Abstract
The COVID-19 pandemic caused by the SARS-CoV-2 virus made governments across the world announce country-wide lockdowns suspending all activities and banning travels. This affected the lives of millions of people across all the continents in the world, including South America. The low-income classes were most affected by the lockdowns as many lost their only source of income. In addition, the uncertainty of the disease and its deadly nature along with lack of access to correct information led to a deterioration of the mental health of the low-income and indigenous groups in South America. The low-income population has little chance of gaining access to proper mental healthcare as many healthcare systems collapsed due to the nature of the pandemic. A good number of them faced short-term mental effects such as anxiety and panic attacks as well as long-term effects of depression. Proper steps must be taken to maintain and help the most vulnerable sections of the population. The pandemic along with the widespread poverty-stricken regions in the country have affected the population of the country. This article assesses the impact of COVID-19 on the poor and low-income population of the South American continent and the impact it has had on their mental health. It also reviews the recommended steps that can be taken to improve the situation and help the affected people.
Similar content being viewed by others
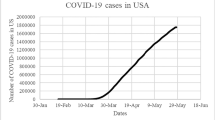
The beginning of the current decade found the globe under a plethora of sufferings caused by the fatal respiratory illness — COVID-19. The epicentre of the disease was located in Wuhan, China, where it first emerged in December 2019 and the virus reached all corners of the world within a matter of few months. Consequently, the disease was declared a pandemic by WHO on March 11, 2020. Across the world, the disease was initially seen affecting higher-income groups returning from abroad to their home countries and their close contacts but spread rapidly to lower-income populations taking everyone in its clenches (Garcia et al., 2020). One of the regions worst hit by COVID-19 is South America, particularly Brazil.
South America is located mostly in the south-western hemisphere and has a high population. Despite the diversity in the countries, what is common to all is wide inequalities in income, effective access to healthcare services and health outcomes which makes the area the most inequitable region in the world (Garcia et al., 2020). The first case of SARS-CoV-2 infection in Latin America was reported on February 26, 2020, in Brazil and the first death from COVID-19 was reported on March 7 in Argentina. By March 19, every country in LA had reported SARS-CoV-2 infections (COVID-19 map., 2020). As of June 1, 2021, a total number of 28,813,102 confirmed cases were recorded in South America with 780,486 deaths (https:, , www.worldometers.info, coronavirus & utm_campaign=homeAdUOASi%3Ca%20href=[Accessed June1, 2021). Of this figure, Brazil and Argentina top the list with 16,547,674 and 3,781,784 cases, respectively (https:, , www.worldometers.info, coronavirus & utm_campaign=homeAdUOASi%3Ca%20href=[Accessed June1, 2021).
The highly mutable nature of the virus only added to the misery of people in the region. The P.1 variant, first detected in travellers to Japan from the city of Manaus, in the Brazilian Amazon, was reported to be the result of mutations on the spike protein that made it 1.4 to 2.2 times more transmissible (Centre of Infectious Disease Research & Policy 2021). The variant accounted for 73% of cases in the state capital Manaus by January 2021 as Brazil shares borders with 10 countries; the spread of the variant to neighbouring countries was inevitable (Centre of Infectious Disease Research & Policy 2021).
Therefore, it is clear that combating the pandemic is a big challenge in the region. However, besides the effects of the variants on physical health, the pandemic and resulting lockdowns have had numerous direct impacts on the population particularly those at the poverty level. The WHO in its report, ‘Bridging the Gaps’ (1995), emphasised on poverty being a trigger to physical and mental disabilities (Murali & Oyebode, 2004). The inability to acquire good nutrition, sanitation or other resources directly elaborates the relationship between physical health and poverty. But the distress, the alienation and helplessness caused by poverty relate to mental health disorders, particularly depression. Besides, it is the poor who are more often exposed to stressful and unrewarding work or are forced to do jobs outside of their comfort zone which makes them all the more vulnerable (Murali & Oyebode, 2004).
In addition to affecting adults, the sense of deprivation plays a critical role in shaping the mental health status of children throughout their development. A strong sense of alienation has shown to pull young children into petty acts like thievery as well. Therefore, there is an intimate relationship between mental health disorders and poverty (Knifton & Inglis, 2020). Hence, our article will be assessing the impact of COVID-19 on the poor in the South American continent and how it has impacted their mental health.
