Abstract
Purpose
We assessed the impact of COVID-19 infection on cardiovascular events in patients with suspected or known coronary artery disease (CAD) referred to stress single-photon emission computed tomography myocardial perfusion imaging (MPS).
Methods
A total of 960 consecutive patients with suspected or known CAD were submitted by referring physicians to stress MPS for assessment of myocardial ischemia between January 2018 and June 2019. All patients underwent stress-optional rest MPS. Perfusion defects were quantitated as % of LV myocardium and expressed as total perfusion defect (TPD), representing the defect extent and severity. A TPD ≥ 5% was considered abnormal.
Results
During a mean follow-up of 27 months (range 4–38) 31 events occurred. Moreover, 55 (6%) patients had a COVID-19 infection. The median time from index MPS to COVID-19 infection was 16 months (range 6–24). At Cox multivariable analysis, abnormal MPS and COVID-19 infection resulted as independent predictors of events. There were no significant differences in annualized event rate in COVID-19 patients with or without abnormal MPS (p = 0.56). Differently, in patients without COVID-19, the presence of abnormal MPS was associated with higher event rate (p < .001). Patients with infection compared to those without had a higher event rate in the presence of both normal and abnormal TPD.
Conclusion
In patients with suspected or known CAD, the presence of COVID-19 infection during a short-term follow-up was associated with a higher rate of cardiovascular events.
Similar content being viewed by others
Introduction
The recent outbreak of Coronavirus disease 2019 (COVID-19) has been rapidly spreading on a global scale [1], and it has resulted in considerable morbidity and mortality worldwide. COVID-19 is accompanied by a cluster of flu-like symptoms and life-threatening severe illnesses including acute respiratory distress syndrome, acute kidney injury, myocarditis, and organ failure [2]. Cardiovascular symptoms occur frequently in COVID-19 patients and the infection is associated with a high incidence of cardiac injury, heart failure, circulatory shock, and arrhythmias [3]. Myocardial damage associated to COVID-19 infection is likely consequent to a cytokine storm and can be responsible for respiratory dysfunction, hypoxemia, hypotension, and shock [4, 5]. Increasing attention is currently being paid to evaluate the relationships between COVID-19 infection and the cardiovascular system. The incidence of COVID-19 infection in patients with cardiovascular diseases (CVD) is difficult to estimate due to varying degrees of national surveillance and data collection around the world [6]. In about 12% of COVID-19 patients, the infection was associated with acute heart injures [7]. Moreover, approximately 5–25% of hospitalized COVID-19 cases had elevations in cardiac troponin, a biomarker of myocardial injury [8]. Patients with acute myocardial injury are older, with a higher prevalence of concomitant CVD and more likely need intensive care treatment [9]. Patients with coronary artery disease (CAD) and COVID-19 have higher rates of comorbidities, inpatient mortality, and need for renal replacement therapy compared to their non-CAD counterparts. In a meta-analysis involving 13 studies in patients with COVID-19, cardiac injury was associated with mortality, need for intensive care, and severity of disease [10]. However, in a further study, after adjusting for other covariates, CAD was not associated with mortality, suggesting that other factors may play a predominant role in the increased mortality and poor outcomes in these patients [11]. Even less clear is the effect of COVID-19 infection on the progression and outcome of CVD. Hence, it could be interesting to investigate the relationships between CAD, COVID-19 infection, and outcome. The aim of this retrospective study was to evaluate the impact of COVID-19 infection on cardiovascular events in patients with suspected or known CAD referred to stress single-photon emission computed tomography myocardial perfusion imaging (MPS).
Methods
Patients
A total of 960 consecutive patients with suspected or known CAD were submitted by referring physicians to stress MPS for assessment of myocardial ischemia between January 2018 and June 2019. Ten patients who underwent early (< 90 days after MPS) coronary revascularization procedures were excluded. Patients’ clinical history was collected, and cardiac risk factors were assessed before testing. A patient was considered to have known CAD at the time of the MPS based on a provided history of previously diagnosed atherosclerotic coronary disease, history of myocardial infarction (chest pain or equivalent symptom complex, positive cardiac biomarkers, or typical electrocardiographic changes), history of percutaneous coronary intervention, or history of coronary artery bypass grafting. Among patients with suspected CAD (n = 535), 466 (87%) were referred to MPS for assessment of myocardial ischemia in the presence of cardiovascular risk factors and/or chest pain symptoms and 69 (13%) for pre-surgery evaluation. All patients with known CAD (n = 415) were referred to MPS for evaluation of myocardial ischemia. The Ethics Committee of our institution approved the study, and all patients gave informed consent (Protocol Number 110/17).
