased arterial oxygen saturation at 5.4%, dizziness at 2.7%, tachypnea at 41.1%, sore throat was 1.4%, and 10.8% were asymptomatic (Tables 1 and 2).
Specifications Under Review for Mothers with Corona
| Title and Case Study | No. (%) |
|---|---|
| Total condition of pregnant mothers | |
| Total termination of pregnancy | 9942 (49.2) |
| Cesarean section | 5965 (59.9) |
| Normal vaginal delivery | 3977 (40) |
| Preterm labor | 699 (7) |
| Stillbirth | 72 (0.7) |
| Status of pregnant mothers | |
| Cesarean section | 26 (35.7) |
| Normal vaginal delivery | 21 (28.8) |
| preterm labor | 15 (20.6) |
| Stillbirth | 6 (8.2) |
| Abortion | 5 (6.8) |
| Gestational age | |
| The first trimester of pregnancy | 5 (6.8) |
| The second trimester of pregnancy | 23 (31.5) |
| The third trimester of pregnancy | 45 (31.6) |
| Clinical symptoms | |
| No symptoms | 8 (10.8) |
| Fever | 22 (29.7) |
| currency | 4 (5.4) |
| Cough | 38 (51.4) |
| Shortness of breath | 30 (40.5) |
| Vertigo | 2 (2.7) |
| Decreased arterial oxygen saturation | 4 (5.4) |
| tachypnea | 1 (1.4) |
| Muscular pain | 5 (6.8) |
| Sore throat | 1 (1.4) |
| Admission to the ICU | |
| Intubation (mechanical ventilation) | 4 (33) |
| Successful weaning and extubation | 8 (67) |
Age Range of Pregnant Women Hospitalized with COVID-19
| Age Range | |||||
|---|---|---|---|---|---|
| 15 - 20 | 20 - 25 | 25 - 30 | 30 - 35 | > 35 | |
| % | 6.8 | 15.1 | 39.7 | 17.8 | 20.5 |
For mothers with COVID, 29 (29.2%) cases were terminated by cesarean section, and 21 (28.4%) cases were terminated by natural childbirth. Twenty cases were pregnant at the end of the study period, and 2 (2.7%) abortions and 2 (2.7%) abortions were reported. 20.5% had preterm delivery and 8.2% stillbirth (Table 1). Twelve cases were admitted to the intensive care unit, all of whom were discharged in good general condition (Table 1).
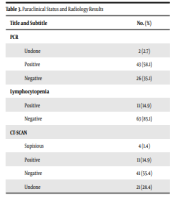
In the CRP test performed by 57 mothers (78.1%), the answer was negative, 8 cases (11%) positive, 4 (5.5%) 2 positive, and 4 (5.5%) 3 positive. CT-scan was not performed in 21 patients and 41 (55.4%) patients; the CT-scan result was normal in 11 (1.4%) cases of coronary heart disease symptoms and 4 (1.4%) cases of fishy reported. In the lymphopenia test, 63 (85.1%) reported a negative result, and 11 (14.9%) reported a positive result. In the PCR test, 26 (1.1%) cases were negative, and 43 (58.1%) cases were positive (Table 3).
Paraclinical Status and Radiology Results
| Title and Subtitle | No. (%) |
|---|---|
| PCR | |
| Undone | 2 (2.7) |
| Positive | 43 (58.1) |
| Negative | 26 (35.1) |
| Lymphocytopenia | |
| Positive | 11 (14.9) |
| Negative | 63 (85.1) |
| CT-SCAN | |
| Supisious | 4 (1.4) |
| Positive | 11 (14.9) |
| Negative | 41 (55.4) |
| Undone | 21 (28.4) |
The percentage of mothers admitted with COVID-19 mark compared to all mothers was 0.36%. The percentage of PCR-positive mothers (hospitalized and outpatient) was 0.46%, and the total number of pregnant mothers was 0.22%. The comparison of the results of the type of delivery and obstetric complications of hospitalized mothers of COVID-19 with others is summarized in Table 4.