Situational Analysis: South America
Pre-COVID-19 Era
A study published in 2003 claimed that Latin America contributed to 10.5% of the world’s total burden of neuropsychiatric disorders. It also estimated that in the year 2000, 18 million people in the region suffered serious financial setbacks due to poor mental health (Alarcón, 2003).
In the following decade, a 2012 WHO report stated that 5% of the adult population in Latin America suffered from depression and six out of these ten do not even have access to treatment (https://www3.paho.org/hq/index.php?option=com_content&view=article&id=7305:2012-dia-mundial-salud-mental-depresion-trastorno-mental-mas-frecuente&Itemid=1926&lang=en).
Thus, the mental health conditions of the people of this area have always been in the grey. Considering the pattern of declining mental health with fall in income, a decline in quality can be projected owing to financial losses due to the pandemic.
The Impact of COVID-19 on Poverty Level in South America
South America is one of the emerging economies, and like every country and region in the world, its economy is also adversely affected by this COVID-19 pandemic.
Gross Domestic Product (GDP) dropped by 8.1% in Latin America as a result of the ongoing pandemic (Centre of Infectious Disease Research & Policy 2021). Thus, the poor have been the most adversely affected. According to the World Data Lab, the International Poverty Line in 2011 PPP is $1.90 per day with $3.20 and $5.50 introduced as ‘higher poverty values’ by the World Bank (https://worlddata.io/blog/a-broader-view-of-poverty-in-south-america). Hence, before the pandemic, the higher-income countries were Uruguay, Chile and Argentina with 2.3%, 6% living on less than $5.50 per day in the first two countries and 1% living on less than $1.90 daily in Argentina. Brazil, Peru, Ecuador, Colombia, Paraguay, Suriname and Guyana all belong to ‘upper-middle-income countries’ and Bolivia, lower-middle-income countries. A total of 4.5–29% of the population of these countries is living below $3.20 and $5.50. Venezuela had the highest percentage of the lower-income population with an estimated 9 million people with less than $1.90 daily (https://worlddata.io/blog/a-broader-view-of-poverty-in-south-america). Although there are no current specific statistics showing poverty levels in each of the countries affected by the pandemic, it is notable that the COVID-19 pandemic has resulted in an increased gap between the poor and the rich. The Economic Commission for Latin America and the Caribbean (ECLAC) projects that ‘as a result of the steep economic recession in the region, which will notch a − 7.7% drop in GDP — it is estimated that in 2020, the extreme poverty rate was 12.5% while the poverty rate affected 33.7% of the population. This means that the total number of poor people rose to 209 million by the end of 2020, affecting 22 million more people than in the previous year. Of that total, 78 million people found themselves living in extreme poverty, or 8 million more than in 2019’ (https://www.cepal.org/en/pressreleases/pandemic-prompts-rise-poverty-levels-unprecedented-recent-decades-and-sharply-affects).
The COVID-19 pandemic has, therefore, resulted in worsening the condition of poverty, especially in the rural areas where people have lost their livelihood and now cannot access healthcare facilities to protect themselves from this pandemic (https://www.cepal.org/en/pressreleases/pandemic-prompts-rise-poverty-levels-unprecedented-recent-decades-and-sharply-affects).
The Mental Health Implications
A large gap in mental health has been exposed by the COVID-19 pandemic across many regions including South America. The mental health needs of the population are given less priority when the pandemic has led to scarce resources, weakened the already fragile health systems and led to unrest and violence due to the COVID-19 containment strategies. The low-income groups will be the most affected by the pandemic and will experience long-term consequences on their mental health (Kola et al., 2021).
Immediate impacts of the pandemic on mental health are the increased signs and symptoms of mental distress experienced by the masses. These symptoms can be due to factors such as the infectious nature of the disease, the consequences of containment and whether normalcy will ever be returned in everyday life. Some of the long-term effects of the pandemic include mood disorders and a rise in suicide due to stress, poverty, unemployment and social isolation. Many of the indigenous people living in remote and rural areas have been affected the most due to a lack of access to information and quality health services. Some of the other barriers include intercultural barriers such as different languages and traditions of the indigenous population. The lower-income population is also vulnerable to mental distress and mental illness due to factors such as overcrowded living conditions, less access to health services and lesser availability of education or employment opportunities. Mental health disorders can affect the wage-earning capacity of the low-income population as it decreases the capacity of an individual’s normal functioning (Kumar & Kumar, 2020).
