Association of Viral Load in SARS-CoV-2 Patients With Age and Gender
- 1Clinical Laboratory Technology, Taibah University, Madinah, Saudi Arabia
- 2Regional Lab in Madinah, Ministry of Health, Madinah, Saudi Arabia
- 3Department of Laboratories and Blood Banks, Ministry of Health, Madinah, Saudi Arabia
- 4Clinical Laboratory Department, College of Applied Medical Sciences, Shaqra University, Shaqraa, Saudi Arabia
- 5Department of Family and Community Medicine, College of Medicine, Taibah University, Madinah, Saudi Arabia
Background: The coronavirus disease 2019 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), is a global public health emergency. Age and sex are two important factors associated with risks and outcomes of various diseases. COVID-19 morbidity also seems to be affected by patient age and sex. It has been found that older age groups have more severe COVID-19 symptoms and higher fatality rates while children tend to have lower prevalence and milder symptoms than adults.
Methods: The study reviewed electronic medical records of COVID-19 patients from Madinah city, Saudi Arabia. The study included all cases who tested positive (n = 3,006) between March 20 and May 22, 2020. Data were obtained from the Health Electronic Surveillance Network (HESN) database.
Results: Approximately 80% of the study sample were males and half were in the 30–40-year-old age group. The Ct value of the whole sample ranged from 15.08 to 35, with a mean of 27.44 (SD: 5.23; 95% C.I. = 27.25–27.66). The means of Ct values varied between age groups from 27.05 to 27.82. Analysis of the mean differences between age groups using one-way ANOVA indicated no statistically significant difference among the groups (F6,2999 = 1.63; p-value = 0.135). A comparison of mean Ct values of males (n = 2,422) and females (n = 584) revealed that males had a statistically significant higher mean Ct value (27.61 ± 5.20) than females (26.72 ± 5.31). The difference between the means of the two groups was −0.89 (95% C.I. = −1.36 to −0.42; t-test −3.71; df = 3,004; p-value < 0.001).
Conclusion: The study found no statistically significant difference in viral loads between age groups. It showed that females had a higher SARS-CoV-2 viral load compared to males. The findings have implications for preventive strategies. Further studies are needed to correlate viral load with clinical symptoms and outcomes.
Introduction
The coronavirus disease 2019 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), is a global public health emergency. The mortality and morbidity caused by the disease constitute a major challenge to healthcare authorities around the globe. The challenge has been aggravated by lack of knowledge of the epidemiological and clinical attributes of the emerging disease (1).
On the 2nd of March 2020, a Saudi man at the Eastern Province coming from Iran confirmed positive for COVID-19 (2). Since then, the Saudi Ministry of Health (MOH) took the case seriously and isolated the patient and all of the contacts. Spreading of the virus was dramatically and several cases were reported in the same region due to the same reason of transmitting the infection of the first case. Such a disease creates huge burden on health care providers and governments as that of MERS Co-V in 2012 (3). Additionally, the worries about re-infection is of a major concern, whoever, protection from reinfection has been reported (4).
Age and sex are two important factors associated with risks and outcomes of COVID-19 disease (5). COVID-19 morbidity also seems to be affected by patient age and sex. It has been found that older age groups have more severe COVID-19 symptoms and higher fatality rates while children tend to have lower prevalence and milder symptoms than adults (6). Nonetheless, the potential role of asymptomatic or mildly symptomatic children in transmitting infection cannot be disregarded and is still debated (7–9). Preliminary evidence also indicated that sex has a role in the disease epidemiology. For example, a study from China indicated that men are at higher risk of severe disease and mortality compared to women (10).
Studying viral dynamics and their variation among population subgroups may help in understanding the role of age, sex, and other factors in the disease's epidemiology. One uncertainty of the new disease is COVID-19's viral dynamics and how they relate to factors in the population. Prior studies revealed that viral load was associated with disease severity and the number of days since the beginning of symptoms (11, 12). However, evidence on the association between viral load and other factors, including age and sex, has not been conclusive. Some studies found that higher viral load in the respiratory system was associated with higher in-hospital mortality and morbidity (13), and a higher risk of transmission (14); other studies found no such relationship (11). Understanding viral load dynamics and covariates is critical for identifying protective measures for individuals and the general public. Therefore, this study investigates the association of viral load with the age and sex of COVID-19 patients.
