- 1Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Globally, a lot of countries put into practice early quarantine measures as an essential COVID-19 prevention mechanism. Other than physical effects, quarantine has a major result on mental health and well-being at both the individual as well as the community level at large. Therefore, this study aimed to assess the psychological burden of COVID-19 on the people in quarantine and isolation centers and to identify associated factors for early and effective psychosocial intervention during the pandemic and beyond.
Method: A cross-sectional study was done among 392 suspected cases of COVID-19 that were in quarantine and isolation centers found in Eastern Ethiopia in 2020. Participants were selected by the convenience sampling method. The common mental disorder was measured by the Self Reporting Questionnaire-20 (SRQ-20). Logistic regression was done to identify predictive factors, and a P < 0.05 was considered statistically significant.
Results: The common mental disorder among suspected cases of COVID-19 in Ethiopia was found to be 13.5% (95% CI: 10.2, 17.1%). Female (AOR = 1.52, 95% CI: 1.1, 2.92), known chronic medical illness (AOR = 7.0, 95% CI: 2.2, 21.8), inadequate accessibility of personal protective equipment (AOR = 6.1, 95% CI: 2.8, 13.3), poor awareness about the pandemic (AOR = 2.90, 95% CI: 2.71, 7.54), presence of symptoms of the disease (AOR = 5.3, 95% CI: 2.57, 11.1), and substance use (AOR = 2.7, 95% CI: 1.2, 6.1) were found to be associated with a common mental disorder.
Conclusion: The current study revealed that the common mental disorder was relatively high among suspected cases of COVID-19 in quarantine and isolation centers as compared with the general population. The results of the present study demonstrate that some subpopulations are more vulnerable to the pandemic's deleterious effects on mental health. Therefore, providing appropriate psychosocial intervention for the populations at risk is important to decrease the effect of common mental disorders among suspected cases of COVID-19.
Introduction
The novel coronavirus disease (COVID-19) was identified for the first time in Wuhan, China, in December 2019 (1), and the WHO affirmed it as a worldwide pandemic on March 11, 2020 (2). It is accompanied by respiratory conditions such as respiratory failure, respiratory distress syndrome, and septic shock. In most cases, patients with COVID-19 may improve without extraordinary management although those with advanced age and preexisting physical illnesses are highly prone to have severe symptoms and illness and may progress to death (1, 3).
Quarantine and isolation became increasingly applied around the world to contain the transmission of the virus (4). Besides practicing different COVID-19 control measures, such as hand washing or sanitizing, use of face masks, and physical distancing, most countries are demanding to provide economic assistance to several people who lost their jobs due to lockdown and closure of nonessential commercial activity (5, 6). Despite those control measures, in the framework of serious threats to everyone's health and livelihood with the irregularity of governance efforts, extensive mental health, substance use, and psychosocial problems seem estimated to occur, both directly from the pandemic and indirectly from the related economic recession. It is known that such a pandemic has a major impact on mental health, and this problem has been described as a “parallel epidemic” (7).
There are various reasons for the impact of the pandemic on mental health. People now are suddenly facing major changes in their daily life, working models, and social behaviors. It is not surprising that several individuals are showing acute fight-or-flight responses, such as increased anxiety levels, panic attacks, irrational fears up to paranoid-like convictions, and related behaviors (8, 9). Some are experiencing losses under traumatic circumstances, such as not being able to say goodbye to dying loved ones or the inability to offer proper burials (10, 11). The disease itself is multiplied as forced mass quarantine to battle COVID-19 can cause depression, anxiety, and distress (12) due to factors such as the sense of getting worried and loss of control (13). This can be severe if families need separation by the uncertainty of disease status, scarcity of essentials, economical constraints, and increased susceptibility to the disease, which usually get exaggerated by unclear information and inappropriate communications via media (5, 14, 15). “The potential benefits of mandatory mass quarantine need to be weighed carefully against the possible psychological costs as studies inform different mental health conditions that may appear when an individual is quarantined or isolated” (5).
Even though the WHO has strategically announced relevant policies and principles, the COVID-19 pandemic has caused a grave challenge on mental health services particularly among suspected and confirmed cases and frontline health care workers. They may develop a fear of contagion, which as a result, may lead to suicidal behaviors, sleep disturbances, and stress-related disorders. Further, firm quarantine and mandatory contact tracing policies by health authorities could cause societal rejection, discrimination, and stigmatization (5).
