- Department of Anesthesiology, University of Chicago at Illinois, Advocate Illinois Masonic Medical Center, Chicago, Illinois, United States.
DOI:10.25259/SNI_801_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ramsis Ghaly, Zinaida Perciuleac, Ana Pleasca, Iulia Pirvulescu, Kenneth D. Candido, Nebojsa Nick Knezevic. Innovative overhead transparent plastic barrier with powered suction technique intended to limit coronavirus disease 2019 aerosols spread during fiber-optic intubation and throughout the surgery. 29-Dec-2020;11:473
How to cite this URL: Ramsis Ghaly, Zinaida Perciuleac, Ana Pleasca, Iulia Pirvulescu, Kenneth D. Candido, Nebojsa Nick Knezevic. Innovative overhead transparent plastic barrier with powered suction technique intended to limit coronavirus disease 2019 aerosols spread during fiber-optic intubation and throughout the surgery. 29-Dec-2020;11:473. Available from: https://surgicalneurologyint.com/surgicalint-articles/10495/
Abstract
Background: In the context of the current coronavirus pandemic, we propose an inexpensive, innovative overhead transparent plastic barrier with powered suction (OTPBPS) technique using materials that are ubiquitous in the hospital, easy to set up in minutes and well tolerated by the patients. As presented in this case report, it is an effective method to reduce viral spread from patients with positive or suspected yet unconfirmed coronavirus disease 2019 status.
Case Description: A 49-year-old male was admitted to the hospital with a diagnosis of cervical stenosis and a C6-C7 disc herniation with spinal cord compression. The OTPBPS technique was set up to create a negative pressure environment around the patient’s head, using a Mayo stand, a transparent plastic bag, and powered wall canister suction. The neurosurgeon successfully performed an anterior cervical discectomy and instrumented fusion under OTPBPS. The patient was satisfied with the intubation and anesthetic management and reported excellent feedback.
Conclusion: The OTPBPS technique helps control the spread of an aerosolized viral load from the patient’s mouth or airway during awake fiber-optic intubation. This technique will help anesthesiologists and other front-line health-care providers manage copious endotracheal secretions and droplet particles, which have an immense infectious potential.
Keywords: Awake fiber-optic intubation, Coronavirus disease 2019, Plastic barrier, Severe acute respiratory syndrome coronavirus 2, Virus spread
INTRODUCTION
In December 2019, the coronavirus disease 2019 (COVID-19), a respiratory infection that spreads through aerosolized particles containing the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in Wuhan, Hubei Province, China.[
Airway management of patients with COVID-19 poses significant risks to health-care providers because of the aerosolizing nature of airway interventions, including facemask, supraglottic airway ventilation, intubation, extubation, and cardiopulmonary resuscitation. These activities require increased precautions and containment of viral respiratory particles. It has been demonstrated that a containment system can limit the spray of a significant portion of respiratory particles during a simulated cough or extubation.[
We propose an inexpensive, innovative overhead transparent plastic barrier with powered suction (OTPBPS) technique made from materials that are ubiquitous in the hospital, quick, and easy to set up, which are well tolerated by the patients. The current case report shows that it is an effective method to protect health-care providers from potential viral spread by patients with positive or unconfirmed COVID-19 status.
CASE DESCRIPTION
A 49-year-old male was admitted to the hospital with diagnosis of cervical stenosis, a C6-C7 intervertebral disc herniation with spinal cord compression and pending COVID-19 test results. The patient arrived in the operating room wearing a protective facemask. Standard American Society of Anesthesiologists monitors were applied. The OTPBPS technique was set up as described below, in preparation for awake fiber-optic intubation.
