- 1School of Medicine, St. George’s University of London, London, United Kingdom
- 2University of Nicosia Medical School, University of Nicosia, Nicosia, Cyprus
- 3Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN, United States
- 4Division of Gastroenterology and Hepatology, Indiana University, Indianapolis, IN, United States
- 5School of Biomedical Sciences, The University of Queensland, Brisbane, QLD, Australia
- 6Department of Psychiatry and Psychology, Mayo Clinic Arizona, Phoenix, AZ, United States
- 7Department of Neuroscience, Mayo Clinic Arizona, Phoenix, AZ, United States
Objective: This systematic review and meta-analysis aims to explore overall prevalence of burnout among physicians during early and late COVID-19 pandemic and geographical differences in burnout.
Methods: This review was registered prospectively with PROSPERO (CRD42022327959). A comprehensive search of several databases, including Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, PsycINFO, and Scopus, spanning from December 2019 to May 2022 was conducted. Eligible studies included physicians or medical professionals including physicians that worked directly or indirectly with COVID-19 patients, whilst reporting burnout outcomes using a validated scale. Literature that did not include physicians or did not occur in a hospital setting were excluded. Literature including medical students were also excluded.
Results: Forty-five observational studies were included, all of which were cross-sectional studies. The pooled estimate of overall prevalence of burnout was 54.60% (95% CI: 46.7, 62.2). Mean emotional exhaustion, depersonalization, and personal accomplishment was found to be 22.06% (95% CI: 18.19, 25.94), 8.72 (95% CI: 6.48, 10.95) and 31.18 (95% CI: 27.33, 35.03) respectively. Frontline workers displayed higher rates of burnout than second-line healthcare workers (HCW) (OR: 1.64, 95% CI: 1.13, 2.37). Studies from the early pandemic period reported burnout prevalence of 60.7% (95% CI: 48.2, 72) compared to a prevalence of 49.3% (95% CI: 37.7, 60.9) from the late pandemic period. Geographically, burnout was highest amongst Middle East and North Africa (MENA) studies (66.6%, 95% CI: 54.7, 78.5), followed by Europe (48.8%, 95% CI: 40.3, 57.3) and then South America (42%, 95% CI: –0.4, 84.4). Lastly, burnout prevalence overall (OR = 0.77, 95% CI: 0.36, 1.67) emotional exhaustion (MD = –0.36, 95% CI: –4.64, 3.91), depersonalization (MD = –0.31, 95% CI: –1.80, 1.18), and personal accomplishment (MD = 0.55, 95% CI: –0.73, 1.83) were found comparable between physicians and nurses.
Conclusion: COVID-19 has had significant consequences on HCW burnout. Further research is needed to examine early signs of burnout and to develop effective coping strategies.
1. Introduction
With the Corona virus disease 2019 (COVID-19) pandemic caused by Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) slowly easing its grip on global healthcare concerns and nearing its resolution, attention is now shifting toward the long term imprint this crisis has left worldwide.
One such imprint is job burnout, a psychological syndrome that stems from extended exposure to work-related stressors that occur in workers who interact with other individuals in some capacity, typically that of staff-client. Due to this, job burnout is observed across a variety of occupational sectors, including healthcare, social services, and education and its effects compromise not only the individual but the society as a whole (1).
Measurement of burnout is divided into three distinct dimensions: emotional exhaustion, feelings of cynicism (depersonalization), and a sense of ineffectiveness (lack of personal accomplishment) (2), as described by the most widely used burnout scale, the Maslach Burnout Inventory (MBI) (1). With emotional exhaustion, workers feel emotionally spent and have a sense of apathy regarding their work. Depersonalization is characterized as negative and cynical feelings toward oneself and those one interacts with. These contemptuous feelings are often related to feeling emotionally depleted, hence the correlation between depersonalization and emotional exhaustion. Lack of personal accomplishment describes an overall feeling of unsatisfaction with oneself and their work (1). Other validated scales used for measuring burnout have similar outcomes, including the Professional Quality of Life (ProQOL) scale (3), the Oldenburg Burnout Inventory (OLBI) (4), the Copenhagen Burnout Inventory (CBI) (5), the Stanford Professional Fulfillment Index (PFI) (6, 7).
Individuals with burnout suffer harmful effects of negative emotions, substance abuse and suicidal ideation (8). In physicians, this domino effect may manifest as medical errors, longer recovery times and increased physician turnover due to reduced physician productivity (9). Consequently, these effects pose a greater economic burden to the healthcare system by increasing healthcare costs for replacement of vacancies from resignations (10). Burnout does not only affect physicians, but also carries a toll on all healthcare workers (HCW); frontline workers and nurses in certain countries may be at higher risk of developing burnout. During the pandemic, frontline and second-line HCW were exposed to varying levels of stressors. Frontline workers are defined as those working directly with COVID-19 patients, while second-line workers are defined as HCW with no direct exposure to COVID-19 patients. Though both groups experienced psychological effects due to the nature of their work, frontline workers were more vulnerable due to their proximity with COVID-19 patients (11), (12). Additionally, burnout affects physicians and nurses differently, given that nurses are more intensely exposed to their patients and thus experience more work-related stressors (13). HCW burnout levels have also been shown to be higher in lower income countries than in middle or high income countries (14).
It is not entirely clear whether HCW were more vulnerable to burnout during early pandemic period, when there was shortage of personal protective equipment (PPE), limited knowledge about the illness, and no proper prevention treatment (15, 16) or during the later stages when the prolonged stress accumulated, and the number of infected individuals rose exponentially (17).