In times past, the topic of mental health and mental disorders was attached with stigma. The COVID-19 pandemic has worsened the situation and has led to an increase in the incidence of health inequalities and also to lower access to mental health services. People with mental health illnesses have to face discrimination at work and lower access to health facilities. Mental health services such as regular clinical visits and telecare have been affected by the pandemic especially for the older population residing in nursing homes (Access to mental health in Latin America amid COVID-19 [Internet]., 2020). Due to a decrease in access to these services, people are experiencing various symptoms such as social isolation and stress as well as sleep disturbances. Anxiety and agitation are also common symptoms being observed. Natural disasters such as Hurricane Maria and the earthquake in Puerto Rico have also led to an increase in poor mental health (Access to mental health in Latin America amid COVID-19 [Internet]., 2020).
Stigma Around Mental Health in South America
In a study conducted by Mascayano et al., a narrative review of the expression of stigma and prejudice around mental illness was closely studied (Mascayano et al., 2016). There has been an increase in the information that is now available around the stigma associated with mental illnesses, but these findings have not yet been applied in mental health services that are provided in South America (Mascayano et al., 2016). Studies have shown that people had negative prejudice against others facing mental illnesses and categorised them as dangerous. Also, many mental health professionals had negative attitudes towards the people suffering from conditions like schizophrenia (Leiderman et al., 2011).
In a study conducted by Hickling et al., it was observed that family members and community members had more positive attitudes towards mental illnesses when the primary health care network also included community mental health services (Hickling et al., 2011). Also, the compassion and benevolence towards individuals with mental illness is likely to grow if proper information is available for the general public (Masayano et al., 2016).
Steps Taken to Improve Mental Health
Some of the steps taken by healthcare providers to improve mental health during this pandemic in the region include the following:
-
Community Outreach
Some government agencies and local communities have identified people in need of mental health services and supported them to access these services. Many humanitarian organisations have also arranged for people in need, virtual support meetings and online resources (Access to mental health in Latin America amid COVID-19 [Internet]., 2020).
-
Online delivery of mental health services is a good alternative for home-based treatment as an alternative to in-patient treatment reducing the chances of spreading COVID-19 by maintaining physical distance norms (Access to mental health in Latin America amid COVID-19 [Internet]., 2020).
Mass communication media at both national and local levels has helped facilitate the spreading of correct information among the masses. For physiosocial education and information, to support cultural and gender perspectives was also spread through this mode of communication. The use of telemedicine and local as well as national hotline mental health services was being provided to the public. To facilitate the delivery of pharmacological treatments to patients, virtual delivery systems were set up in partnership with the pharmaceutical networks that were already set up to allow easier access to quality services and treatment options (Antiporta & Bruni, 2020).
In addition to this, in Central America, people suggested the formation of mental health technical working groups that would continue to provide mental health services even after in a post pandemic setting. To enhance mental health, it is important that there are partnerships between local and civil organisations. To tailor the services according to the needs of the population, a community-based system could be set up. For monitoring of mental health burden, a system that is timely and robust should be set up to better inform the authorities (Antiporta & Bruni, 2020).
Conclusion and Recommendations
It is clear that indeed the COVID-19 pandemic has had a tremendous impact on the mental health of the lower-income class in South America and several strategies have been developed to eradicate or minimise this impact, particularly the use of technology. Technology has helped in all spheres of life since the onset of the pandemic, in education, work, telemedicine or self-help treatments. However, the internet required for these activities is not accessible to all classes of the population. Many of the essential services are thus inaccessible to older adults, the low-income population and people who are not familiar with technology usage. Free access to the internet must be provided to all, especially the disadvantaged communities of the population. It is also necessary that more research is conducted to find long-term alternative plans to provide mental health services to the vulnerable groups of the population (Access to mental health in Latin America amid COVID-19 [Internet]., 2020). In addition to this, as many institutions and workplaces open across the countries, various organisations should institute mental health plans for their workers to cater to their mental needs. Also, more awareness should be created on mental health and activities that help boost mental health.
