Abstract
Background
During the COVID-19 crisis, a new nurse and doctor-led telephone triage model of care was evaluated as a method of prioritising essential visits to the ophthalmic accident and emergency department in the Royal Victoria Eye and Ear Hospital. This new method of service is known as “Telehealth” or “E-Health”.
Aims
To assess the safety and efficacy of a Telehealth model of care ultilised during the COVID-19 pandemic.
Methods
A prospective study was undertaken in the Royal Victoria Eye and Ear Hospital where the telephone triage records were examined over a 28-day period during the COVID-19 pandemic from 19 March 2020 to 16 April 2020 inclusive.
Results
During this period, 1120 telephone calls were received by the call centre. A total of 739 patients attended the emergency department over the 28-day period compared to 2247 during the same period in 2019.
Conclusion
To reduce risk of transmission, the COVID-19 pandemic has necessitated novel ways of interacting with patients and sharing healthcare information. Our new mode of service provision in the RVEEH portrays the effectiveness of Telehealth. This study gives us further scope to improve this model of care into the future.
Similar content being viewed by others
Introduction
The Royal Victoria Eye and Ear Hospital (RVEEH) is a specialised hospital for ophthalmic and ENT conditions. Prior to March 2020, the ophthalmic emergency department (ED) provided a 7-day walk in service from 9 a.m. to 7 p.m. and a 24-h on-call emergency service. On average, the ophthalmic ED department assessed 100 patients per day and over 30,000 patients per year [1]. The provision of efficient medical care to patients proved to be a challenge with such high numbers due to safety and staffing issues. Historically, all patients were first triaged by a casualty nurse and then were assessed by NCHDs or community ophthalmologists on site. There is restricted space in both our waiting room (which measures 40 m2 with a capacity for 14 chairs) and our clinical areas, and it was common for three doctors to examine their patients in a room measuring 15 m2, a practice which was not feasible during the COVID-19 pandemic. It was not unusual for patients to wait for 6–8 h, often for non-emergency conditions such as dry eyes or blepharitis. Patients were either self-referred or referred by their GP, optometrist, or another hospital in the catchment area [2].
The COVID-19 outbreak, which began in December 2019, presented a significant challenge for the entire world. The pandemic had its initial impact on the healthcare setting in March 2020. The large number of cases worldwide has prompted the HSE to introduce measures to curtail non-essential visits to hospitals. In line with this, the RVEEH has initiated a care delivery system involving information and communications technologies called Telehealth, primarily a nurse-led telephone triage system. As of 16 March 2020, an appointment only service came into operation.
Telemedicine is the utilisation of technology to provide healthcare services to patients who are at a distant location with respect to the healthcare provider [3]. Rather than being a single technology, telemedicine is part of a wider process or chain of care. It has been assumed that telemedicine can improve this chain of healthcare provision and thus enhance the quality and efficiency of patient care. Telemedicine can further increase the fairness and equality of the distribution of health services, because the accessibility of care, especially in remote areas, can be improved.
Our model of Telehealth was primarily a nurse-led phone-in triage system. The service is run by an experienced senior nurse, which met one of the following criteria: (1) an advanced nurse practitioner (ANP), (2) clinical nurse specialist, (3) nurse with a post-graduate diploma with 6-month ED experience or (4) a general staff nurse with 2-year ED experience. There were two nurses along with one NCHD/consultant on the telephone triage telephone line from 8 a.m. to 8 p.m. daily.
Patients can access the service by contacting the dedicated telephone triage number, or their GP can refer them electronically via Health Link. All patients had a tele-consultation prior to their appointments. Health Link is a messaging service that allows patient information to be securely transferred between hospitals and medical practitioners. Patients are initially registered by the administration staff. The triaging team then ring all registered patients and conduct a conversation with the patient regarding their signs and symptoms.
Embedded into the service is the ability to email photos to a dedicated email address to assist with clinical decision making.
Based on the telephone conversation, the triaging member of staff will determine if the patient needs advice, a physical appointment or a referral to a different hospital or service. In some situations, it may be deemed necessary to send a prescription to the patient. This can be emailed to an appropriate pharmacy via Healthmail as required. The new model of care was shared with the Ireland East Hospital Group (IEHG), and an emergency ophthalmic guideline was developed ensuring standardised care across the IEHG.