Previous studies conducted worldwide about the impact of COVID-19 on mental health show that symptoms of depression, anxiety, and unexplained somatic symptoms are common emotional and psychological responses to the pandemic (16, 17). The communities were concerned about social isolation accompanied by quarantine during the pandemic (18). According to a study done in China, which determines the impact of the COVID-19 pandemic, the majority of the study respondents reported a different level of symptoms of common mental disorders. In this study, about 16% of the participants reported different levels of depression, 35% reported different symptoms of anxiety, and 8% reported moderate-to-severe distress (19).
Developing countries traditionally have a higher prevalence of mental disorders (20, 21). Therefore, it is reasonable to assume that, in the pandemic, this situation worsened. Although the tremendous psychological impact of the pandemic is widely discussed, a burden of the psychological impact of this pandemic on the peoples in quarantine and isolation centers is not yet well studied in developing countries, including Ethiopia. It is very significant to study the mental health status of the people in quarantine to develop and implement effective interventions to mitigate the impact of psychological disorders in this grave pandemic era. Therefore, this study was intended to assess the psychological burden of COVID-19 on the people in quarantine and isolation centers and to identify associated factors for early and effective psychosocial intervention during the pandemic and beyond.
Hypothesis
Ho1: There is no psychological impact of COVID-19 among suspected cases in quarantine and isolation centers.
Ho2: All suspected cases of COVID-19 with different characteristics are equally experiencing psychological illnesses.
Materials and Methods
Study Period, Area, and Design
A cross-sectional study was done in Harari and Oromia Regional state, which is found in Eastern Ethiopia, from November 15 to December 31, 2020. During this period, the pandemic was highly contagious, the numbers of cases were dramatically increased in Ethiopia, and this would cause a greater mental disorder.
Harari Regional state is divided into six urban and three rural districts. According to the 2007 national population census, the total population of the region was 183,344, of which 99,321 (54.2 %) were urban and 84,023 (45.8 %) were rural residents. There are two public and one police hospital in region. The East Hararghe zone of Oromia regional state is one of the most populous zones of the region with more than 2.7 million people. It is divided into 18 districts and has three public hospitals (22).
Characteristics of Participants
All suspected cases of COVID-19 in people aged 18 years and above and who were in quarantine and isolation centers at Harari regional state and East Hararghe Zones, Eastern Ethiopia, during the data collection period were included in the study. Suspected cases of people with COVID-19 who cannot communicate due to severe health conditions were excluded from the study.
Sampling Technique
A convenience sampling method was applied to select the respondents. A total of 392 suspected cases who were identified by the rapid response team of the Harari regional state health bureau and eastern Hararghe zonal health department and available in quarantine and isolation centers during the study period were interviewed face to face (direct contacts), considering all the necessary precautions recommended by WHO that were kept to prevent the transmission of COVID-19.
Data Collection Instruments
The common mental disorder was assessed by using the Self-Reporting Questionnaire (SRQ-20). It contains 20 “yes” or “no” questions that assess the symptoms of depression, anxiety, and unexplained somatic complaints in the previous 30 days (23). The SRQ-20 has been tested in various settings with different cutoff points. The SRQ-20 was validated in Ethiopia at a general population, and a cutoff point of six was found to have a sensitivity of 90.7% and specificity of 80.7% (24). For this study, the cutoff point six was considered as the presence of common mental disorders, and the reliability in this study was kappa value of 0.89. People scoring above six were linked and underwent a full clinical psychiatric examination by licensed psychiatrists.
Semistructured questionnaires were applied to review the demographic, clinical, and COVID-19-related descriptions of the participants. Sociodemographic and economic characteristics include age, sex, educational status, religion, occupation, marital status, and residence. Clinical variables include previous history of mental illness and known preexisting chronic medical illness.
COVID-19 control measures, knowledge about COVID-19, time spent focusing on COVID-19 information, presence of adequate personal protective equipment, any symptoms of COVID-19, and perceived severity of COVID-19 were included in the study as COVID-19-related characteristics. Participants' knowledge of COVID-19 was assessed based on responses to the following COVID-19-related single-topic questions: 1) “What kind of information have you received about COVID 19?” with possible response options being how to protect yourself from the disease, symptoms of COVID-19, how it is transmitted, what to do if they have the symptoms, and risks and complications of illness; 2) “what are the major symptoms of COVID 19?” with possible response options being cough, shortness of breath, sore throat, runny or stuffy nose, muscle or body aches, headaches, fatigue (tiredness), diarrhea, and loss of taste and smell; and 3) “how do you rate your level of knowledge on how to prevent the spread of COVID-19 (face mask, hand washing/sanitizing, physical distancing or other)?” with possible response options being little, very poor, poor, good, and very good.