Study protocol
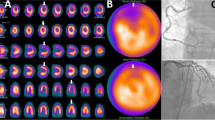
All patients underwent stress-optional rest MPS by CZT-SPECT systems (D-SPECT, Spectrum Dynamics, Caesarea, Israel) by 99mTc sestamibi physical exercise or dipyridamole stress test, according to the recommendations of the European Association of Nuclear Medicine [12, 13]. In all patients, beta-blocking medications and calcium antagonists were withheld for 48 h and long-acting nitrates for 12 h before testing. All patients were also instructed to fasting for 4 h before the stress test. For patients undergoing exercise test, symptom-limited treadmill standardized protocols were performed, with monitoring of heart rate and rhythm, blood pressure, and ECG. Test endpoints were achievement of 85% maximal predicted heart rate, horizontal or down-sloping ST-segment depression > 2 mm, ST-segment elevation > 1 mm, moderate to severe angina, systolic blood pressure decrease > 20 mm Hg, blood pressure > 230/120 mmHg, dizziness, or clinically important cardiac arrhythmia. Patients undergoing dipyridamole stress test were instructed not to consume products containing caffeine for 24 h before the test. Dipyridamole was infused at dose of 0.142 mg/kg per min intravenous over 4 min. A dose of 100 mg of aminophylline was administered intravenously at the end of the stress test in the event of chest pain or other symptoms, or after significant ST depression. No patient showed symptoms that required discontinuation of the stress test. At peak exercise, or 4 min after completion of dipyridamole infusion, a bolus of 370 MBq of 99mTc-sestamibi was injected intravenously. For both types of stress, heart rate and blood pressure data were recorded at rest, at the end of each stress stage, at peak stress, and in the delay phases at rest. The 12-lead ECG was continuously monitored and recorded during the stress test. Maximal degree of ST-segment changes at 80 ms after the J-point of the ECG was measured and assessed as horizontal, down-sloping, or up-sloping. Horizontal or down-sloping ST-segment depression ≥ 0.1 mV, persisting for at least 0.06 to 0.08 s after the J-point in one or more ECG lead, were considered diagnostic for ischemia, whereas up-sloping ST depressions ≥ 1.0 mm were considered nondiagnostic. All ST depression < 1.0 mm additional from baseline was defined as negative. Recordings were obtained using 9 pixilated CZT crystal detector columns mounted vertically spanning a 90° geometry. Each of the columns consists of 1024 (16 × 9 × 64) 5-mm thick CZT crystal elements (2.46 × 9 × 2.46 mm). Square hole tungsten collimators are fitted to each of the detectors, which are shorter than conventional low-energy, high-resolution collimators, yielding significantly better geometric speed [14]. Data were acquired focusing on the heart by the detectors rotating in synchrony and saved in list mode. Images were obtained with the patient in a semi recumbent position. A 10-s pre-scan acquisition was performed to identify the location of the heart and to set the angle limits of scanning for each detector (region of interest-centric scanning). Using the myocardial count rate from the pre-scan acquisition, the time per projection was set to target the recording of 1000 myocardial kcounts; the duration of the scans was less than 10 min for stress and 4 min for rest. Summed and gated projections were reconstructed with an iterative maximum likelihood expectation maximization algorithm using 7 and 4 iterations, respectively [15]. An automated software program (e-soft 2.5, QGS/QPS, Cedars-Sinai Medical Center, Los Angeles, CA) was used to calculate left ventricular (LV) volumes, ejection fraction, wall motion, wall thickening, and the scores incorporating both the extent and severity of perfusion defects, using standardized segmentation of 17 myocardial regions [16, 17]. Perfusion defects were quantitated as % of LV myocardium and expressed as total perfusion defect (TPD), ischemia (reversible perfusion defect), and scar (fixed perfusion defect). A TPD ≥ 5% and a post-stress LV ejection fraction < 45% were considered abnormal [18,19,20].