Methods
Study Design
The study reviewed electronic medical records of COVID-19 patients from Madinah city, Saudi Arabia. The study included all cases who tested positive between March 20 and May 22, 2020. Data were obtained from the Health Electronic Surveillance Network (HESN) database. HESN is a web-based platform run by the Ministry of Health to integrate public health programs in order to detect and control diseases, and monitor the population's health.
Setting
Al-Madinah region has a population of 2.13 million. The main city in the region is Al-Madinah city, a holy city and home to the Prophet's Mosque. It attracts year-round visits from religious pilgrims from all over the world.
Procedure Used by MOH in Specimens Collection of SARS-CoV-2 Patients
The MOH obligates all the health care workers who collect specimens to use appropriate personal protective equipment (PPE) such as, eye protection, surgical mask, while dealing with suspected Covid-19 patients. They must collect the respiratory specimen under aerosol generating procedure; personnel should wear a particulate proficient N95 respirator. Additionally, specimens should be placed for carriage in leak-proof specimen bags (secondary container) that have a detached sealable pocket for the specimen, with the patient's name tag on the specimen container (primary container). HESN printed lab requisitions must be sent with samples and national lab reception report and result values must be informed on HESN on their consistent time.
In terms of sources of sample testing, the most generally tested sources are nasopharynx and oropharynx (15). However, viral RNA in several biological specimens such as stool, tears and blood has been detected with variable positivity rates (16). Two types of samples are usually requested by the physicians be collected from the patients. First, lower respiratory tract samples, containing endotracheal aspirate, bronchoalveolar lavage fluid or sputum. Second, upper respiratory tract samples, nasopharyngeal swab (with or without oropharyngeal swab) in viral transport medium in a single tube. If initial testing is negative, repeat testing should be accomplished in case of there is a high index of suspicion. Finally, all results should be reported via HESN starting from registering of the case, for test requested select COVID-19, and select the designated regional laboratory. During shipment of samples they should be at 2–8°C and ship on ice pack to lab. Samples can be stored at 2–8°C for ≤48 h, if longer storage is required, samples should be stored at −70°C. If sample is frozen at −70°C, ship on dry ice https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/Coronavirus-Disease-2019-Guidelines-v1.2.pdf.
Participants
All positive cases from Al-Madinah region were included in this analysis. Laboratory results of cases in the region were reported to the HESN database by the Al-Madinah Regional Lab. Epidemiological information on cases and samples originated from hospitals and primary healthcare centers in Al-Madinah region. In addition, samples collected during contact tracing or active surveillance were included in the HESN database.
Variables
The outcome was the cycle threshold (Ct) value as measured by quantitative reverse transcriptase polymerase chain reaction (RT-PCR) assay. Lower Ct values indicate higher viral load and vice versa. Positive cases were defined as cases having Ct value of <35 in their sample. Age was calculated based on the date of birth and the sample submission date. Age was divided into seven categories (under 10 years old, 10 – <20, 20 – <30, 30 – <40, 40 – <50, 50 – <70, and 70 years or older).
Statistical Analyses
Statistical analyses were performed using Stata 14.0 (StataCorp LLC, TX, USA). Data were presented as mean, standard deviation (SD), 95% confidence intervals (C.I.) or proportions as appropriate. One-way ANOVA was used to compare the differences of means between groups in a univariate analysis. Two-way ANOVA was used in a multivariable analysis to model the relationship between Ct values (outcome), and age group and sex (independent variables). Interaction was tested in the model. Equality of variances was assessed using Levene's Test.
Ethical Considerations
Data collection was required by MOH as a part of the public health surveillance system. This investigation was conducted according to international and national ethical guidelines and approved by the regional research ethics committee of the Madinah Health Directorate (IRB number H-03-M-084).