Substance use behavior of the participants was assessed by the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). It is a brief, standardized WHO screening questionnaire to find out about participant's use of psychoactive substances with a sensitivity and specificity of 97 and 90%, respectively. It comprises eight questions or items, covering 10 substances: tobacco, alcohol, cannabis, cocaine, amphetamine-type stimulants (ATS), inhalants, sedatives, hallucinogens, opioids, and “other” drugs. For the purpose of this study, Khat was included under the stimulant category. The ASSIST also investigates frequency of use and associated problems for each substance (25).
Social support of the study participants was assessed by the Oslo 3-item Social Support Scale (OSSS-3). It is a brief and economic instrument for the assessment of the level of social support (26). In a Nigerian population, the internal consistency of the OSSS-3 was accepted with a Cronbach's alpha coefficient of 0.50 and the concurrent validity of OSSS-3 with the depression subscale of the Hospital Anxiety Depression Scale (HADS) was low but significant and inversely related. The discriminate validity was good and was shown by the significant difference between mean OSS-3 of HADS-depression subscale cases compared with non-cases (t-test = 6.710; p ≤ 0.0001; r = −0.3; p = 0.011) (27).
The OSSS-3 contains three items assessing the number of close confidantes, perceived level of concern from others, and perceived ease of getting help from neighbors. The OSSS-3 sum score can be operationalized into three broad categories of social support; 3–8 poor social support, 9–11 moderate social support, and 12–14 strong social support (28).
Data Collection Procedures
Data were collected from suspected COVID-19 individuals using face-to-face interviews by 25 trained health professionals (nurses) working under the districts' (woredas') rapid response team of the Harari region health bureau region and eastern Hararghe zonal health department. Four supervisors were monitoring the data collection process at each site. During the data collection period, all the necessary precautions recommended by WHO were kept to prevent the transmission of COVID-19.
Statistical Analysis
EpiData (version 3.1, EpiData Association, Odense, Denmark) was used to enter the cleaned data, and STATA (version 14.0, StataCorp LLC, College Station, Texas, USA) was used for analyzing the data. Categorical variables were described using frequency and percentage, and continuous variables were described using mean and standard deviation (SD). Explanatory factors that have been associated with a common mental disorder were identified by conducting bivariable and multivariable logistic regression, and a p < 0.05 was considered statistically significant. For all of the models, variance inflation factor (VIF) was used to test multicollinearity of independent variables, and the Hosmer and Lemeshow test was done to check model adequacy.
Ethical Consideration
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University, with the approval number of IHRERC/243/2020. The permission letter was submitted to Harari regional state and east Hararghe zone COVID-19 task force office. Before the questionnaire was administered to any eligible participant, informed, voluntary, written and signed consent was obtained from each participant.
Results
Sociodemographic Descriptions of Study Participants
Of 423 suspected cases selected for the study, 392 consented to participate, which yields a response rate of 92.7%. More than half of the respondents, 244 (62.2%) were less than 30 years old with a mean age of 28.9 years (±11.2). A total of 187 (47.7%) participants were females. Orthodox religion followers accounted for 145 (37%), and 172 (43.9%) were Oromo in ethnicity. The majority of the study participants, 204 (52%), were married, and 100 (25.5%) were government employees. Around 115 (29.3%) of the participants were joining the college for the learning, and 346 (88.3%) were living in urban areas as shown in Table 1.

Table 1. Sociodemographic characteristics of suspected cases in quarantine and isolation centers due to COVID-19 in Eastern Ethiopia, 2020.
COVID-19 Related and Clinical Descriptions
Of the respondents, eight (2.0%) had a preexisting mental disorder, and 25 (6.4%) had a chronic medical illness. About 74 (18.9%) of the study participants didn't practice any types of COVID-19 control measures. Of the study participants practicing control measures of COVID-19, hand washing or sanitizing 260 (66.3%) were the most common followed by proper use of face masks 159 (40.7%). About 101 (25.8%) of the participants have no adequate accessibility to personal protective equipment (26), and 205 (52.3%) were seeking information about COVID-19 two times daily. Regarding the knowledge of COVID-19, 227 (57.9%) of them received information on how to protect themselves from the disease, whereas 193 (49.2%) of them received information on how it is transmitted. The majority, 262 (66.8%), of the participants perceived that they have good knowledge about the COVID-19 pandemic (Table 2).