Outcome
Patient follow-up was obtained by use of a questionnaire that was assessed by a phone call to the patients, general practitioners, or cardiologists, and by review of hospital or physicians’ records by individuals blinded to the patient’s test results. The follow-up questionary included all possible data linked to COVID-19 infection: time and duration of the infection, symptoms, hospitalization, and related course. Moreover, outcome was composite end-point of cardiac death, nonfatal myocardial infarction, or coronary revascularization, whichever occurred first. The cause of death was confirmed by review of death certificate, hospital chart, or physician’s records. Death was of cardiac origin if the primary cause was defined as acute myocardial infarction, congestive heart failure, valvular heart disease, sudden cardiac death, or cardiac interventional/surgical procedure related. The diagnosis of myocardial infarction was made by the treating team of healthcare providers [21]. No patient experienced events from MPS to COVID-19 infection. The date of the last examination or consultation was used to determine the length of follow-up.
Statistical analysis
Continuous data are expressed as mean ± standard deviation and categorical data as percentage. A student two-sample t-test and chi-square test were used to compare the differences in continuous and categorical variables, respectively. A p < 0.05 (two-sided) was considered statistically significant. Annualized event rates (AER), expressed as % person-years, were calculated as the cumulative number of events divided by person-time. This latter is an estimate of the actual time-at-risk that all persons contribute to the study, i.e., the sum of each individual follow-up period. Because patients shifted from the no COVID-19 to the COVID-19 group during follow-up, unadjusted event-free survival functions were estimated using the method proposed by Simon-Makuch [22], a modification of Kaplan–Meier analysis, and compared using the Mantel-Byar test [23]. In this context, COVID-19 is treated as a binary nonreversible time-dependent covariate that starts at 0 (no COVID-19) and may switch to 1 (COVID-19) at some time point. Thus, the study cohorts are continually updated as follows: for the time prior to COVID-19 infection, the patient contributes to the no COVID-19 cohort, but for the time after COVID-19 infection, the patient contributes to the COVID-19 cohort. The start time (t0) for the no COVID-19 group is the beginning of follow-up (index MPS), while for the COVID group t0 is the date of COVID-19 infection after index MPS. The impact of COVID on event-free survival was evaluated with the extended Cox regression model. To consider differences in the time from index MPS to COVID-19, COVID-19 was treated as a binary nonreversible time-dependent covariate. Thus, COVID-19 patients were members of the no COVID-19 group until the day of infection. At that point, they were crossed over to the COVID-19 group. This means that patients contribute to the hazard estimate of the no COVID-19 group up to the infection time, when they start to contribute to the hazard estimate of the COVID-19 group. Statistical analysis was performed with Stata 16 software (StataCorp, College Station, Texas USA).
Results
Patient characteristics and outcome
Follow-up data were not available in 73 (8%) of the 950 patients, leaving 877 subjects for the analysis. Clinical characteristics and imaging findings in patients with suspected or known CAD are illustrated in Table 1. Coronary angiographic data were available in 20 patients with suspected CAD and in 349 patients with known CAD. A significant coronary artery stenosis (≥ 50%) was present in 51 of the patients with known CAD.
Over a median follow-up of 27 months (range 4–38), 31 cardiac events occurred (3.5% cumulative event rate) and 6 patients died of COVID-19 infection. Cardiac events were cardiac death in 9 (29%), nonfatal myocardial infarction in 5 (16%), and revascularization procedures in 17 (55%) patients. Patient’s characteristics and imaging findings according to the occurrence of cardiac events are reported in Table 2. All patients with abnormal MPS and known CAD were referred to optimized medication. During the follow-up, 55 (6%) patients presented a COVID-19 infection and 822 (94%) did not. The median time from index MPS to COVID-19 infection was 16 months (range 6–24). Clinical characteristics and imaging findings according to the occurrence of COVID-19 infection are described in Table 3. As shown, patients with COVID-19 had lower mean age and a higher prevalence of angina symptoms as compared to patients without COVID-19. All the others clinical characteristics were comparable between the two groups. Moreover, the prevalence of abnormal MPS was similar in patients with and without COVID-19. The cumulative event rate was 14% in patients with COVID-19 and 2.8% in those without (p < 0.001).