The aim of this study is to determine the safety and efficacy of the new telephone triage service that was introduced to the ED. The future value of this study is to ensure that the Telehealth model ensures appropriate referral to the service, is safe and effective and will reduce patient flow times through the department.
Method
A prospective study was undertaken, authorised by the institutional review board in the RVEEH ED from 19 March to 16 April 2020. All ophthalmic patients registered by the telephone triage system were enrolled in the study. The inclusion criteria were patients who self-registered, referrals by GPs (general practitioners), opticians and other hospitals. The exclusion criteria were ear, nose and throat (ENT) patients and duplicate patients. Control data was obtained by comparing results to the number of ED attendees in the same period in 2019. An episode counted as a telephone call to the dedicated triage number. The following information was collected from the triage notes: urgency of referral, patient demographics, reason for referral, suspected nursing diagnosis, whether a picture was sent, triage time for appointment if granted, diagnosis by NCHD (non-consultant hospital doctors) and follow-up outcome. All information obtained and information given was recorded on either the telephone triage sheet, ED card or the patient’s healthcare record and scanned into the Informa patient episode recording system. Statistical analysis was collated and preformed using Microsoft Excel in conjunction with the Data Analysis ToolPak add-in feature.
To determine efficacy, we compared the number of patients seen in the emergency department from 19 March to 16 April 2020 with the number of patients seen in the same period in 2019. To prove that the implementation of the Telehealth triage system was safe, we looked at the number of patients who called the service and were initially given advice over the phone from a triaging member of staff but who later rang back again with worsening symptoms requiring an appointment in the emergency department. Figure 1 illustrates the flow process involved in triaging. Figure 2 shows us the triaging categories used by nursing staff to prioritise patient’s needs.
Results
Patient demographic data showed a 51%/49% male-to-female ratio, with the mean age of 50 years.
Fifty-one percent of patients presented from South Dublin, 15% North Dublin and 34% from outside Dublin (Graph 1). The total number of calls received over the 28-day period was 1120. Sixty-three of these were self-referrals, 15% were referred via their GP, 1% by opticians and 3% by other hospitals (Graph 2, 3).
There were 1120 episodes (i.e., calls to the triage number/referrals from Health Link, opticians or other hospitals). Of the 1120 episodes, 79 patients made 2 calls to the service, 1 patient made 3 calls to the service and 3 patients initially called the triage number and were registered by the secretarial staff but did not respond when the nursing staff called them back. One hundred seventy-nine notes or charts were unobtainable. Sixteen ENT calls/patients were excluded as were any OPD queries resulting in 898 patients. There was an average of 55–60 calls a day peaking at 77 with an average of 37.5 patients been seen daily Monday–Friday. On Saturdays, initially 20–38 calls with 14 patients seen and Sunday 20 calls and an average of 10 patients seen.
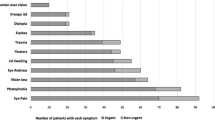
Figures 3, 4 portray the number of patients falling under each triage category along with the suspected diagnosis. Acute emergencies accounted for 2.5% of all patients seen. Eighteen percent of patients who contacted our service required an appointment on the same day while 34.5% required an appointment within 3 days. A further 33% required general advice and finally nursing staff sought advice from NCHDs for 12% of cases. These patients were initially discussed by the triage nurse with the NCHD/consultant prior to deciding whether an appointment was required. There were 7 emergency admissions over the 28 days: 5 retinal detachments, 1 retinal tear and 1 optic neuritis.
The validity of diagnosis was negatively highlighted in 8 patients who were initially diagnosed by the telephone triage staff as one condition but who subsequently called the service on a second occasion and were offered an appointment. At this emergency department consultation, their diagnosis and treatment differed from their initial diagnosis (0.8%) (Fig. 5).
Patient flow times through the department were evaluated. The time taken from check-in to being assessed by the nurse 15 min.