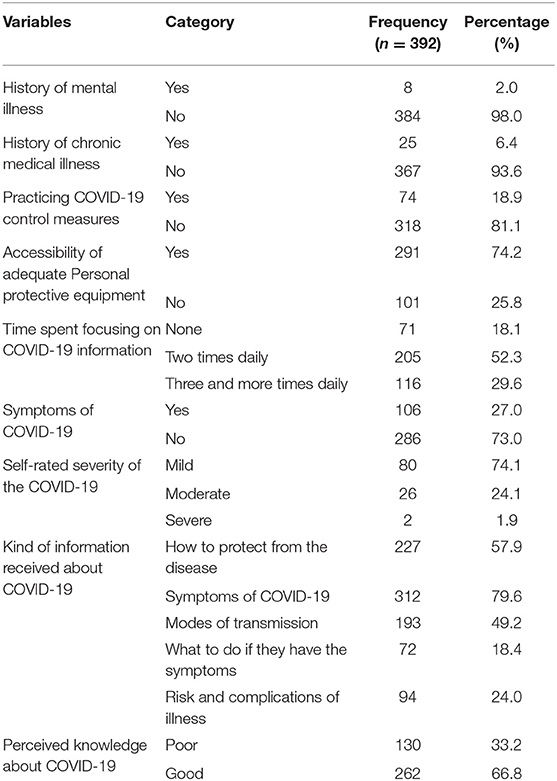
Table 2. Clinical and COVID-19 related characteristics of suspected cases in quarantine and isolation centers due to COVID-19 in Eastern Ethiopia, 2020.
About 106 (27%) of the study participants had symptoms of COVID-19 pandemic, and of this, cough 67 (63.2%) is the most prevalent symptom; 80 (74.1%) of them rated their symptoms as mild (Figure 1).
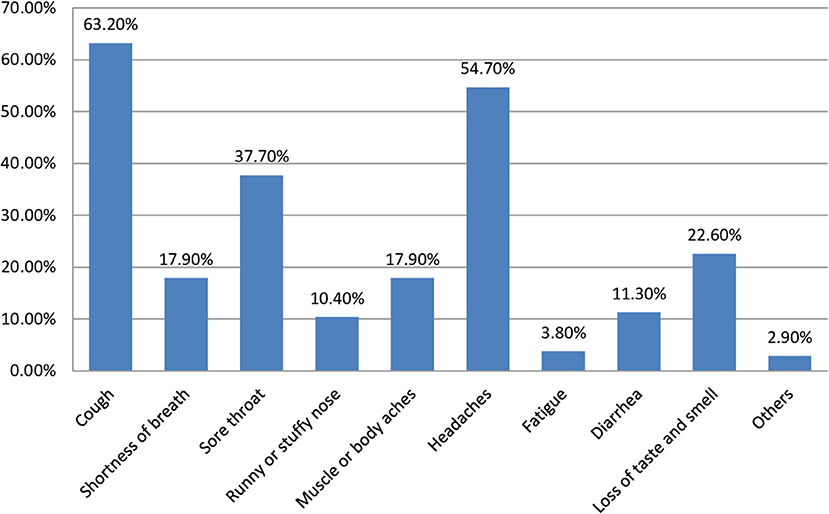
Figure 1. Description of signs and symptoms manifested by the suspected cases in quarantine and isolation centers due to COVID-19 in Eastern Ethiopia, 2020.
Substance Use Behavior and Psychosocial Related Characteristics of the Participants
The substance use behavior of the participants was assessed using ASSIST. Accordingly, 91 (23.2%) were using a substance at least once throughout their lifetime, and 89 (22.7%) were using at least one type of substance within the last 3 months as shown in Figure 2. Regarding receiving the support, 165 (42.1%) of the study participants had good social support, and 57 (14.5%) had poor social support.
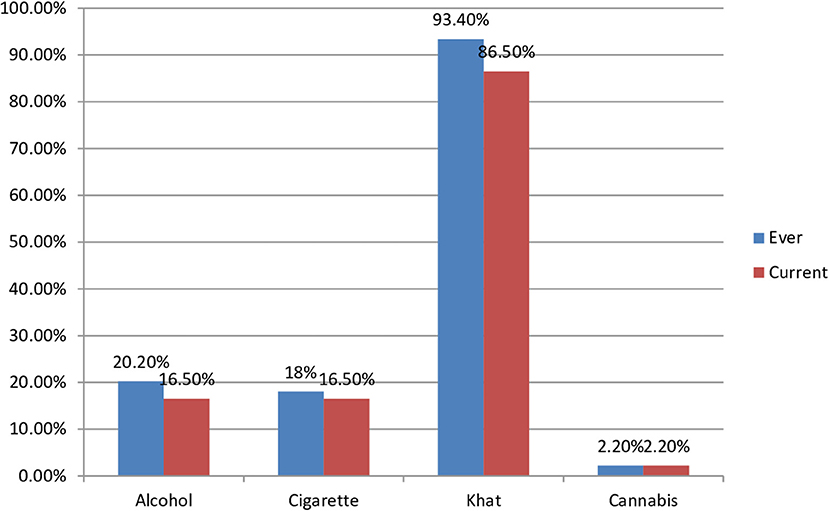
Figure 2. Description of types of substance used by he suspected cases in quarantine and isolation centers due to COVID-19 in Eastern Ethiopia, 2020.