Predictors of events
The results of Cox univariable and multivariable analysis for prediction of cardiac events are reported in Table 4. At multivariable analysis, only abnormal MPS and COVID-19 infection were significant predictors of events. Event-free survival was better in patients without than in those with COVID-19 (p < 0.001) (Fig. 1). The AER according to COVID-19 infection and MPS are depicted in Fig. 2. Patients with infection compared to those without had a higher event rate in the presence of both normal and abnormal TPD.
Simon and Makuch’s modified Kaplan–Meier curves in patients with (red line) and without (blue line) COVID-19 infection (time-dependent covariate). COVID − , patients without infection; COVID + , patients with infection; MPS − , patients with normal MPS (TPD < 5%); MPS + , patients with abnormal MPS (TPD ≥ 5%)
There were no significant differences in AER in COVID-19 patients with or without abnormal MPS (p = 0.56). On the contrary, in patients without COVID-19, the presence of abnormal MPS was associated with a higher event rate (p < 0.001). The event-free survival curves according to COVID-19 and MPS results are reported in Fig. 3. Patients with COVID-19 and abnormal MPS had the worst outcome with a lower event-free survival as compared to patients without COVID-19 with both normal and abnormal MPS (p < 0.001). Yet, the event-free survival was similar in patients with COVID-19 and normal MPS and those with COVID-19 and abnormal MPS (p = 0.48). There was no difference in event-free survival between patients without COVID 19 and with abnormal MPS and patients with COVID-19 but normal MPS. The best outcome was observed in no COVID-19 patients and normal MPS.
Simon and Makuch’s modified Kaplan–Meier curves in patients without COVID-19 and normal MPS (blue line), without COVID-19 and abnormal MPS (red line), with COVID-19 and normal MPS (green line) and with COVID-19 and abnormal MPS (yellow line). COVID − , patients without infection; COVID + , patients with infection; MPS − , patients with normal MPS (TPD < 5%); MPS + , patients with abnormal MPS (TPD ≥ 5%)
Discussion
The present study demonstrated that patients referred to stress MPS for evaluation of suspected or known CAD, who presented COVID-19 infection during follow-up had a higher incidence of cardiac events compared to patients without subsequent COVID-19 infection. In particular, COVID-19 infection and abnormal MPS were both independent predictors of cardiac events at follow-up.
After its onset, COVID-19 infection has spread to over 22 countries globally, and mortality in patients with severe disease has been reported to be almost 50% [24]. Previous studies demonstrated that patients with COVID-19 infection and other comorbidities were more frequently affected by a severe COVID-19 disease with a higher rate of mortality [25]. Therefore, increasing attention is being directed to analyze the impact of underlying diseases on the prognosis of COVID-19 [26,27,28]. Cardiac disease represents the most common comorbidity in patients with COVID-19 and the presence of CVD is a relevant risk factor for rapid progression and poor prognosis in these patients [29].
In a retrospective study of 138 patients from the University of Wuhan, patients with severe disease who needed intensive care treatment were significantly older and had more frequently underlying comorbidities, such as hypertension, diabetes mellitus, and known CAD [9]. On the other hand, COVID-19 infection may be associated with myocardial injury. Moreover, the mechanisms of myocardial injury involve a direct damage to myocardiocytes, systemic inflammation, myocardial interstitial fibrosis, exaggerated T-cell Helper type 1 and 2 activation, coronary plaque destabilization, and hypoxia [30]. In our study population, in a follow-up of about 2 years, the presence of COVID-19 infection and abnormal MPS was associated with the worst prognosis, while patients with normal MPS and without COVID-19 disease had the best prognosis. Interestingly, there were no significant difference in the composite end-point of cardiac death, nonfatal myocardial infarction, or coronary revascularization between patients with COVID-19 and normal or abnormal MPS. Thus, COVID-19 infection in patients with suspected or known CAD resulted a significant variable in defining the risk of cardiac event. Likely, the presence of COVID-19 and has an important role on the poor outcome, observed, independently of others cardiac risk factors and the presence of abnormal perfusion.