The issues of physician burnout have been adequately studied, and have shown a negative effect on depression, stress, mood disorders, suicides, and poor patient quality care (18–20). This remains true for other healthcare professions, as high nurse burnout has been linked with increased turnover, leading to nurse shortage and poorer patient care outcomes (21). Although these phenomena have been studied, measures have not been taken to alleviate this issue. Understanding the subtle differences in burnout domains between different groups and at different geographical locations could provide valuable guidance in developing effective intervention strategies.
As frontline HCW continue to respond to the COVID-19 outbreak, it is of utmost importance that we invest immediately in the psychological wellness of HCW. Burnout in medical professionals has generally been overlooked and the novelty of the COVID-19 outbreak presents a gap in understanding burnout prevalence trends in healthcare in such unforeseen situations. It is in the best interest of public health to start acting on this issue now before the burnout-related effects progress any further. Therefore, the aim of this meta-analysis is to explore burnout prevalence in HCW, focusing on physicians, during the COVID-19 pandemic as well as differences in burnout prevalence according to region, COVID-19 timelines, and healthcare profession (whether nurse or physician) to better understand this hidden healthcare crisis.
2. Methods
2.1. Search strategy and data sources
The review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (22). A comprehensive search of several databases from December 2019 to May 2022 was conducted for pertinent English language publications. The databases included Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, PsycINFO, and Scopus. The search strategy was designed and conducted by an experienced librarian. Controlled vocabulary with keywords was used to search for studies describing COVID-19 and physician burnout. Supplementary Item 1 outlines the search strategy listing all the search terms used and how they are combined. This review was registered prospectively with PROSPERO (CRD42022327959).
2.2. Eligibility criteria and quality assessment
Eligible studies were observational studies that met all the following inclusion criteria: (1) Studies of physicians or medical healthcare professionals including physicians who were frontline workers or a mix of frontline and second-line workers during the COVID-19 pandemic in a hospital setting; (2) Reported burnout outcomes using a validated questionnaire. With regards to study designs, original, observational studies excluding case reports, case series, abstracts, conference abstracts, and articles that were not reported in English. The study also excluded medical school students and studies that did not delineate results between medical and non-medical HCW (e.g., administration, security staff). There was no comparison group in our study. The quality of each study was independently evaluated by two authors (MM and OS-O) using the Newcastle Ottawa Assessment Scale. The scale assesses sample Selection (representativeness of the target population, sample size, comparability between respondents and non-respondents, and outcome ascertainment), Comparability (comparability between subjects in different outcome groups), and Outcomes (method of measurement of outcome and statistical test used). A maximum of one star can be given to a study in each of the categories under Selection and Outcome, and a maximum of two stars can be given for Comparability (23). The difference in the determination of quality was resolved by discussion with a third author until a consensus was reached (RM). Results of the quality assessment of all included studies are shown in Supplementary Item 2.
2.3. Questionnaires
2.3.1. Maslach burnout inventory
The MBI scale measures burnout with 22 items measuring three dimensions: nine items measuring emotional exhaustion, five measuring depersonalization, and eight measuring personal accomplishment. Traditionally, high scores on both emotional exhaustion and depersonalization and low scores on personal accomplishment were associated with increased burnout risk (24). Each item is measured using a five- or seven-point Likert scale depending on the study. Some of the included studies used a modified MBI were only one (emotional exhaustion) (25) or two (emotional exhaustion and depersonalization) (26, 27) of the MBI subscales were used to evaluate burnout in their population.
2.3.2. Professional quality of life
The ProQOL scale measures the effects of traumatic stress experience on work burnout, compassion satisfaction, and compassion fatigue. Each subscale has ten items and cut-offs depend on the type of Likert scale used. Traditionally, a five-point Likert scale is employed, and for each subscale, moderate levels of burnout are indicated by scores of 23–41, whereas scores over 41 indicate high levels (28).
2.3.3. Oldenburg burnout inventory
The OLBI consists of two subscales, exhaustion, and disengagement, measured by eight positively and negatively framed items each. It is used as an alternative to the MBI so that the subscales of depersonalization and personal accomplishment are seen as consequences of stress and coping (29). The OLBI scale generally uses a four-point Likert scale going from one (strongly agree) to four (strongly disagree). Higher scores are associated with worse burnout symptoms and in most studies, burnout is defined as positive when the total score is greater or equal to 21 (30).
2.3.4. Copenhagen burnout inventory
The CBI consists of nineteen items and three different subscales which apply to a greater range of occupational sectors; personal related burnout (six items), work-related burnout (seven items), and client-related burnout (six items) (31). The work-related burnout sector uses a 5-point Likert scale, with higher scores indicating higher levels of burnout (32).
2.3.5. Stanford professional fulfillment index
The Stanford PFI was developed to evaluate both burnout and physician professional well-being at work, with the two domains of burnout represented as interpersonal disengagement and work-exhaustion (33). Hence, the PFI is a sixteen-items scale with four items assessing work-exhaustion, six items evaluating professional fulfillment, and six items assessing interpersonal disengagement. Possible burnout scores range from zero to forty for burnout and zero to 24 for professional fulfillment (34).
2.3.6. Mini-Z survey
The Mini-Z burnout survey is a twelve-item measurement scale, with items one through eleven being five- point Likert scale assessing job satisfaction, stress, burnout, satisfactory control of working conditions, satisfactory time available for documentation of cases, chaos, professional value alignment with those of the department heads, good teamwork, time spent on electronic medical record at home, and gender or racial discrimination. Item 12 is the following open question: “Tell us more about your stresses and what we can do to minimize them” (7).
2.4. COVID timelines
In this paper, early pandemic period referred to the onset of the pandemic until August 2020, while late pandemic period referred to September 2020 onward, based off of general trends of the first (February 2020 to August 2020), second (September 2020 to Mid-February 2021), and third (Mid-February 2021 to June 2021) COVID-19 waves (35).