Prevalence of the Common Mental Disorder
The overall prevalence of a common mental disorder among suspected cases in quarantine and isolation centers due to COVID-19 was found to be 13.5% [95% CI: 10.2, 17.1%]. Concerning the distribution of the symptoms, headache (n = 66) was the symptom experienced most frequently, followed by having a poor appetite (n = 48). The mean of SRQ-20 score was 3 (SD = 1).
Factors Associated With a Common Mental Disorder
In the bivariable logistic regression model: age, sex, marital status, educational status, residence, chronic medical illness, presence of adequate personal protective equipment, perceived knowledge about COVID-19, presence of any symptoms of COVID-19, and current use of any substance were associated with a common mental disorder and considered for multivariable analysis.
The final multivariable logistic regression model revealed the following: Female sex (AOR = 1.52, 95% CI: 1.1, 2.92), known chronic medical illness (AOR = 7.0, 95% CI: 2.2, 21.8), inadequate accessibility of personal protective equipment (AOR = 6.1, 95% CI: 2.8, 13.3), poor awareness concerning the pandemic (AOR = 2.90, 95% CI: 2.71, 7.54), presence of symptoms of the disease (AOR = 5.3, 95% CI: 2.57, 11.1), and substance use (AOR = 2.7, 95% CI: 1.2, 6.1) were found to be associated with a common mental disorder (Table 3).
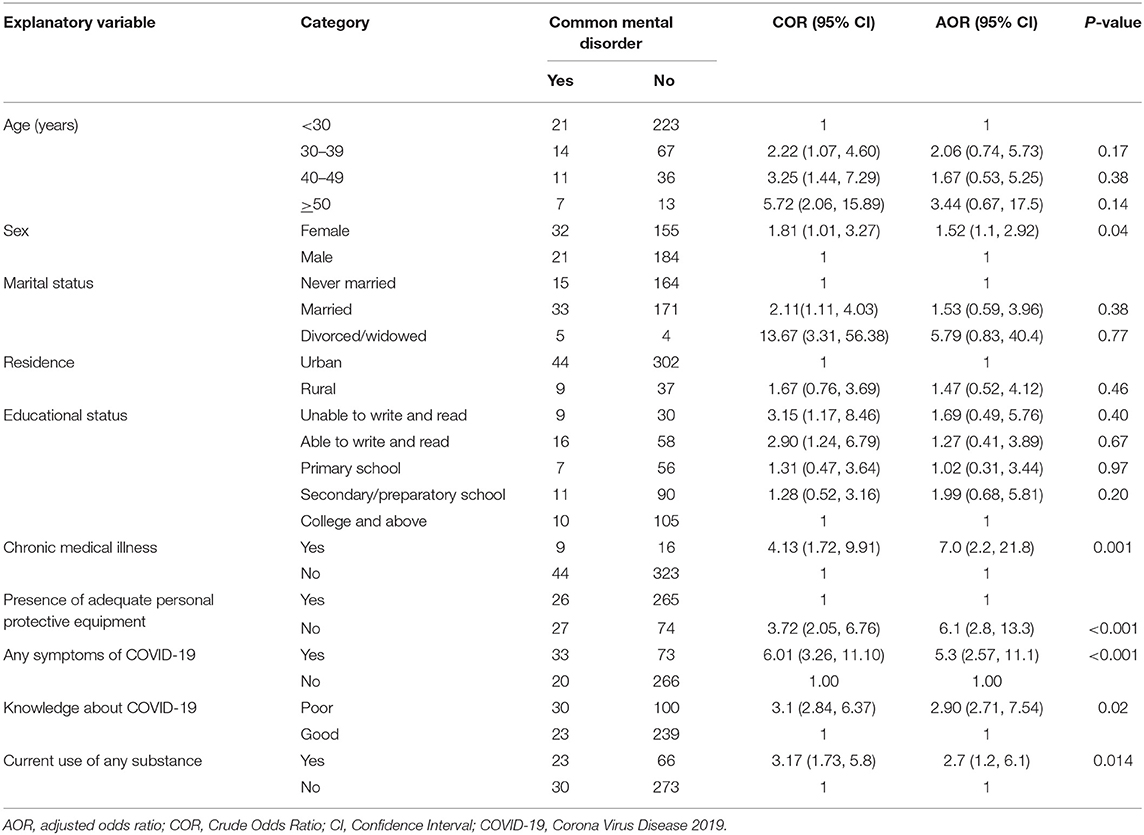
Table 3. Factors associated with common mental disorder among suspected cases in quarantine and isolation centers due to COVID-19 in Eastern Ethiopia, 2020.