Discussion
This study demonstrates a significant decrease in the number of ophthalmic emergency department visits over the initial months of introducing a Telehealth service model in the Royal Victoria Eye and Ear Hospital. A total of 739 patients were physically seen the emergency department in a 4-week period in comparison with 2247 patients seen in the equivalent period on 2019. This represents a reduction of 67.1%. A total of 1120 calls were made to the triage service during this period. Whilst there is without doubt a reduction of one-third of patients attending the department, this is associated with the confounding factor that the number of patients visiting any hospital facility was drastically reduced during the first wave of the COVID-19 pandemic due to the fear of spreading or contracting the highly contagious virus. Going forward as more people become vaccinated, this fear will no doubt dissipate.
For evaluation of safety, we examined the number of patients that had the wrong diagnosis or suffered mismanagement as a result of Telehealth. This consisted of eight patients who made further contact with the triaging service, after their initial consultation did not lead to resolution of their symptoms. This subsequently required them to attend the emergency department for a physical examination. The overall rate of misdiagnosis was 0.8% which could lead to long-term ocular morbidity.
However, safety is a difficult parameter to measure whilst using a Telehealth method. Other studies which looked at the safety of Telehealth models made direct comparison between a control group using the traditional model of care and the new Telehealth model. For example, Muller et al. [4] evaluated long-term treatment outcomes and safety of telemedicine consultations for non-acute headaches in a Norwegian population. Patients were randomised to traditional physical examination or a teleconference meeting. Patients were then followed up with a questionnaire at 3 and 12 months to evaluate for the resolution of symptoms. Chen et al. [4] evaluated the safety of Telehealth in poorly controlled type 2 diabetes mellitus patients in Taiwan. This study compared treatment results of patients receiving additional Telehealth treatment and controls receiving only conventional treatment. Both of these studies therefore had a control group to evaluate safety. Unfortunately in setting up the new triage service in the RVEEH hospital, due to the sudden emergence of the COVID-19 into society and the urgency in which the service was set up, it was not possible to create a control group. Therefore, we can only extrapolate safety from the low number of patients that needed to re-access the service on a subsequent phone call. Going forward, further safety parameters should be put in place to consistently evaluate the safety of the service.
Whilst this is a new patient service for the RVEEH, triaging systems are widely used worldwide to identify and treat patients with the highest clinical need. On accessing the literature, a number of articles were found which described similar services as is provided in the RVEEH. An important example was the creation of a virtual eye casualty in Moorfields Eye Hospital in London. This was introduced in March 2020 and utilised a platform supporting patient to doctor live video consultations. On this platform, suitable patients contacted nurse-led telephone lines and if deemed appropriate were directed towards the video service. This was then staffed by 3–5 ophthalmologists. An audit was undertaken in the first 6 weeks of use during which 331 video consults occurred. It was found that 78.6% of patients avoided hospital attendance by undertaking in a video consult. Following video consultation, 21.4% were found to need hospital review. Moorfields eye casualty attendance reduced from 250 patients per day to an average of 64. An average of 38 patients were initially seen via the video consultation system in the first 12 days. This number increased in 150 daily later in its introduction [5]. For the purposes of emergency eye care, triaging ensures that those with the highest clinical risk are seen urgently and in a hospital setting and those with lower clinical risk are streamed to self-manage or are seen in a more appropriate setting and timing [6]. Triaging also helps to increase patient flow through the department. The initial check-in to the time that the patient was first assessed by a nurse fell from 35 min in pre-COVID times to 15 min on setting up this service. This was largely due to patients arriving at the hospital at a specified appointment time.
Whilst this new triage system has proven extremely efficacious, it does not come without fault which going forward can be improved on to maximise patient care. Firstly, the literature indicates cautionary tales regarding the cessation of walk-in services which failed due to lack of engagement with the wider community, i.e. GPs/COPs (community ophthalmic physicians) local optometrists, hospitals, etc. However, it has been shown that communication, education and access to the service are keys for its successful continuation. To this end as of 13 July 2020, the presence of a dedicated ophthalmic NCHD was initiated as part of the Telehealth team which enabled doctors in the community to discuss patients, doctor to doctor. This dedicated resource facilitates medical review call backs, better gatekeeping and decision making to ensure appropriate referrals from the community. Senior medical doctors dedicated to Telehealth, who can review appointments and develop clear access routes to subspecialties, have the ability to improve efficiency and optimise capacity in the triage setting. It is also important going forward to upskill community GPs and optometrists in basic ophthalmic knowledge. This has been cited as beneficial in previous studies to improve triaging [7].