2.5. Geographical locations
We categorized studies into six regions, three with high income countries: Europe (Cyprus, France, Italy, Romania, Russia, and Spain), North America (Canada and the USA), and Australia, and three with middle/low-income countries: Asia (China, India, Malaysia, Pakistan, Singapore, South Korea, Taiwan, Turkey), Middle East and North Africa (MENA) (Egypt, Iran, Jordan, Qatar, Saudi Arabia), and South America (Argentina and Brazil).
2.6. Statistical analysis
The pooled means and proportions of our data were analyzed using a random, inverse variance method for continuous data and the Mantel-Haenszel method for dichotomous data. The heterogeneity of effect size estimates across the studies was quantified using the Q statistic and the I2 index (P < 0.10 was considered significant). A value of I2 of 0–25% indicates minimal heterogeneity, 26–50% moderate heterogeneity, and 51–100% substantial heterogeneity (36). Data analysis was performed using Open Meta analyst software (CEBM, Brown University, Providence, Rhode Island, USA) and RevMan software version 5.4 (Review Manager (RevMan) [Computer program]. The Cochrane Collaboration, 2020, Copenhagen, Denmark). If mean and standard deviation (SD) were unavailable, median was converted to mean using the formulas from the Cochrane Handbook for Systematic Reviews of Interventions (37). Authors were contacted three times to obtain additional information such as the exact Likert scale used in the MBI scale, clarification of setting (hospital or outpatient), and whether the population included only medical healthcare workers or non-medical staff as well. Publication bias was assessed using a funnel plot (38).
2.7. Data extraction
Following a thorough reading of the articles, the necessary information was retrieved using the summary and collection form. The title, responsible author, the sample size of the study, country and time of the study, study design, study participants based on their patient-facing roles (doctor, nurse, and other clinical), exposure of the participants to COVID-19 patients in the workplace, diagnostic instrument, and findings were all provided on this form. For each of the selected articles, summary forms were filled.
Necessary information was extracted from the articles and rechecked by two authors (MM and OS-O). The extraction included general information about the studies (title, author, study year and timeline of data collection, country, study design, and study setting), population characteristics (sample size, population gender, mean age, and professional role i.e., physician, nurse, or allied healthcare worker) and outcomes which included reported scores on the respective burnout scales used in each study.
3. Results
3.1. Identification and selection of studies
A literature search of several databases following PRISMA guidelines yielded 2,361 records, from which 2,147 records were eliminated by title and abstract screening. The remaining 163 records were then assessed for full text screening and 45 records were finally included in the study. Out of these 45 included studies, twenty were utilized for quantitative analysis. The PRISMA flow diagram is shown in Supplementary Item 3.
3.2. Study characteristics
All the 45 observational studies included were cross-sectional. A total of 29,785 medical healthcare professionals were included in the study population. Mean age range of workers was 27–47 years. A total of 27 (8, 26, 27, 39–59) studies included both frontline and second-line workers in their studies, while twelve studies (24, 25, 28, 60–68) had only frontline workers and six (32, 69–73) did not delineate between frontline and second-line workers. In terms of regions, fifteen (33.3%) of studies (28, 41, 45, 47, 51, 55, 56, 58, 59, 63, 67, 68, 71, 72, 74) took place in Asia. Europe (8, 26, 42, 48, 53, 57, 60, 62, 66, 69, 73) was represented by 11 (24.4%) studies while the Middle East and North Africa (MENA) (25, 32, 39, 44, 46, 49, 50, 64, 65, 70) were represented by ten (22.2%) studies each. South America (24, 40, 52, 54, 61, 75), North America (27, 76), and Australia (43) were represented by six (13.3%), two (4.4%), and one (2.2%) study respectively. Burnout results between nurses and physicians were compared in fourteen studies (32, 42, 43, 53, 55, 56, 62, 63, 67–71, 74). Twenty-eight studies (8, 25, 27, 28, 32, 39, 40, 42–44, 47, 49, 50, 52, 53, 55–59, 62, 63, 65, 67, 68, 70, 73, 75) conducted data collection during the early stages of the COVID-19 pandemic and fifteen (24, 26, 41, 44–46, 48, 51, 54, 60, 62, 66, 69, 71, 74, 76) studies were conducted during the later stages. Two studies (26, 61) did not specify the time of data collection. Burnout was measured using a variety of questionnaires. Thirty studies (8, 24–27, 39–42, 44, 46, 48, 49, 53, 54, 57–59, 61–64, 66, 68, 70–72, 74, 76) used the MBI questionnaire or some variation of it. All other information regarding sample size, timeline of data collection, and age distribution are included in Table 1.