Discussion
The present study utilizing a sample of 392 Ethiopian adults found that the common mental disorder was 13.5% in suspected cases of COVID-19 who were self-isolating and in a quarantine center due to the COVID-19 pandemic. The finding was comparable with studies done in China 11.9% (29), but it was lower as compared with the studies done in the United States 69% (30), China 36.05% (31), and Canada, which revealed the prevalence of depression and anxiety as 31.2 and 28.9%, respectively (14, 32). The possible explanation for this difference might be due to the government introducing the rapid response team to prevent and control the disease, which includes a psychological first aid team. Besides this, this study was conducted in December 2020 when the incidence of the cases decreased, indicating the quick transmission of the virus had been controlled, which alleviated psychological distress and symptoms of common mental disorder symptoms. On the other hand, the result was higher than the study conducted in another part of China at 9.0% (33). This discrepancy might be due to the variation in demographic characteristics, sampling size, and data collection instrument used to measure the dependent variable.
After adjusting for the potential confounder, being female, having known chronic medical illness, having inadequate accessibility of personal protective equipment, having poor knowledge about the COVID-19 pandemic, complaining of any symptoms of COVID-19, and currently using any type of substances were associated with a common mental disorder.
In this study, female sex was significantly associated with the common mental disorder. This result was consistent with studies conducted in Spain (34), the United Kingdom (35), and China (31). The possible explanation for this might be due to the affective nature of a female's response to stressful life events and hormonal changes. Second, during the virus pandemic, different studies reported the increments in domestic violence, and home quarantine may exacerbate gender-based violence (36).
Suspected cases of COVID-19 who had any type of chronic disease were seven times more likely to have a common mental disorder. This result agrees with a study done in the United Kingdom (37). In this situation, patients with chronic illnesses, cardiovascular diseases, cancer, diabetes, hypertension, stroke, cognitive disorders, and psychotic disorders experience emotional disturbance, nervousness, rage, perplexity, and stigma (5, 38) due to unexpected separation from loved ones, scarcity of essentials, the loss of freedom, and uncertainty over disease status. In addition, some patients have been confronted with difficulties in regular medical supplies due to delayed transportation and scarcity of medicines and human power in health facilities (39). Moreover, in this pandemic, the death rate in aged patients with chronic illness is the highest. Some older patients dared not go to the hospital. All these circumstances raise the possibility of relapse or even death.
According to this study, inadequate accessibility of personal protective equipment was significantly associated with the common mental disorder. This finding agreed with a study done in the United States (40). “Personal protective equipment is recommended in the care of anyone with suspected COVID-19 by multiple health organizations including the World Health Organization and the Centers for Disease Control and Prevention, forcing physicians to choose between protecting themselves and caring for their patients” (41). This causes specific sources of worry and panic among frontline health care worker that are combating the COVID-19 outbreak.
The other important predictor of a common mental disorder was having the common signs and symptoms of the COVID-19 disease. This result was in accordance with studies done in Spain (34) and Wuhan, China (42). In the current study, people with suspected cases of COVID-19 who had low awareness of the pandemic were 2.4 times more likely to have common mental disorders. The finding was consistent with the study done in Spain (34). The role of information seems to be fundamental and influences the mental health status of the individuals.
It is also worth noting that currently using any type of substance was significantly associated with the development of a common mental disorder (AOR = 2.7, 95% CI: 1.2, 6.1). This result was supported by studies conducted in the United Kingdom (43) and the United States (44). There are several possible explanations for this result. Existing literature shows that exposure to a traumatic event is particularly linked to starting substance use and that using the substance in response to stress has been specifically linked to an increased possibility of developing a substance use disorder and other common mental illness (45).
The finding of this study support the notion that public mental health interventions should be formally integrated into public health preparedness and emergency response plans. Mental health-care organizations and public health institutions are releasing practical guidelines on taking care of mental health and well-being (46, 47). The American Psychiatric Association (APA), the National Alliance on Mental Illness (NAMI), and the Substance Abuse and Mental Health Services Administration (SAMHSA) provide general tips for the community on how to organize their own time and manage their physical and mental health. The Centers for Disease Control and Prevention and the WHO supply further information specific for high-risk groups (48, 49).
Limitation of the Study
The study has some limitations. Considering the limited availability of resources and the urgent or alarming effect of the COVID-19 pandemic outbreak, we implemented the convenience sampling technique. This sampling strategy was not based on a random selection of the sample, and the study population did not reveal the actual pattern of the general population.