Secondly in this modern era, physicians are increasingly aware that electronic medical records can help to improve communication in both referrals and feedback processes. It eliminates difficulties finding notes and ensures continuity of care. However from our study, we can see that 179 charts were unavailable for review at the time of data retrieval. Further investment in the electronic patient record system is necessary going forward. Leading on from this further investment is required on the hospital’s website to ensure as much information is available online as a source of support to patients. In line with the people strategy, patients, staff and the wider community will be involved in the design and delivery of the service as it moves forward [8]. This has begun with a patient survey carried out on 15 September 2020 which indicated that all patients had positive experiences with one indicating it was an excellent experience.
Lastly, the funding of this new service has yet to be properly addressed. To date, there is no charge for professional advice or prescriptions sent to patients who are not required to attend the ED. This requires further exploration with the hospital group to ensure that it is viable going forward.
This has been a major organisational change for staff and patients. Access, evaluation and engagement around operational issues and staff well-being are paramount and will add value to staff dedicated to this service.
Additional remodelling will be necessary going forward to ensure effective utilisation of the service as this data was acquired during the early phases of the pandemic when patient demand was drastically suppressed.
Conclusion
Following the emergence of the COVID-19 pandemic, the ED department in the RVEEH has been limited by infrastructure and social distancing constraints with capacity for only 50 ophthalmic appointments a day, which is 50% of the previous capacity. With many eye diseases rising sharply in prevalence with increasing age, this will continue to be a growing demand for ophthalmic emergency services. Telehealth is the way forward to ensure that the right patient gets the right service by the right staff at the right time. This study supports a new innovative model of care and demonstrates the safety and effectiveness of nurse-led triage. Nurse-led telephone triage is only the beginning.Further investment in workforce planning, senior medical involvement, communication, strengthening community links and digitalisation with emphasis on audit, data collection, outcome measures and virtual platforms will ensure that Telehealth is the future of safe quality healthcare in ED in the Royal Victoria Eye and Ear Hospital.
References
Al-Arrayedh H, O’Doherty M, Murphy C, O’Reilly F (2010) An audit of primary care referrals to the Ophthalmic Accident and Emergency Department of the Royal Victoria Eye and Ear Hospital. Dublin Ireland Student Med J 3:25–28
Prendiville C, Nasser Q, McGettrick P (2008) Patients presenting to an Ophthalmic Emergency Department after 5pm. Ir Med J 101(4):116–118
Caffery LJ, Taylor M, Gole G, Smith AC (2019) Models of care in tele-ophthalmology: a scoping review. J Telemed Telecare 25(2):106–122
Müller KI, Alstadhaug KB, Bekkelund SI (2017) A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology 89(2):153–162
Kilduff CL, Thomas AA, Dugdill J et al (2020) Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ health & care informatics 27(3)
Buchan J (2015) The Way Forward – Options to help meet demand for the current and future care of patients with eye disease. Emergency Eye Care. The Royal College of Ophthalmologists [Internet]. [Available from: Jan 2021] https://www.rcophth.ac.uk/wp-content/uploads/2015/10/RCOphth-The-Way-Forward-Emergency-Eye-Care-300117.pdf (Assessed Jan 2021)
Fenton S, Jackson E, Fenton M (2001) An audit of the ophthalmic division of the accident and emergency department of the Royal Victoria Eye and Ear Hospital. Dublin Irish medical journal 94(9):265–266
Health Service Executive – Human Resources Division (2019) People Strategy 2019–2024. Dublin, Ireland: Health Service Executive
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was performed in compliance with the principles of the Declaration of Helsinki. The ethics committee-decided approval was not necessary for this study as it consisted of retrospective chart review with no additional patient contact and no extra procedures performed.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hanrahan, G., Ennis, C., Conway, M. et al. An evaluation of the safety and effectiveness of telephone triage in prioritising patient visits to an ophthalmic emergency department — the impact of COVID-19. Ir J Med Sci 191, 2393–2398 (2022). https://doi.org/10.1007/s11845-021-02806-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02806-w