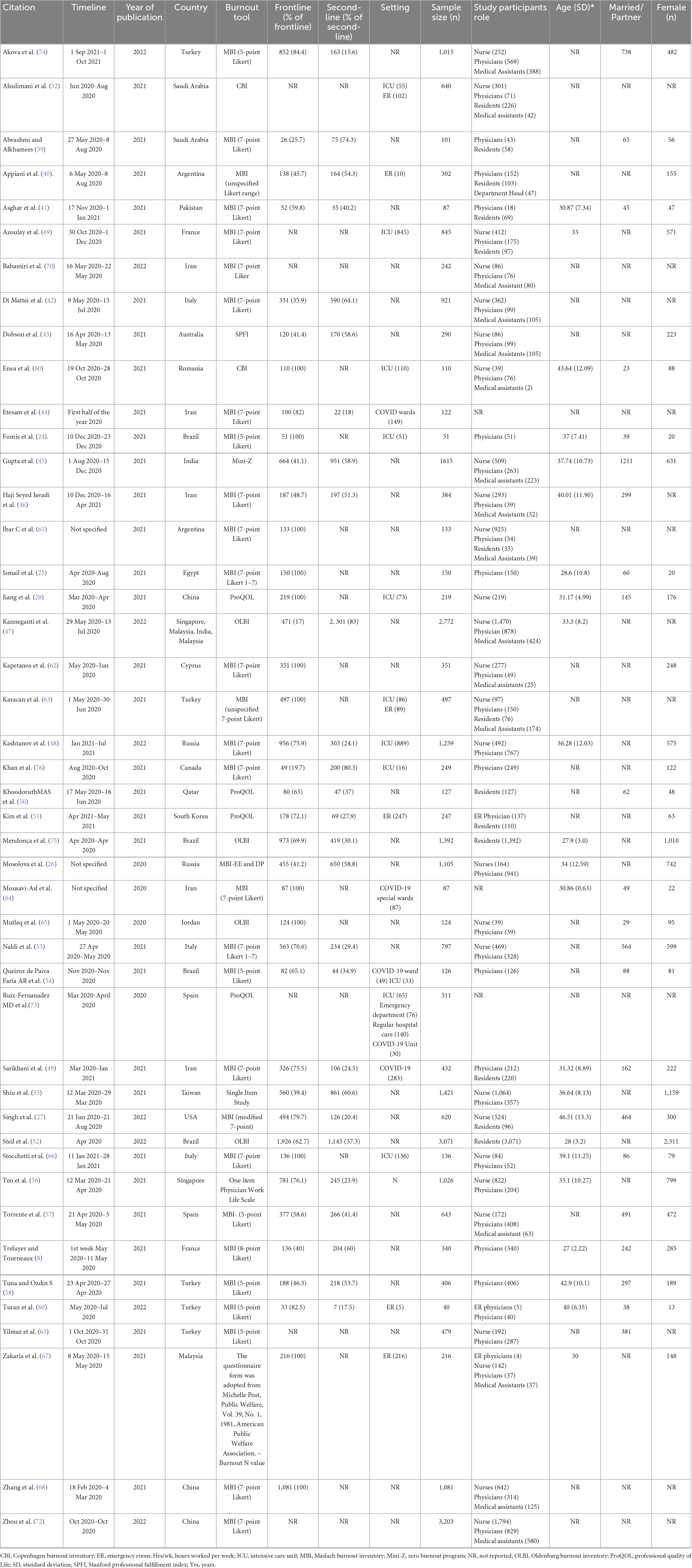
3.3. Pooled estimated prevalence of burnout and its main domains
As shown in Figure 1, overall burnout was evaluated among thirteen studies (8, 24, 39, 40, 44, 48, 49, 57, 61, 66, 69, 70, 76) with MBI or a modified MBI, and the prevalence was 54.6% (95% CI: 46.7, 62.2, I2 = 96.12%). Mean emotional exhaustion, depersonalization, and personal accomplishment were found to be 22.06 (95% CI: 18.19, 25.94, I2 = 98.81%), 8.72 (95% CI: 6.48, 10.96, I2 = 99.16%), and 31.18 (95% CI: 27.33, 35.03, I2 = 99.34%) respectively.
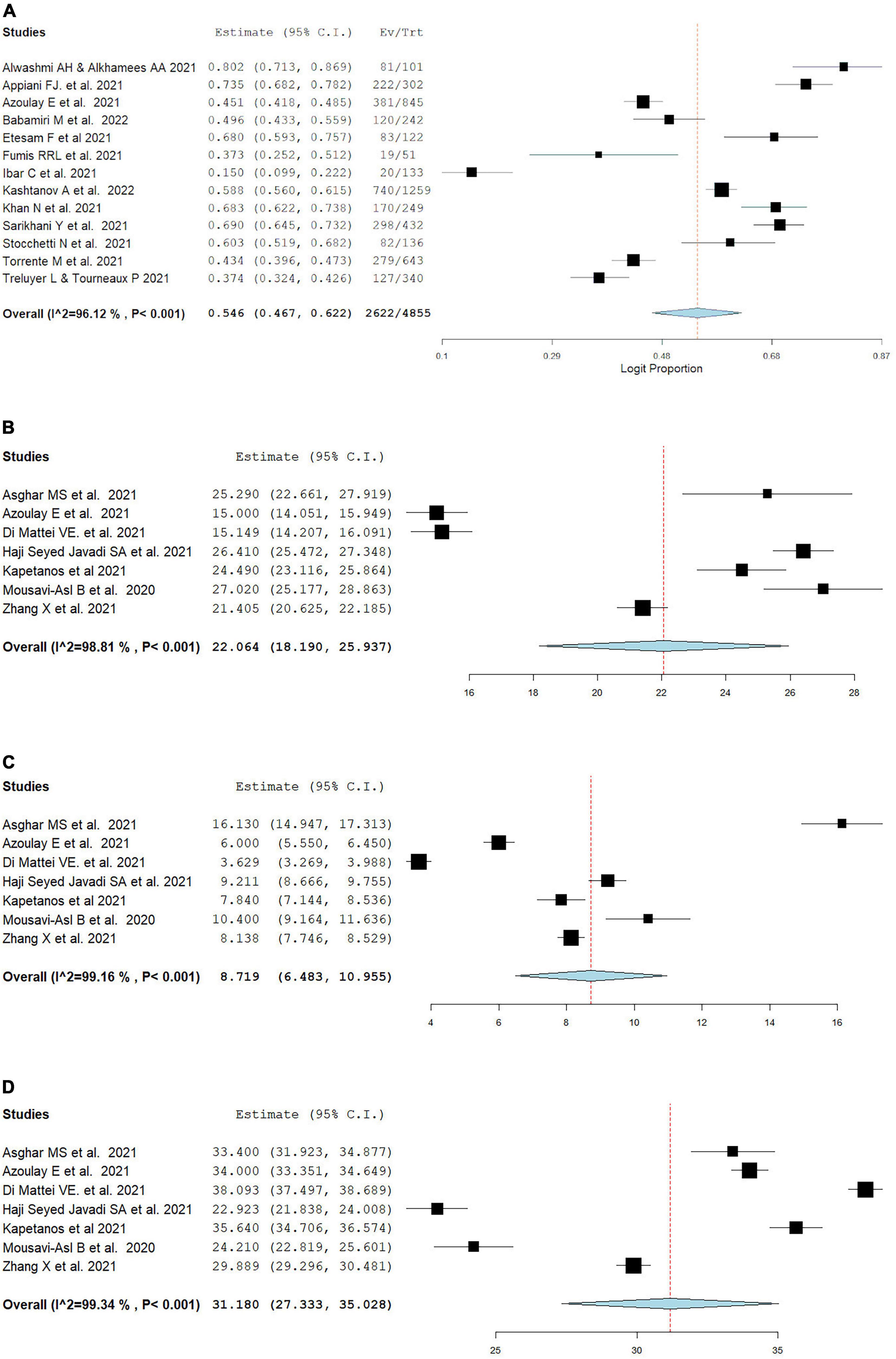
Figure 1. Pooled estimate of overall burnout in healthcare workers according to the Maslach burnout inventory by (A) overall prevalence, (B) emotional exhaustion, (C) depersonalization, (D) personal accomplishment.