It is well known that coronaviruses are able to bind to some metal peptidases such as ACE2, which is widely expressed on epithelial cells of several compartments, such as pulmonary alveoli and intestinal mucosa, as well as on arterial and venous endothelial cells and smooth muscle cells [31]. The variety of expression of ACE2 suggests the correlation between COVID-19 and extra-pulmonary manifestations, in particular cardiac involvement. Moreover, the virus is able to determine a down regulation of ACE2 pathways at the myocardial level, with consequent myocardial inflammation [32]. It has been demonstrated that patients with comorbidities such as CVD, arterial hypertension, diabetes, and/or chronic obstructive pulmonary disease who contract COVID-19 infection show a poor prognosis with a 10% rate of mortality [33]. Cardiac complications associated with viral pneumonia include malignant arrhythmias, myocardial infarction, and heart failure [33]. Myocardial damage during COVID-19 can be asymptomatic and therefore can only be evaluated with laboratory markers, or it can be clinically evident. A recent meta-analysis reports how the evolution of COVID-19 disease can exacerbate a pre-existing ventricular dysfunction or predispose to a new cardiomyopathy [34]. Therefore, the presence of underlying cardiovascular comorbidities in patients with COVID-19 is associated with high mortality. Our preliminary results involved a limited number of patients in a short-term follow-up. Probably an analysis in a larger study population followed for more time could help to better elucidate the relationship between COVID-19 infection and cardiovascular disease and to evaluate the correlation between infection and poor outcome. Moreover, it has been demonstrated that COVID-19 induced an endothelial cell dysfunction by an excessive generation of thrombin and a shutdown of fibrinolysis, which indicate a state of hyper-coagulability [35]. Therefore, investigations on microvascular and endothelial damage can play a fundamental role in explaining the pathophysiological mechanisms, the clinical course and for the development of new treatments, as well as to reduce the number of those who will need intensive care units.
Conclusions
In our series of patients with suspected or known CAD undergoing to stress MPS, subsequent COVID-19 infection was associated with a significantly higher rate of cardiovascular events during a short-term follow-up, independently of others cardiovascular risk factors. COVID-19 and abnormal MPS were both associated with an increased risk of cardiac events in these patients. Effects of COVID-19 infection on cardiovascular system may have a role in determining a poor outcome in patients with suspected or known CAD.
References
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42.
Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45:100618.
Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14:247–50.
Petrovic V, Radenkovic D, Radenkovic G, Djordjevic V, Banach M. Pathophysiology of cardiovascular complications in COVID-19. Front Physiol. 2020;11:575600.
Song P, Li W, Xie J, Hou Y, You C. Cytokine storm induced by SARS-CoV-2. Clin Chim Acta. 2020;509:280–7. https://doi.org/10.1016/j.cca.2020.06.017.
Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–58.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;39:497–506.
The European Society for Cardiology. ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESCCOVID-19-Guidance. (Last update: 10 June 2020)
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9.
Peterson E, Lo KB, DeJoy R, Salacup G, Pelayo J, Bhargav R, et al. The relationship between coronary artery disease and clinical outcomes in COVID-19: a single-center retrospective analysis. Coron Artery Dis. 2021;32:367–71.
Santoso A, Pranata R, Wibowo A, Al-Farabi MJ, Huang I, Antariksa B. Cardiac injury is associated with mortality and critically ill pneumonia in COVID-19: a meta-analysis. Am J Emerg Med. 2021;44:352–7.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, European Association of Nuclear Medicine (EANM), et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40.
Acampa W, Di Benedetto C, Cuocolo A. An overview of radiotracers in nuclear cardiology. J Nucl Cardiol. 2000;7:701–7.
Esteves FP, Raggi P, Folks RD, Keidar Z, Askew JW, Rispler S, et al. Novel solid-state-detector dedicated cardiac camera for fast myocardial perfusion imaging: multicenter comparison with standard dual detector cameras. J Nucl Cardiol. 2009;16:927–34.
Mannarino T, Assante R, Ricciardi C, Zampella E, Nappi C, Gaudieri V, et al. Head-to-head comparison of diagnostic accuracy of stress-only myocardial perfusion imaging with conventional and cadmium-zinc telluride single-photon emission computed tomography in women with suspected coronary artery disease. J Nucl Cardiol. 2021;28:888–97.