Data Availability
Data availability does not apply to this article as no new data were created or analysed in this study.
References
Access to mental health in Latin America amid COVID-19 [Internet]. Borgenmagazine.com. 2020 [cited 2021 Jun 1]. Available from: https://www.borgenmagazine.com/mental-health-in-latin-america/
Alarcón, R. D. (2003). Mental health and mental health care in Latin America. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 2(1), 54–56.
Antiporta, D. A., & Bruni, A. (2020). Emerging mental health challenges, strategies, and opportunities in the context of the COVID-19 pandemic: Perspectives from South American decision-makers. Revista Panamericana de Salud Pública, 44.
Centre of Infectious Disease Research and Policy https://www.cidrap.umn.edu/news-perspective/2021/03/covid-surges-strain-health-systems-parts-south-america [Assessed May 21, 2021]
Garcia, P. J., Alarcón, A., Bayer, A., Buss, P., Guerra, G., Ribeiro, H., Rojas, K., Saenz, R., Salgado de Snyder, N., Solimano, G., Torres, R., Tobar, S., Tuesca, R., Vargas, G., & Atun, R. (2020). COVID-19 Response in Latin America. Am J Trop Med Hyg., 103(5), 1765–1772. https://doi.org/10.4269/ajtmh.20-0765
Hickling, F. W., Robertson-Hickling, H., & Paisley, V. (2011). Deinstitutionalization and attitudes toward mental illness in Jamaica: A qualitative study. Revista Panamericana De Salud Publica, 29, 169–176.
https://www.worldometers.info/coronavirus/?utm_campaign=homeAdUOA?Si%3Ca%20href= [Accessed June 1, 2021
Johns Hopkins Coronavirus Resource Center, 2020. COVID-19 map. Available at: https://coronavirus.jhu.edu/map.htmAccessed May 22, 2021. [Google Scholar]
Knifton, L., & Inglis, G. (2020). Poverty and mental health: Policy, practice and research implications. Bjpsych Bulletin, 44(5), 193–196. https://doi.org/10.1192/bjb.2020.78
Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. Lancet Psychiatry [Internet]. 2021; Available from: https://doi.org/10.1016/S2215-0366(21)00025-0\
Kumar, M., & Kumar, P. (2020). Impact of the pandemic on mental health in lower- and middle-income countries (LMICs). Glob Ment Health (camb)., 7(e35), 1–9.
Leiderman, E. A., Vazquez, G., Berizzo, C., Bonifacio, A., Bruscoli, N., Capria, J. I., et al. (2011). Public knowledge, beliefs and attitudes towards patients with schizophrenia: Buenos Aires. Social Psychiatry and Psychiatric Epidemiology, 46, 281–290.
Masayano, F., Tapia, T., Schilling, S., Alvarado, R., Tapia, E., Lips, W., & Yang, L. H. (2016). Stigma toward mental illness in Latin America and the Caribbean: A systematic review. Brazilian Journal of Psychiatry, 38, 73–85.
Mascayano F, Toso-Salman J, Sia KJ, Escalona A, Alvarado R, Yang LH. ‘What matters most’ towards severe mental disorders in Chile: A theory driven, qualitative approach. Rev Fac Cien Med Univ Nac CordobaForthcoming. 2016
Murali, V., & Oyebode, F. (2004). Poverty, social inequality and mental health. Advances in Psychiatric Treatment, 10(3), 216–224. https://doi.org/10.1192/apt.10.3.216
Author information
Authors and Affiliations
Contributions
Aparna Gupta conceived the idea and worked alongside Arnav Bansal Bansal, Arushi Kapoor and Esther Bassey in building the manuscript. Esther Bassey also reviewed the manuscript and created the outline for the writing process.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bassey, E.E., Gupta, A., Kapoor, A. et al. COVID-19 and Poverty in South America: the Mental Health Implications. Int J Ment Health Addiction 21, 2954–2960 (2023). https://doi.org/10.1007/s11469-022-00765-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-022-00765-6