3.4. Burnout in frontline vs second-line HCW
Overall burnout was evaluated with the MBI scale, and the frontline workers had a higher rate of burnout compared to second-line HCW (OR: 1.64, 95% CI: 1.13, 2.38, I2 = 67.14%), as can be seen in Figure 2. Mean emotional exhaustion and depersonalization were found to be higher in frontline than in second-line HCW (MD = 6.55, 95% CI: 2.35, 10.76, I2 = 88.48%) and (MD = 3.79, 95% CI: 1.57, 6.01, I2 = 90.45%) respectively. Mean personal accomplishment had comparable levels in frontline workers versus second-line workers (MD = –1.69, 95% CI: –5.60, 2.23, I2 = 91.41%).
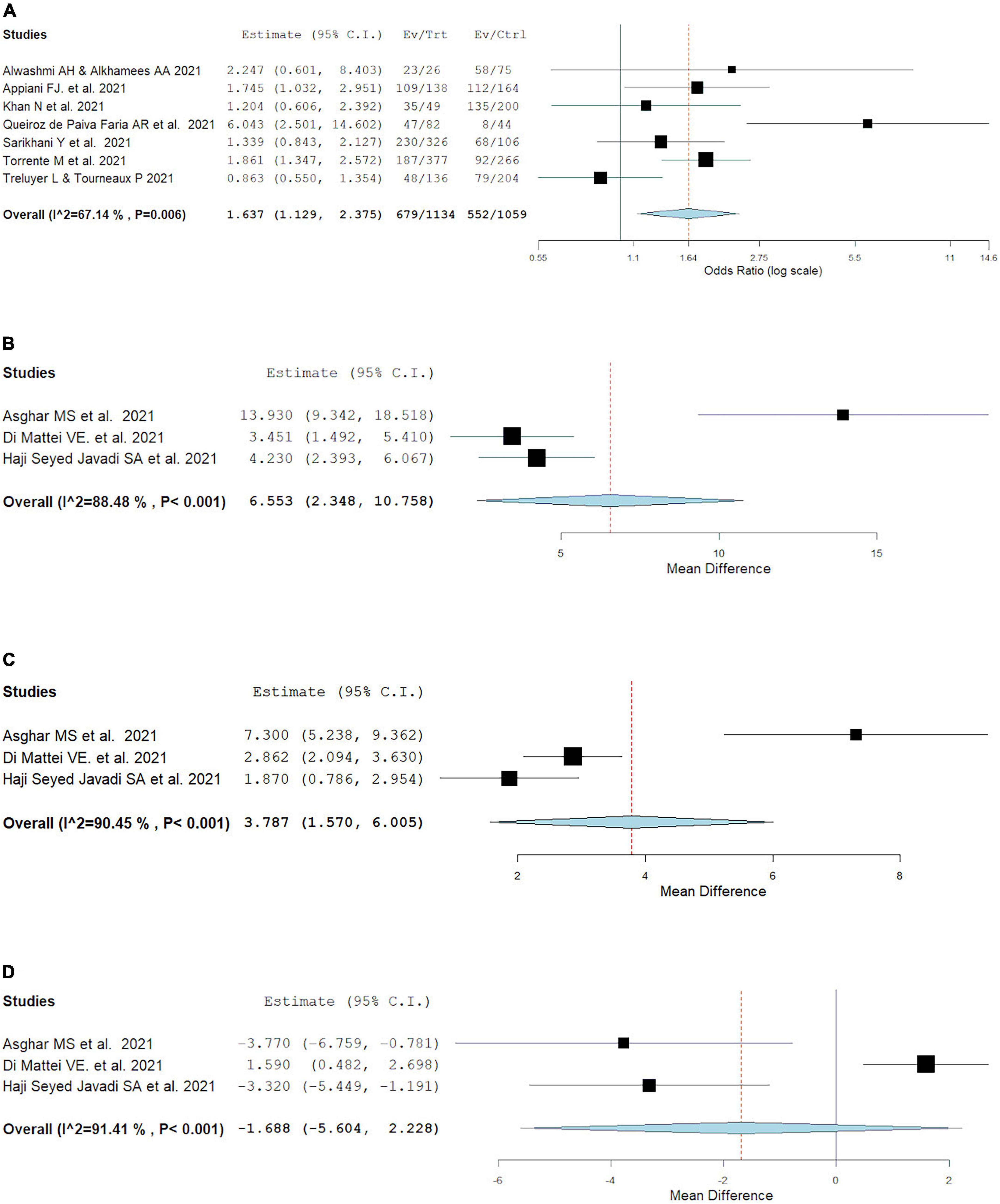
Figure 2. Pooled estimate of burnout in frontline vs second-line healthcare workers according to Maslach burnout inventrory by (A) overall prevalence, (B) emotional exhaustion prevalence, (C) depersonalization prevalence, (D) personal accomplishment prevalence.