Results
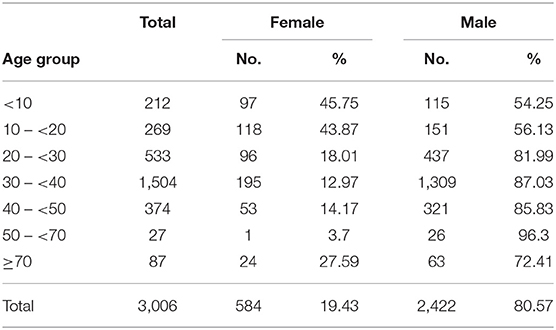
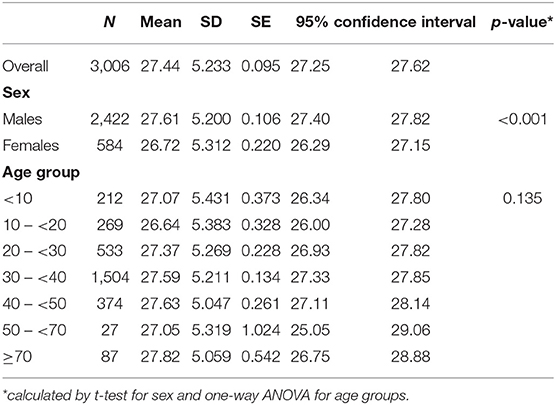
This study used data from the national HESN database. It included 3,006 positive COVID-19 cases reported in the Al-Madinah region from March 20 to May 22, 2020. Approximately 80% of the study sample were males and half were in the 30 to 40-year-old age group (Table 1). The Ct value of the whole sample ranged from 15.08 to 35, with a mean of 27.44 (SD: 5.23; 95% C.I. = 27.25–27.66; Table 2). The means of Ct values varied between age groups from 27.05 to 27.82.
Univariate Analysis
Analysis of the mean differences between age groups using one-way ANOVA indicated no statistically significant difference among the groups (F6,2999 = 1.63; p-value = 0.135).
A comparison of mean Ct values of males (n = 2,422) and females (n = 584) revealed that males had a statistically significant higher mean Ct value (27.61 ± 5.20) than females (26.72 ± 5.31). The difference between the means of the two groups was −0.89 (95% C.I. = −1.36 to −0.42; t-test −3.71; df = 3,004; p-value < 0.001).
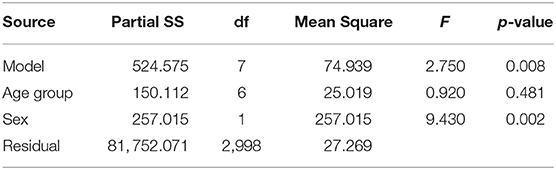
Multivariable Analysis
Two-way ANOVA analysis was conducted to examine the effect of age and sex on Ct value. There was no significant interaction between age and sex and Ct value (F = 1.61, p-value = 0.139). The main effect showed that the statistically significant difference between males and females persisted after adjustment for age group (p-value = 0.002). The two-way ANOVA analysis also showed no statistically significant difference between age groups (Table 3).
Discussion
This study compared COVID-19 viral load, as indicated by Ct value, across seven age groups, and between men and women. It found that viral load in patients did not differ by age group, but was higher among women than men. The argument in this study was that viral load is proportional to infectiousness of viral infections. The relationship between viral load and risk of transmission has been established in other viral diseases (17, 18); COVID-19 seemed likely to follow a similar pattern (19). Therefore, identifying factors related to viral load could aid prevention strategies and identification of groups contributing to higher transmission risk.
The distribution of viral load observed in this study is consistent with results from previous studies. In Switzerland, Jacot et al. (20) analyzed data on 4,172 positive patients and concluded there was no statistically significant difference between 5 year age groups. Another study from Switzerland compared 352 patients older than 16 years with 53 children under 16 years old and found a similar mean viral load between the two groups (21). Similarly, a study in the United States which included 4,428 patients with positive lab results found no variation in mean and median viral load values (22). Notably, other studies with smaller sample sizes had conflicting results regarding the relationship between SARS-CoV-2 viral load and age. One study of 23 patients concluded that older age groups had higher viral loads (23); another study (24) of 145 patients found that children under 5 years of age had higher viral loads.
This study found higher SARS-CoV-2 viral loads (lower Ct values) among females compared to males. Previous studies were not conclusive on the sex difference in viral load. Jacot et al. (20) and Kleiboeker et al. (22) reported comparable viral loads between males and females. Takahashi et al. (25) found the clinical status of patients was a modifier for the relationship between sex and viral load. Finding that sex effects viral load and immunological response to infectious disease is not surprising; it has been demonstrated in other diseases. This is thought to be related to a difference in immune response in which females develop a higher immune response to infectious agents, making them less susceptible to diseases (26). Gender differences in the response to hepatitis B virus were reported in humans as well (27). Similarly, sex difference seems to play a role in COVID-19 infection; various mechanisms have been suggested to explain this difference (28). Women mount stronger immune responses to infections as well as vaccinations and outlive men (29). As we do not have enough clinical data to investigate the disease severity and correlate that with age and gender, other study showed that men tended to get much sever cases than women. Additionally, older age was greater number in the deceased patients than in the patients who survived. However, several reports showed that there was no difference in terms of susceptibility to SARS-CoV-2 between women and men (10).