Maternal Outcome of Corona and Non-corona
| Pregnancy Outcome | Total | Percent | Number of Cases COVID-19 | Percentage of Cases with COVID |
|---|---|---|---|---|
| Cesarean section | 5965 | 60 | 26 | 0.4 |
| Normal vaginal delivery | 3977 | 40 | 21 | 0.52 |
| Total delivery | 9942 | 100 | 47 | 0.47 |
| Abortion | 1954 | 10.6 | 5 | 0.47 |
| Stillbirth | 72 | 0.72 | 6 | 8.3 |
| Preterm labor | 699 | 7 | 15 | 2.1 |
4. Discussion
The COVID-19 pandemic has been a major global challenge since December 2019 and has challenged all health systems in the country. The forefront of controlling this disease, like many infectious diseases is prevention, and health systems play a key role in informing about ways to prevent infection. Therapeutic systems have prioritized the diagnosis and treatment of COVID-19 for the past 8 months. Pregnant mothers are among the most at-risk groups in the health care system, and improving their health is one of the health indicators of the Ministry of Health and the World Health Organization. In the current acute situation, pregnant mothers, like other sections of society, are at risk of coronary heart disease; on the other hand, COVID’s disease can affect the health of the mother and fetus and lead to maternal and obstetric complications such as abortion, stillbirth, preterm delivery, etc. On the other hand, infection with this virus, like other dangerous viruses, may lead to fetal complications such as various anomalies. Because it does not take long to recognize and define the disease, healthcare systems need to share their information about the results of pregnant mothers with the virus to better identify the behavior in pregnant women. Although the disease is often mild, it is a severe disease in the high-risk population and, in many cases, leads to death. The consequences of pregnancy remain largely unknown (11). Qiancheng et al.’s study did not show a relationship between pregnancy and disease severity and length of hospital stay (8). There was also no evidence of vertical transmission late in pregnancy, including vaginal delivery (8), which is consistent with the results of the present study. Ellington et al. reported that pregnant women were more likely to be hospitalized than non-pregnant women and were at greater risk for intensive care unit (ICU) admission and mechanical ventilation, but their mortality was similar (12) and contradicted the results of the present study. In the present study, the average age of the affected mothers was 25 - 30 years, most of whom were in the third trimester of pregnancy. In Zaigham and Andersson’s study, the average age of the mother was 29 to 32 years, and women were mostly in the third trimester of pregnancy and comorbidities including preeclampsia, gestational diabetes, hypothyroidism, placenta previa, previous uterine surgeries, etc., were reported (13). There is no information on the association between gynecological diseases, such as preeclampsia, gestational diabetes, and COVID-19. Since epidemics cause anxiety and stress, pregnant women can experience side effects such as preeclampsia, depression, preterm labor, increased nausea, and vomiting (14). In the studied pregnant women, there were some concomitant diseases or complications of pregnancy, such as preeclampsia, the onset of labor pains, preterm labor, embolism, seizures, bleeding, fetal motility, gestational diabetes, etc., which were approximately consistent with the results of Zaigham and Andersson’s and Ellington et al.’s research (12, 13).
In the present study, the most common symptoms of COVID-19 disease were fever at 29.7%, shivering at 5.4%, cough at 51.4%, and shortness of breath at 40.5% (13). In Marim et al.’s study, the most common symptoms in pregnant patients were fever and cough, chest pain, fatigue, shortness of breath, sore throat, diarrhea, and headache (14). In the weekly report of June 16, 2020, Ellington et al. reported on the characteristics of COVID-19 disease in pregnant and non-pregnant women with symptomatic symptoms similar to cough (> 50%) and shortness of breath (30%) (12). According to the findings of this study, the percentage of pregnant women admitted with the clinical symptom of COVID-19 relative to the total number of pregnant mothers was 0.3% which is not a high number compared to the total. In Wuhan, China, pregnant women accounted for 0.24%. In the United States, (2%) of patients were pregnant, and 4 were admitted to the ICU (14). According to the Ellington et al.’s study, approximately one-third (31.5%) of pregnant women were hospitalized (compared with 5.8% of non-pregnant women) (12).