Conclusion
The current study revealed that having a common mental disorder was relatively high among suspected cases of COVID-19 as compared with the general populations. Being female, having known chronic medical illness, inadequate accessibility of personal protective equipment, having poor knowledge about the COVID-19 pandemic, complaining of any symptoms of COVID-19, and currently using any type of substance was associated with a common mental disorder. Therefore, providing appropriate psychosocial intervention for the populations at risk is important to decrease the effect of common mental disorders among suspected cases of COVID-19.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors were contributed to the inception of the study, organized the data collection process, equally contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was financially supported by Haramaya University (Grant No. HUCF-2020-02-NA-06).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful to Haramaya University for sponsoring this study. Our appreciation also goes to the East Hararghe and Harari region COVID-19 task force. Finally, we have great thanks to the study participants.
Abbreviations
AOR, adjusted odds ratio; ASSIST, Alcohol Smoking and Substance Involvement Screening Test; CI, Confidence Interval; COR, Crude Odds Ratio; COVID-19, Corona Virus Disease 2019; SRQ-20, Self Reporting Questionnaire.
References
1. Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and Antiphospholipid Antibodies in Patients with COVID-19. N Engl J Med. (2020) 17:382. doi: 10.1056/NEJMc2007575
2. World Health Organization. Mental Health and Psychosocial Considerations During the COVID-19 Outbreak. (2020). Available online at: https://apps.who.int/iris/handle/10665/331490 (accessed Nevember 10, 2020).
3. Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M, et al. Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: a case report. Brain Behav Immun. (2020) 87:179–81. doi: 10.1016/j.bbi.2020.05.054
4. Tognotti E. Lessons from the history of quarantine, from plague to influenza A. Emerg Infect Dis. (2013) 19:254–9. doi: 10.3201/eid1902.120312
5. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
6. Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. (2020) 42: e2020038. doi: 10.4178/epih.e2020038
7. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e21. doi: 10.1016/S2215-0366(20)30090-0
8. Marazziti D, Stahl SM. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. (2020) 19:261. doi: 10.1002/wps.20764
9. Unützer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. (2020) 19:130. doi: 10.1002/wps.20766
10. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) 63:e32. doi: 10.1192/j.eurpsy.2020.35
11. Giallonardo V, Sampogna G, Del Vecchio V, Luciano M, Albert U, Carmassi C, et al. The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front Psychiatry. (2020) 11:533. doi: 10.3389/fpsyt.2020.00533
12. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndrome. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
13. Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. (2020) 368:m313. doi: 10.1136/bmj.m313
14. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
15. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can Med Assoc J. (2003) 168:1245–51. doi: 10.168/10/1245.short
16. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732–8. doi: 10.7150/ijbs.45120
17. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. (2020) 74:281–2. doi: 10.1111/pcn.12988
18. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. (2020) 52:102066. doi: 10.1016/j.ajp.2020.102066
19. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
20. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. (2017). Available online at: https://apps.who.int/iris/bitstream/handle/10665/254610/W?sequence=1 (accessed November 17, 2020).
21. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. (2014) 43:476–93. doi: 10.1093/ije/dyu038
22. Central Statistical Agency. Population Housing Census of 2007, Ethiopia. (2008). Available online at: https://catalog.ihsn.org/index.php/catalog/3583 (accessed Nevember 12, 2020).
23. World Health Organization. A User's Guide to the Self Reporting Questionnaire (SRQ). (1994). Available online at: https://apps.who.int/iris/bitstream/handle/10665/61113/?sequence=1 (accessed Nevember 10, 2020).
24. Youngmann R, Zilber N, Workneh F, Giel R. Adapting the SRQ for Ethiopian populations: a culturally-sensitive psychiatric screening instrument. Transcult Psychiatry. (2008) 45:566–89. doi: 10.1177/1363461508100783
25. WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. (2002) 97:1183–94. doi: 10.1046/j.1360-0443.2002.00185.x
26. Kocalevent RD, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. (2018) 6:31. doi: 10.1186/s40359-018-0249-9
27. Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item Oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malaysian J Psychiatry. (2013) 22:32–41. Available online at: http://mjpsychiatry.org/index.php/mjp/article/view/264 (accessed March 20, 2021).