The OTPBPS technique
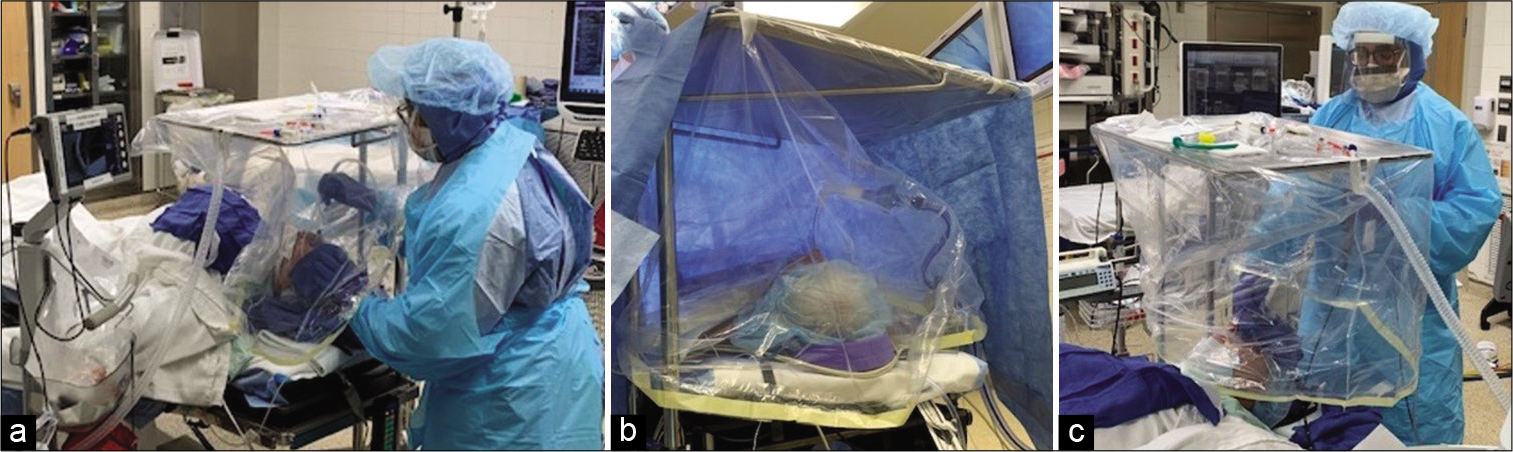
The simulation technique was first carried out in volunteers and revealed no issues with oxygen saturation, while breathing was deemed “excellent” and without claustrophobia.
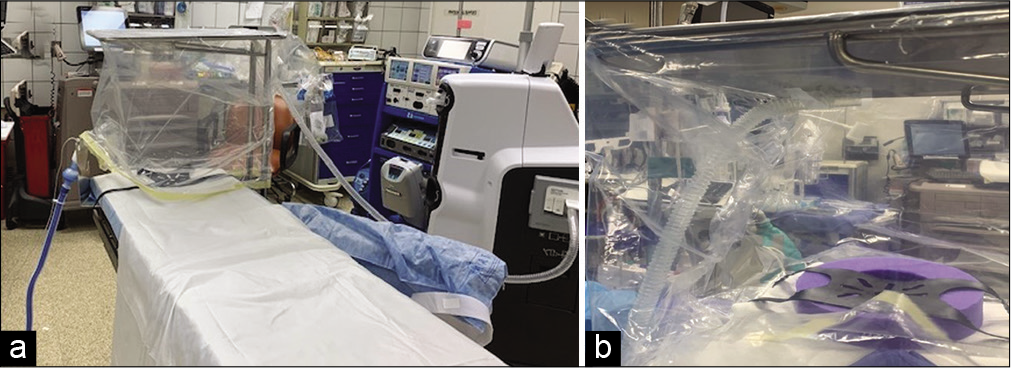
It is recommended to use a large clear transparent plastic bag, Mayo stand, and large powered suction, covering the head of the bed space [
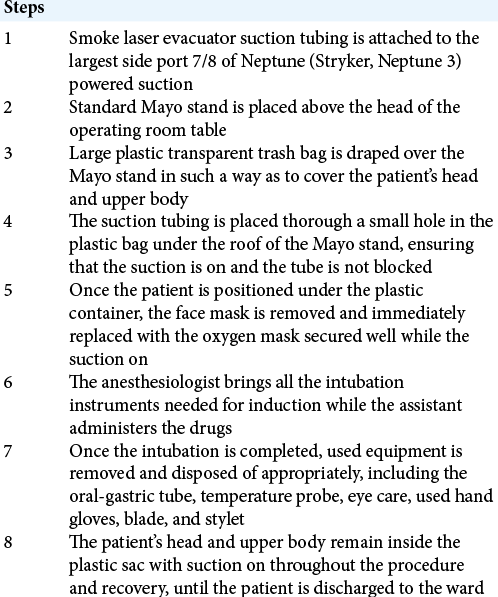
A step by step of the OTPBPS technique procedure is provided in [
Surgical outcome
Awake fiber-optic nasal intubation was carried out as per standard protocol, using a C-MAC fiber-optic scope (Karl Starz, C-MAC) and 7.5 mm endotracheal Rae nasal tube. The patient was satisfied with the intubation and anesthetic management, had no recall after the anesthetic local topicalization, and reported excellent overall clinical feedback. The neurosurgeon successfully performed an anterior cervical discectomy and instrumented fusion. The patient tolerated the procedure well and was kept intubated in the surgical intensive care unit (ICU) overnight to reduce airway swelling. The surgical and nursing staff felt confident that the OTPBPS technique provided protection against respiratory aerosols.
Use in other procedures
Modified partial plastic draping, restricted to the area of the patient’s mouth and nose can be used for head, neck, chest, and cardiac surgeries. The OTPBPS technique was used in other surgical procedures and is currently a standard practice in our institution for COVID-positive or high-risk patients for the coronavirus infection, during general anesthesia, conscious sedation and cases performed under regional anesthetic blockade.