The present study provides evidence on age and sex differences in SARS-CoV-2 viral load in a large sample size. It also included a good number of young children who are often less represented in similar studies.
Limitations of the study are a lack of clinical data and the consequent inability to correlate laboratory values with illness stage or severity. Additionally, only respiratory tract specimens were considered and the study non-including alternative shedding routes and that could represent future developments of the study.
In conclusion, the study found no statistically significant difference in viral loads between age groups. It showed that females had a higher SARS-CoV-2 viral load compared to males. The findings have implications for preventive strategies. Further studies are needed to correlate viral load with clinical symptoms and outcomes.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Madinah Health Directorate (IRB number H-03-M-084). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
AA-Z and WM conceived and designed the study, conducted the preliminary review of articles, wrote the initial and final drafts of the article, and provided logistic support. AA-Z, WM, and AA provided research scope, and collected and organized the extracted data. AA-Z, WM, AD, and HA analyzed and interpreted the data, have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Xu T, Chen C, Zhu Z, Cui M, Chen C, Dai H, et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. (2020) 94:68–71. doi: 10.1016/j.ijid.2020.03.022
2. Alsofayan YM, Althunayyan SM, Khan AA, Hakawi AM, Assiri AM. Clinical characteristics of COVID-19 in Saudi Arabia: a national retrospective study. J Infect Public Health. (2020) 13:920–5. doi: 10.1016/j.jiph.2020.05.026
3. Al-Raddadi RM, Shabouni OI, Alraddadi ZM, Alzalabani AH, Al-Asmari AM, Ibrahim A, et al. Burden of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. J Infect Public Health. (2020) 13:692–6. doi: 10.1016/j.jiph.2019.11.016
4. Mahallawi W. Case report: a recovered SARS CoV-2 patient protected from reinfection. Front Med. (2020) 7:649. doi: 10.3389/fmed.2020.564264
5. Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. (2020) 11:6317. doi: 10.1038/s41467-020-19741-6
6. Naja M, Wedderburn L, Ciurtin C. COVID-19 infection in children and adolescents. Br J Hosp Med. (2020) 81:1–10. doi: 10.12968/hmed.2020.0321
7. Rajmil L. Role of children in the transmission of the COVID-19 pandemic: a rapid scoping review. BMJ Paediatr Open. (2020) 4:e000722. doi: 10.1136/bmjpo-2020-000722
8. Shane AL, Sato AI, Kao C, Adler-Shohet FC, Vora SB, Ery J, et al. A Pediatric infectious disease perspective of SARS-CoV-2 and COVID-19 in children. J Pediatric Infect Dis Soc. (2020) 9:596–608. doi: 10.1093/jpids/piaa099
9. Kim J, Choe YJ, Lee J, Park YJ, Park O, Han MS, et al. Role of children in household transmission of COVID-19. Arch Dis Child. (2020) 7:596–608:archdischild-2020-319910. doi: 10.1136/archdischild-2020-319910. [Epub ahead of print].
10. Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. (2020) 8:152. doi: 10.3389/fpubh.2020.00152
11. Walsh KA, Jordan K, Clyne B, Rohde D, Drummond L, Byrne P, et al. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Infect. (2020) 81:357–71. doi: 10.1016/j.jinf.2020.06.067
12. Wang Y, Zhang L, Sang L, Ye F, Ruan S, Zhong B, et al. Kinetics of viral load and antibody response in relation to COVID-19 severity. J Clin Invest. (2020) 130:5235–44. doi: 10.1172/JCI138759
13. Magleby R, Westblade LF, Trzebucki A, Simon MS, Rajan M, Park J, et al. Impact of SARS-CoV-2 viral load on risk of intubation and mortality among hospitalized patients with coronavirus disease 2019. Clin Infect Dis. (2020) 30:ciaa851. doi: 10.1093/cid/ciaa851
14. Shrestha NK, Marco Canosa F, Nowacki AS, Procop GW, Vogel S, Fraser TG, et al. Distribution of transmission potential during non-severe COVID-19 illness. Clin Infect Dis. (2020) 71:2927–32. doi: 10.1093/cid/ciaa886
15. Karia R, Nagraj S. A Review of viral shedding in resolved and convalescent COVID-19 patients. SN Compr Clin Med. (2020) 2:1–10. doi: 10.1007/s42399-020-00499-3
16. Morone G, Palomba A, Iosa M, Caporaso T, De Angelis D, Venturiero V, et al. Incidence and persistence of viral shedding in COVID-19 post-acute patients with negativized pharyngeal swab: a systematic review. Front Med (Lausanne). (2020) 7:562. doi: 10.3389/fmed.2020.00562
17. Bardeskar NS, Ahir-Bist SP, Mehta PR, Samant-Mavani P, Nanavati R, Mania-Pramanik J. Anti-retroviral therapy failure in HIV-1 infected pregnant women and its associated risk of HIV transmission. Arch Gynecol Obstet. (2020) 302:1229–35. doi: 10.1007/s00404-020-05743-8
18. Mayer BT, Krantz EM, Wald A, Corey L, Casper C, Gantt S, et al. Estimating the risk of human herpesvirus 6 and cytomegalovirus transmission to ugandan infants from viral shedding in saliva by household contacts. Viruses. (2020) 12:171. doi: 10.3390/v12020171
19. He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. (2020) 26:672–5. doi: 10.1038/s41591-020-0869-5
20. Jacot D, Greub G, Jaton K, Opota O. Viral load of SARS-CoV-2 across patients and compared to other respiratory viruses. Microbes Infect. (2020) 22:617–21. doi: 10.1016/j.micinf.2020.08.004
21. Baggio S, L'Huillier AG, Yerly S, Bellon M, Wagner N, Rohr M, et al. SARS-CoV-2 viral load in the upper respiratory tract of children and adults with early acute COVID-19. Clin Infect Dis. (2020) 6:ciaa1157. doi: 10.1101/2020.07.17.20155333
22. Kleiboeker S, Cowden S, Grantham J, Nutt J, Tyler A, Berg A, et al. SARS-CoV-2 viral load assessment in respiratory samples. J Clin Virol. (2020) 129:104439. doi: 10.1016/j.jcv.2020.104439
23. To KK, Tsang OT, Leung WS, Tam AR, Wu TC, Lung DC, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. (2020) 20:565–74. doi: 10.1016/S1473-3099(20)30196-1
24. Heald-Sargent T, Muller WJ, Zheng X, Rippe J, Patel AB, Kociolek LK. Age-related differences in nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate Coronavirus Disease 2019 (COVID-19). JAMA Pediatr. (2020) 174:902–3. doi: 10.1001/jamapediatrics.2020.3651
25. Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. (2020) 588:315–20. doi: 10.1101/2020.06.06.20123414
26. Park MD. Sex differences in immune responses in COVID-19. Nat Rev Immunol. (2020) 20:461. doi: 10.1038/s41577-020-0378-2
27. Mahallawi W. Persistence of hepatitis B surface antibody and immune memory to hepatitis B vaccine among medical college students in Madinah. Ann Saudi Med. (2018) 38:413–9. doi: 10.5144/0256-4947.2018.413
28. Bunders MJ, Altfeld M. Implications of sex differences in immunity for SARS-CoV-2 pathogenesis and design of therapeutic interventions. Immunity. (2020) 53:487–95. doi: 10.1016/j.immuni.2020.08.003
Keywords: SARS-CoV-2, age, gender, CT value, HESN
Citation: Mahallawi WH, Alsamiri AD, Dabbour AF, Alsaeedi H and Al-Zalabani AH (2021) Association of Viral Load in SARS-CoV-2 Patients With Age and Gender. Front. Med. 8:608215. doi: 10.3389/fmed.2021.608215
Received: 19 September 2020; Accepted: 08 January 2021;
Published: 27 January 2021.
Edited by:
Marco Iosa, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
Omar Khabour, Jordan University of Science and Technology, JordanAngela Palomba, University of Campania Luigi Vanvitelli, Italy
Copyright © 2021 Mahallawi, Alsamiri, Dabbour, Alsaeedi and Al-Zalabani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Waleed H. Mahallawi, wmahallawi@gmail.com
 Waleed H. Mahallawi
Waleed H. Mahallawi Ali Dakhilallah Alsamiri2
Ali Dakhilallah Alsamiri2  Hamdah Alsaeedi
Hamdah Alsaeedi Abdulmohsen H. Al-Zalabani
Abdulmohsen H. Al-Zalabani