Germano G, Kavanagh PB, Waechter P, Areeda J, Van Kriekinge S, Sharir T, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. I: technical principles and reproducibility. J Nucl Med. 2000;41:712–9.
Nappi C, Gaudieri V, Acampa W, Assante R, Zampella E, Mainolfi CG, et al. Comparison of left ventricular shape by gated SPECT imaging in diabetic and nondiabetic patients with normal myocardial perfusion: a propensity score analysis. J Nucl Cardiol. 2018;25:394–403.
Slomka PJ, Nishina H, Berman DS, Akincioglu C, Abidov A, Friedman JD, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol. 2005;12:66–77.
Otaki Y, Betancur J, Sharir T, Hu LH, Gransar H, Liang JX, et al. 5-year prognostic value of quantitative versus visual MPI in subtle perfusion defects: results from REFINE SPECT. JACC Cardiovasc Imaging. 2020;13:774–85.
Zampella E, Acampa W, Assante R, Nappi C, Gaudieri V, Mainolfi CG, et al. Combined evaluation of regional coronary artery calcium and myocardial perfusion by 82Rb PET/CT in the identification of obstructive coronary artery disease. Eur J Nucl Med Mol Imaging. 2018;45:521–9.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138:e618–51.
Simon R, Makuch RW. A non-parametric graphical representation of the relationship between survival and the occurrence of an event: application to responder versus non-responder bias. Stat Med. 1984;3:35–44.
Mantel N, Byar DP. Evaluation of response time data involving transient states: an illustration using heart-transplantation data. J Am Stat Assoc. 1974;69:81–6.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (London, England). 2020;395:507e13.
Yang YM, Hsu CY, Lai CC, Yen MF, Wikramaratna PS, Chen HH, et al. Impact of comorbidity on fatality rate of patients with Middle East respiratory syndrome. Sci Rep. 2017;7:11307.
Nappi C, Megna R, Acampa W, Assante R, Zampella E, Gaudieri V, et al. Effects of the COVID-19 pandemic on myocardial perfusion imaging for ischemic heart disease. Eur J Nucl Med Mol Imaging. 2021;48:421–7.
Einstein AJ, Shaw LJ, Hirschfeld C, Williams MC, Villines TC, Better N, INCAPS COVID Investigators Group, et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77:173–85.
Hirschfeld CB, Shaw LJ, Williams MC, Lahey R, Villines TC, Dorbala S, INCAPS-COVID Investigators Group, et al. Impact of COVID-19 on cardiovascular testing in the United States versus the rest of the world: the INCAPS-COVID study. JACC Cardiovasc Imaging. 2021;14:1787–99.
Li M, Dong Y, Wang H, Guo W, Zhou H, Zhang Z, et al. Cardiovascular disease potentially contributes to the progression and poor prognosis of COVID-19. Nutr Metab Cardiovasc Dis. 2020;30:1061–7.
Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A. Myocardial injury and COVID-19: possible mechanisms. Life Sci. 2020;253:117723.
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7.
Beyerstedt S, Casaro EB, Rangel ÉB. COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis. 2021;40:905–19.
Moccia F, Gerbino A, Lionetti V, Miragoli M, Munaron LM, Pagliaro P, et al. COVID-19-associated cardiovascular morbidity in older adults: a position paper from the Italian Society of Cardiovascular Researches. Geroscience. 2020;42:1021–49.
Dhakal BP, Sweitzer NK, Indik JH, Acharya D, William P. SARS-CoV-2 Infection and cardiovascular disease: COVID-19 heart. Heart Lung Circ. 2020;29:973–87.
Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319–29.
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
R.A, M.P., A.C., and W.A. conceptualized the paper; T.M., V.G., E.Z., C.G.M., E.C., C.N., E.C., R.B., and G.Z. evaluated and reported the imaging findings; V.C. and R.G collected follow-up data; R.A, M.P., A.C., and W.A. drafted the manuscript; and all the authors revised and commented on the paper and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed approval
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology
Rights and permissions
About this article
Cite this article
Assante, R., D’Antonio, A., Mannarino, T. et al. Impact of COVID-19 infection on short-term outcome in patients referred to stress myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 49, 1544–1552 (2022). https://doi.org/10.1007/s00259-021-05619-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05619-2