3.5. Prevalence of burnout during early vs late pandemic
Overall burnout prevalence in the early wave of the pandemic was found to be 60.7% (95% CI: 48.2, 72.0%, I2 = 96.7%) of the population, as evident in Figure 3. Overall burnout in the later pandemic period was shown to be prevalent in 49.3% (95% CI: 37.7, 60.9%, I2 = 96.74%) of the population.
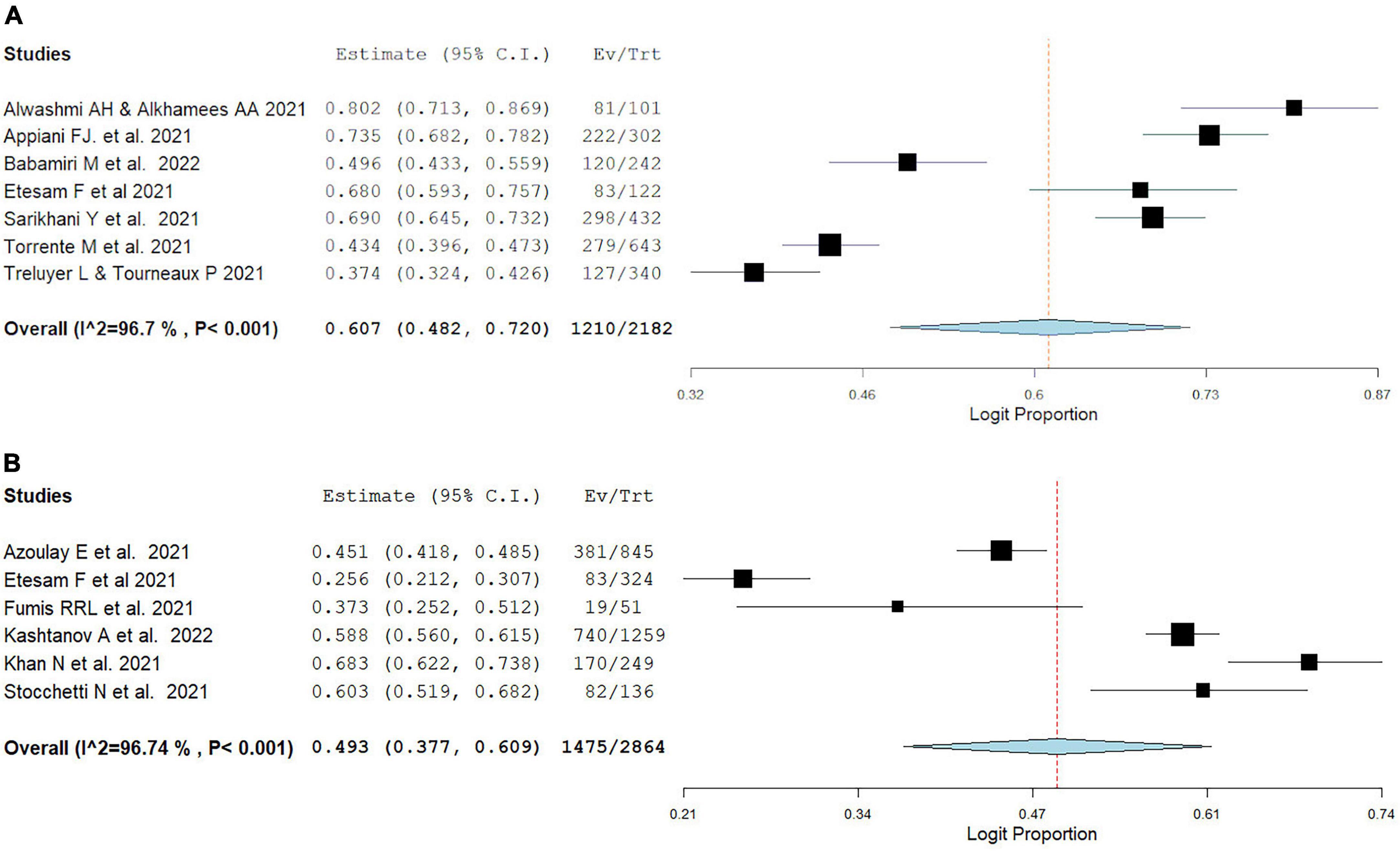
Figure 3. Pooled estimate of burnout prevalence according to the Maslach burnout inventory in (A) early pandemic period, (B) late pandemic period.
3.6. Prevalence of burnout in different geographical locations
As can be seen in Figure 4, burnout prevalence among HCW was highest amongst MENA studies (66.6%, 95% CI: 54.7, 78.5%, I2 = 92.67%), second highest prevalence was observed in Europe (48.8%, 95% CI: 40.3, 57.3%, I2 = 95.27%) reporting burnout, and finally the lowest burnout prevalence was found in South America (42%, 95% CI: –0.4, 84.4%, I2 = 99.08%). We could not estimate the pooled prevalence in Asian studies because they used different scales to measure burnout.