28. Duko B, Ayano G, Bedaso A. Depression among pregnant women and associated factors in Hawassa city, Ethiopia: an institution-based cross-sectional study. Reprod Health. (2019) 16:25. doi: 10.1186/s12978-019-0685-x
29. Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monitor. (2020) 26:e924609–1. doi: 10.12659/MSM.924609
30. Rosen Z, Weinberger-Litman SL, Rosenzweig C, Rosmarin DH, Muennig P, Carmody ER, et al. Anxiety and distress among the first community quarantined in the US due to COVID-19: psychological implications for the unfolding crisis. PsyArXiv Preprints. (2020). doi: 10.31234/osf.io/7eq8c
31. Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. (2020) 36:164–78. doi: 10.1080/08870446.2020.1782410
32. Lancee WJ, Maunder RG, Goldbloom DS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Services. (2008) 59:91–5. doi: 10.1176/ps.2008.59.1.91
33. Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. (2020) 274:1–7. doi: 10.1016/j.jad.2020.05.009
34. González-Sanguino C, Ausín B, ÁngelCastellanos M, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immunity. (2020) 1828:1715–22. doi: 10.1016/j.bbi.2020.05.040
35. Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom: results from the understanding society UKHLS. medRxiv. (2020) 291:113267. doi: 10.1016/j.psychres.2020.113267
36. Aolymat I. A cross-sectional study of the impact of covid-19 on domestic violence, menstruation, genital tract health, and contraception use among women in jordan. Am J Trop Med Hyg. (2020) 104:519–25. doi: 10.4269/ajtmh.20-1269
37. Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. (2020) 6:e125. doi: 10.1192/bjo.2020.109
38. Hajure M, Tariku M, Mohammedhussein M, Dule A. Depression, anxiety and associated factors among chronic medical patients amid COVID-19 pandemic in mettu karl referral hospital, Mettu, Ethiopia, 2020. Neuropsychiatr Dis Treat. (2020) 16:2511–8. doi: 10.2147/NDT.S281995
39. Pellino G, Spinelli A. How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in italy: a long shadow beyond infection. Dis Colon Rectum. (2020) 63:720–2. doi: 10.1097/DCR.0000000000001685
40. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
41. Chirico F, Nucera G, Magnavita N. covid-19: protecting-healthcare-workers-is-a-priority. Infect Control Hosp Epidemiol. (2020) 41:1117. doi: 10.1017/ice.2020.148
42. Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. (2020) 292:113297. doi: 10.1016/j.psychres.2020.113297
43. Smith L, Jacob L, Yakkundi A, McDermott D, Armstrong NC, Barnett Y, et al. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatry Res. (2020) 291:113138. doi: 10.1016/j.psychres.2020.113138
44. Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res. (2020) 293:113407. doi: 10.1016/j.psychres.2020.113407
45. Hyman SM, Sinha R. Stress-related factors in cannabis use and misuse: implications for prevention and treatment. J Subst Abuse Treat. (2009) 36:400–13. doi: 10.1016/j.jsat.2008.08.005
46. Kuzman MR, Curkovic M, Wasserman D. Principles of mental health care during the COVID-19 pandemic. Eur Psychiatry. (2020) 63:e45. doi: 10.1192/j.eurpsy.2020.54
47. McDaid D. Investing in strategies to support mental health recovery from the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e32. doi: 10.1192/j.eurpsy.2021.28
48. Centers for Disease Control Prevention. COVID-19 Overview and Infection Prevention and Control Priorities in non-US Healthcare Settings. (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html (accessed March 20, 2021).
49. World Health Organization. Coronavirus Disease (COVID-19) Outbreak: Rights, Roles and Responsibilities of Health Workers, Including Key Considerations for Occupational Safety and Health. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-covid-19.pdf?sfvrsn=bcabd401_0 (accessed January 18, 2021).
Keywords: suspected cases, quarantine, isolation, common mental disorder, COVID-19, Ethiopia
Citation: Misgana T, Tesfaye D, Tariku M, Ali T, Alemu D and Dessie Y (2022) Psychological Burden and Associated Factors of the COVID-19 Pandemic on People in Quarantine and Isolation Centers in Ethiopia: A Cross-Sectional Study. Front. Psychiatry 12:753383. doi: 10.3389/fpsyt.2021.753383
Received: 04 August 2021; Accepted: 29 November 2021;
Published: 12 January 2022.
Edited by:
Gábor Gazdag, Jahn Ferenc Dél-Pesti Kórház és Rendelőintézet, HungaryReviewed by:
Claudio Andre Barbosa De Lira, Universidade Federal de Goiás, BrazilGaia Sampogna, University of Campania “L. Vanvitelli”, Italy
Copyright © 2022 Misgana, Tesfaye, Tariku, Ali, Alemu and Dessie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tadesse Misgana, tadessemisgana25@gmail.com
 Tadesse Misgana
Tadesse Misgana Dejene Tesfaye
Dejene Tesfaye Mandaras Tariku
Mandaras Tariku Tilahun Ali
Tilahun Ali Daniel Alemu
Daniel Alemu Yadeta Dessie
Yadeta Dessie