The laboratory findings of pregnant women are very similar to those of other patients. The most common laboratory finding is lymphocytopenia. An increase in CRP and ESR was also seen. This study observed lymphocytopenia and positive PCR in 14.9% and 58.1% of hospitalized mothers. In the study by Zaigham and Andersson, 59% lymphocytopenia and CRP 70% increase was observed (13). Chest radiographs are usually normal. Contrast-free CT scan (due to low risk to the fetus) should be performed to confirm the diagnosis in suspected cases. Findings found on lung CT scans are significantly more pronounced in pregnant women than in non-pregnant adults (14). In the present study, the percentage of CT scan symptoms in hospitalized pregnant women was 16.6%.
In some studies, premature rupture of membranes, preterm delivery, and blood clotting with liver dysfunction and maternal death have been reported in pregnant women. In the present study, in mothers with COVID-19, the indicators of termination of pregnancy changed, the rate of normal delivery and preterm delivery increased, and the rate of cesarean section and abortion did not change much. In Della Gatta et al. systematic review, 39% of preterm deliveries (> 37 weeks) and 96% of cesarean sections were reported (15). In a study in the United Kingdom, Khalil et al. obtained similar results to a study of the prevalence of stillbirth and preterm labor during a pandemic (16). The researchers reported high rates of preterm delivery and cesarean section in women with the severe acute respiratory syndrome but did not find enough evidence for stillbirth (16). There is no evidence that the delivery method is superior to COVID-19 in terms of risks associated with another unless the pregnant woman’s clinical severity and respiratory status require immediate intervention; in the present study, 28.8% of natural deliveries and 35.6% of cesarean deliveries were performed. 20.5% gave birth prematurely, and 6.8% resulted in an abortion. Pregnant women with COVID-19 have a higher prevalence of preterm delivery, low birth weight, cesarean delivery, and NICU hospitalization than the general population, consistent with Phowsa and Khaliq’s study in South Africa (17). In Mullins et al.’s study, preterm delivery affected 47% of women admitted for COVID-19 (18). Marim et al. reported severe maternal morbidity and mortality due to COVID-19 and recommended careful monitoring of pregnancy and measures to prevent neonatal infection (14). There are few reports of the virus in the amniotic fluid, cord blood, breast milk, and throat swabs in infants of infected mothers, but the possibility of vertical transmission of the virus to the fetus has not been ruled out (14). Vertical transmission of infection from mother to fetus can occur around childbirth in the third trimester, but it is not common (19). Pregnant women do not show clinical periods, and the result is comparable to non-pregnant women of childbearing age when infected with SARS-CoV-2. Zero point three percent of pregnant mothers were infected, which is not a high rate. Complications of pregnancy, such as preterm delivery and IUFD, are more common in involved pregnant women.
References
-
1.
Haghbin M, Abbasi A, Rafei E, Kheradmand A, Javdani F, Hatami N, et al. [Anxiety caused by new coronavirus (Covid-19) in breast cancer patients during the coronavirus pandemic]. Iran J Obstet Gynecol Infertil. 2020;23(8):8-17. Persian.
-
2.
Keyvanlo Z, Mahdavifar N, Shahrabadi R, Mehri A, Joveini H, Hashemian M. [Level of knowledge, attitude, and practice of women in Sabzevar concerning home quarantine for prevention of the new coronavirus disease]. Iran J Obstet Gynecol Infertil. 2020;23(8):49-57. Persian.
-
3.
Moaya M, Shahali S, Farhoudi B. [Maternal and neonatal outcomes of pregnant women with COVID-19 in Amir-al-momenin hospital during March to May 2020]. Iran J Obstet Gynecol Infertil. 2021;23(9):35-42. Persian.
-
4.
Fayazi M, Rahmani R, Rahmani Bilandi R. [Clinical manifestations, maternal, fetal and neonatal outcomes in pregnant women with COVID-19: A systematic review]. Iran J Obstet Gynecol Infertil. 2021;24:108-19. Persian.
-
5.