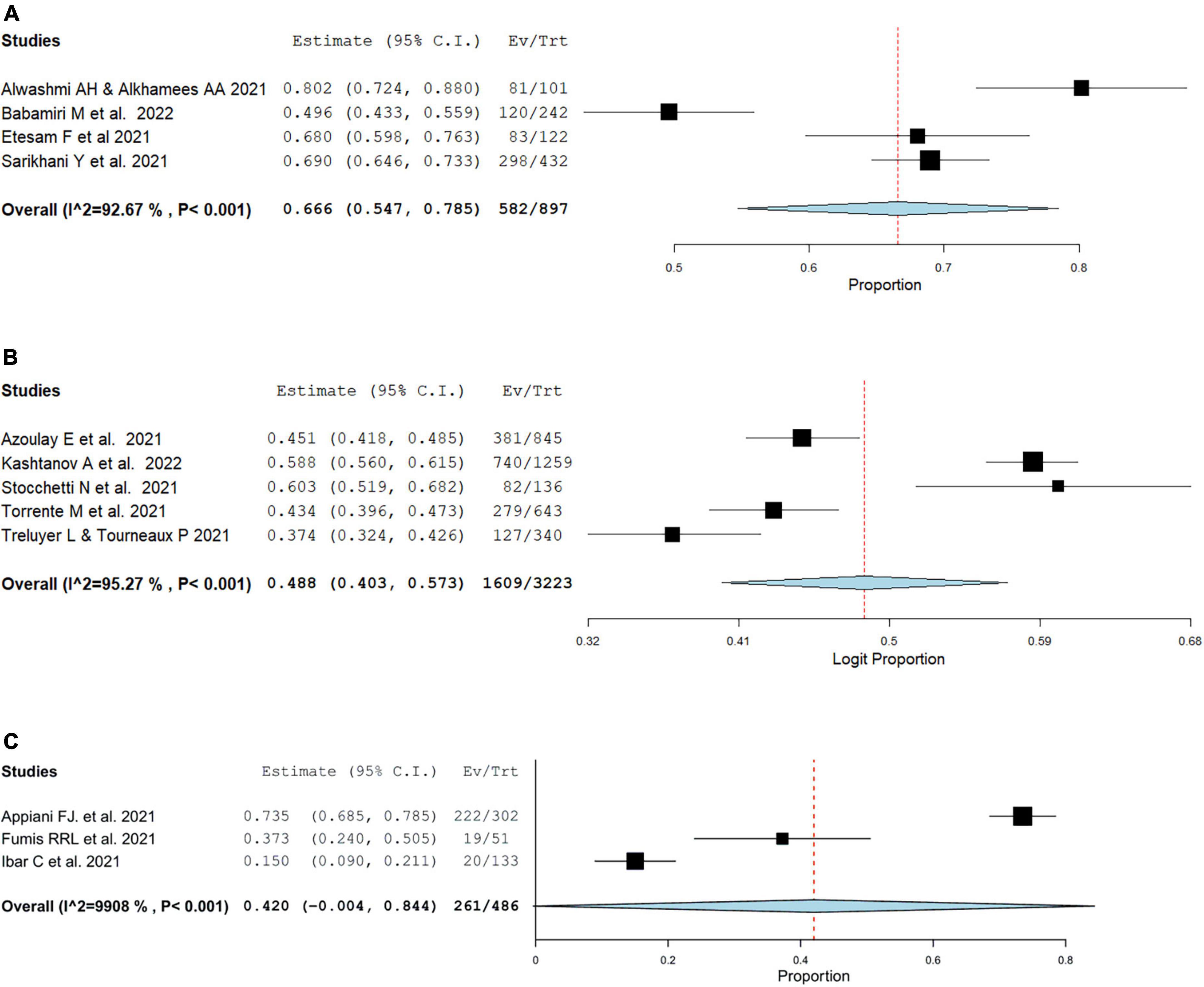
Figure 4. Pooled estimate of burnout prevalence according to Maslach burnout inventory in (A) MENA, (B) Europe, (C) South America. Asian studies forest plots could not be pooled due to burnout scale discrepancy.
3.7. Prevalence of burnout among nurses vs physicians
Fourteen studies compared burnout outcomes between physicians and nurses. Among fourteen studies, four studies (42, 62, 68, 69) reported emotional exhaustion, depersonalization, and personal accomplishment prevalence, while two studies (69, 70) reported overall MBI burnout. In comparison to nurses, physicians had comparable rates of overall burnout rate (OR = 0.77, 95% CI: 0.36, 1.67, I2 = 78.11%). Emotional exhaustion, depersonalization, and personal accomplishment mean result were also comparable between physicians and nurses (MD = –0.36, 95% CI: –4.64, 3.91, I2 = 92.5%) (MD = –0.31, 95% CI: –1.80, 1.18, I2 = 85.51%) (MD = 0.55, 95% CI: –0.73, 1.83, I2 = 66.41%), as showcased in Figure 5.