DISCUSSION
Aerosol transmission
The SARS-CoV-2 virus is spread through inoculation of mucous membranes by droplets and aerosols containing the virus, as well as by contact with droplet-contaminated fomites. Fomites can act as live-virus reservoirs for hours to days. Studies on the dispersion of respiratory particles from a cough showed that they could extend more than 2 m from the subject. Within a closed room environment, such as an operating room, air currents generated by the breathing of the occupants disperse the cough particles so that anyone in the room would be exposed to the particles within minutes.[
Risk to health-care providers
As of December 7, 2020, there are over 14.6 million confirmed COVID-19 cases in the US.[
Due to the virus’s spread through aerosol droplets, health-care providers are exposed to increased risk of infection during aerosol-generating procedures such as endotracheal intubation and extubation. Although effective, conventional personal protective equipment provides only a static physical barrier between the health care worker and the infectious patient. Creating an additional barrier in preventing the spread of aerosolized particles may present a superior option for health-care providers’ safety.
Minimizing the spread of infectious particles
The OTPBPS technique is well tolerated for general anesthesia, conscious sedation, and awake fiber-optic intubation, throughout the surgery as well as in the early recovery phase. It can be adjusted to accommodate other operation room equipment with no interference such as that imposed by use of a C-arm or robotic arms.
Once the patient enters the operating room, his head and upper body are covered as seen in the picture [
There have been several published articles describing different methods of protection while intubating patients, but not all of them have proven to be functional, should complications develop, and the intubation cannot be accomplished.[
Limitations
Despite the benefits that the OTPBPS technique provides health care workers, it may hinder their access to a patient’s head and upper chest, which could particularly be an issue in a real emergency. In addition, although the vacuum reduces the viral particles, it does not guarantee full immunity to the health-care personnel. All measures need to be taken to prevent trapping of the virus in the plastic drape, which could happen if the suction is not sufficiently powerful. The plastic drape should not be reused. The OTPBPS technique may also be uncomfortable for claustrophobic patients if they cannot tolerate it despite adequate preoperative preparation and sedation.
We recommend continued adherence to restricted PPE, limiting the number of people entering the plastic draping space, and limiting the time of proximity to the patient. Furthermore, it remains important to maintain a six-foot physical distance (when possible). Finally, when ready to remove the draping, care must be taken to avoid potential contamination of other sites.
CONCLUSION
In light of the current pandemic, the OTPBPS technique is used to limit viral spread from the patient’s airway during surgical procedures. It is inexpensive, convenient, and does not necessitate any additional training or skills. This technique helps health-care providers in the front lines of treating the pandemic manage highly infectious endotracheal secretions. The OTPBPS technique can be used in high-risk patients, positive or unknown status for COVID-19, throughout the hospital: not only in the operating room but also in the postanesthesia care unit, ICU, emergency department, and cardiac catheterization lab. The rising death toll from COVID-19 among health-care providers globally necessitates a change of standards of care. The OTPBPS is one such change and utilizes standard equipment readily found in most operating rooms in the country.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. . Available from: https://www.covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days [Last accessed on 2020 Dec 07].
2. . Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Last accessed on 2020 Dec 07].
3. Brown S, Patrao F, Verma S, Lean A, Flack S, Polaner D. Barrier system for airway management of COVID-19 patients. Anesth Analg. 2020. 131: e34-5
4. Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020. 382: 1957-8
5. . Characteristics of health care personnel with COVID-19-United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020. 69: 477-81
6. Klompas M, Morris CA, Sinclair J, Pearson M, Shenoy ES. Universal masking in hospitals in the COVID-19 era. N Engl J Med. 2020. 382: e63
7. Laosuwan P, Earsakul A, Pannangpetch P, Sereeyotin J. Acrylic box versus plastic sheet covering on droplet dispersal during extubation in COVID-19 patients. Anesth Analg. 2020. 131: e106-8
8. Lazzerini M, Putoto G. COVID-19 in Italy: Momentous decisions and many uncertainties. Lancet Glob Health. 2020. 8: e641-2
9. Lindsley WG, King WP, Thewlis RE, Reynolds JS, Panday K, Cao G. Dispersion and exposure to a cough-generated aerosol in a simulated medical examination room. J Occup Environ Hyg. 2012. 9: 681-90
10. Luo M, Cao S, Wei L, Tang R, Hong S, Liu R. Precautions for intubating patients with COVID-19. Anesthesiology. 2020. 132: 1616-8
11. Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health. 2020. 5: e475-83
12. Ozma MA, Maroufi P, Khodadadi E, Kose S, Esposito I, Ganbarov K. Clinical manifestation, diagnosis, prevention and control of SARS-CoV-2 (COVID-19) during the outbreak period. Infez Med. 2020. 28: 153-65