Eshraghi N, Kashanian M, Eshraghi N, Sarchami N, Nafisi N. [A pregnant woman with uncommon symptoms and complications of covid19: Case report]. Iran J Obstet Gynecol Infertil. 2021;23(11):106-11. Persian.
-
6.
Berghella V, Hughes B. Coronavirus disease 2019 (COVID-19). Pregnancy issues. 2020:1-18.
-
7.
Alavian F, Alavian K. [Pregnancy and COVID-19: Physiology, some Challenges, and Solutions]. Iran J Obstet Gynecol Infertil. 2021;24(1):99-111. Persian.
-
8.
Qiancheng X, Jian S, Lingling P, Lei H, Xiaogan J, Weihua L, et al. Coronavirus disease 2019 in pregnancy. Int J Infect Dis. 2020;95:376-83. [PubMed ID: 32353549]. [PubMed Central ID: PMC7185021]. https://doi.org/10.1016/j.ijid.2020.04.065.
-
9.
Panahi L, Amiri M, Pouy S. Risks of Novel Coronavirus Disease (COVID-19) in Pregnancy; a Narrative Review. Arch Acad Emerg Med. 2020;8(1). e34. [PubMed ID: 32232217]. [PubMed Central ID: PMC7092922].
-
10.
Yousefian M, Farzipour S, Noroozi V, Salmanfar T. AComparative Study of Ketofol and Thiopental Sodium in Patients undergoing Dilation and Curettage by General Anesthesia. Rev Latinoam de Hipertens. 2018;13(6):515-9.
-
11.
Dotters-Katz SK, Hughes BL. Considerations for Obstetric Care during the COVID-19 Pandemic. Am J Perinatol. 2020;37(8):773-9. [PubMed ID: 32303077]. [PubMed Central ID: PMC7356077]. https://doi.org/10.1055/s-0040-1710051.
-
12.
Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, et al. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769-75. [PubMed ID: 32584795]. [PubMed Central ID: PMC7316319]. https://doi.org/10.15585/mmwr.mm6925a1.
-
13.
Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020;99(7):823-9. [PubMed ID: 32259279]. [PubMed Central ID: PMC7262097]. https://doi.org/10.1111/aogs.13867.
-
14.
Marim F, Karadogan D, Eyuboglu TS, Emiralioglu N, Gurkan CG, Toreyin ZN, et al. Lessons Learned so Far from the Pandemic: A Review on Pregnants and Neonates with COVID-19. Eurasian J Med. 2020;52(2):202-10. [PubMed ID: 32612432]. [PubMed Central ID: PMC7311134]. https://doi.org/10.5152/eurasianjmed.2020.20118.
-
15.
Della Gatta AN, Rizzo R, Pilu G, Simonazzi G. Coronavirus disease 2019 during pregnancy: A systematic review of reported cases. Am J Obstet Gynecol. 2020;223(1):36-41. [PubMed ID: 32311350]. [PubMed Central ID: PMC7165087]. https://doi.org/10.1016/j.ajog.2020.04.013.
-
16.
Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O'Brien P, Magee L. Change in the Incidence of Stillbirth and Preterm Delivery During the COVID-19 Pandemic. JAMA. 2020;324(7):705-6. [PubMed ID: 32648892]. [PubMed Central ID: PMC7435343]. https://doi.org/10.1001/jama.2020.12746.
-
17.
Phoswa WN, Khaliq OP. Is pregnancy a risk factor of COVID-19? Eur J Obstet Gynecol Reprod Biol. 2020;252:605-9. [PubMed ID: 32620513]. [PubMed Central ID: PMC7320674]. https://doi.org/10.1016/j.ejogrb.2020.06.058.
-
18.
Mullins E, Evans D, Viner RM, O'Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586-92. [PubMed ID: 32180292]. https://doi.org/10.1002/uog.22014.
-
19.
Ranjbar F, Gharacheh M. “Letter to Editor” Should women postpone childbearing during the COVID-19 pandemic? Iran J Nurs. 2020;33(123):1-5. https://doi.org/10.29252/ijn.33.123.1.