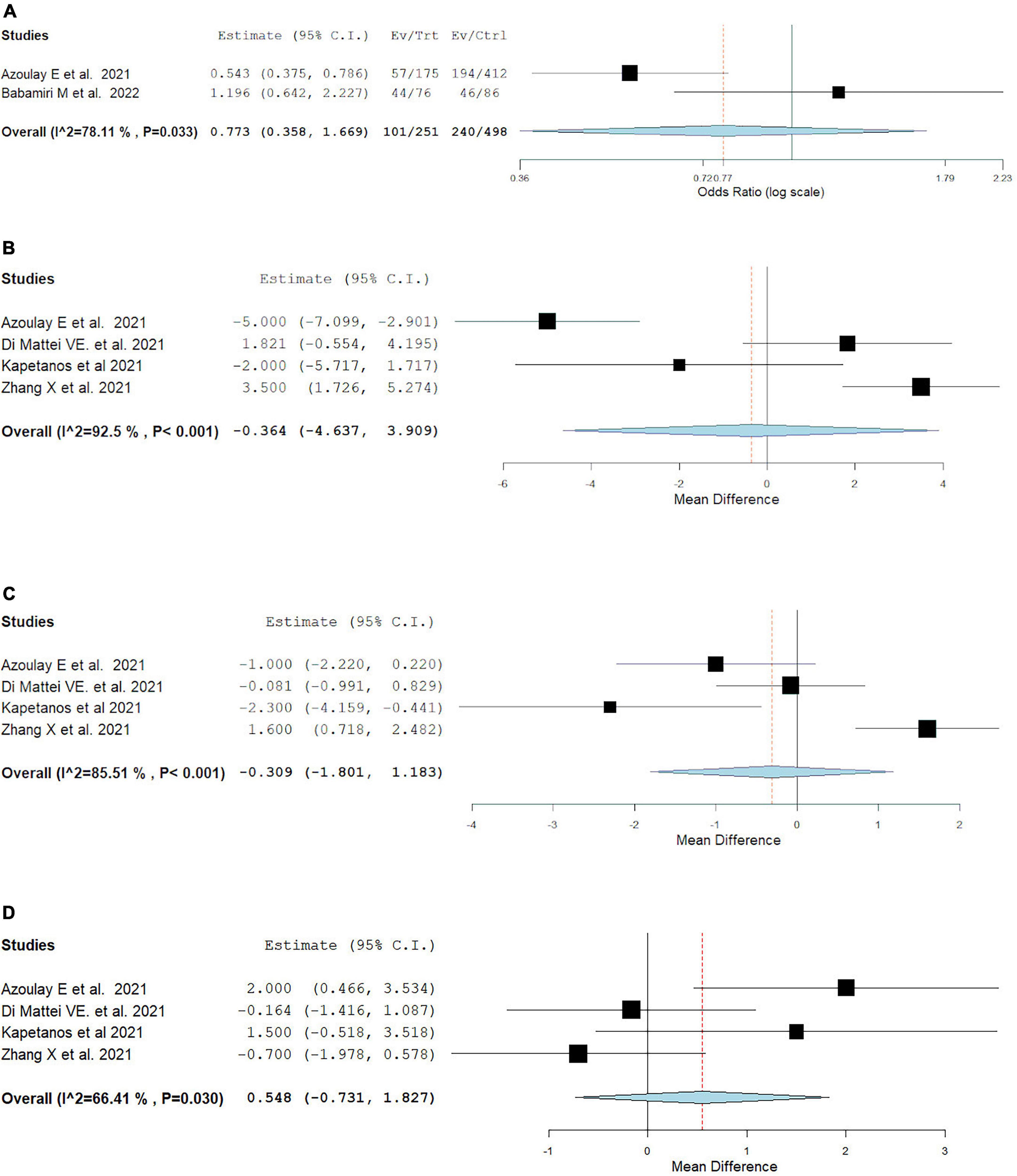
Figure 5. Pooled estimate of burnout prevalence in nurses vs physician according to Maslach burnout inventory by (A) overall prevalence, (B) emotional exhaustion prevalence, (C) depersonalization prevalence, (D) personal accomplishment prevalence.
4. Discussion
The COVID-19 pandemic has proven to be an enormous burden on healthcare systems across the globe, placing considerable strain on the psychological well-being of all healthcare workers (HCW) involved. The results of this meta-analysis demonstrate that more than half of HCW experienced burnout at some point during the pandemic. As expected, frontline, compared to second-line HCWs, were found to have higher rates of burnout. In addition, burnout prevalence was shown to be higher during the early pandemic as compared to late and specifically in MENA countries. Finally, physicians and nurses were found to be comparable in overall burnout and all its domains. This meta-analysis specifically examines the prevalence of specific burnout domains which could be utilized as potential targets for therapeutic intervention. To our knowledge, no previous meta-analysis has investigated burnout based on frontline versus second-line HCW, nurses versus physician, early versus late pandemic waves, as well as between regions. Additionally, previous reviews included medical and non-medical healthcare workers, in and out of hospital setting, while this review focused specifically on medical healthcare staff within a hospital setting. The cut-off scores for low, moderate, and high levels of the MBI subdomains used in this review may be found in Supplementary Item 4.
Lack of personal accomplishment, defined as having a negative outlook on the worth of one’s work (1), was found to be the most affected domain during the COVID-19 pandemic out of the three subscales of the MBI. Indeed, the mean score for personal accomplishment referred to a low score as per MBI subscale cut-off ranges, while mean scores for emotional exhaustion and depersonalization were found to indicate moderate levels (77). Increased stress levels are linked to reduced personal accomplishment and feelings of low self-esteem (78). This could be due to increased workload, inadequate protective personal equipment, increased risk of infection, emotional strain of caring for patients suffering alone in confinement (79), and difficult decision making due to scarce resource allocation (80). All these factors were undoubtedly experienced by HCWs during the pandemic, which could lead to a reduced level of effectiveness of care that may affect one’s outlook on their accomplishments as healthcare providers, especially in the case of frontline workers (54).
Frontline workers were at higher risk of experiencing burnout compared to their second-line worker colleagues. They also experienced higher mean scores for emotional exhaustion and depersonalization. Aside from fear of getting infected or spreading the infection to their loved ones, frontline HCW became the target of stigmatization in their communities, with people viewing this group as a possible cause of virus transmission (81). Frontline workers also experienced increased workload coupled with the unique demands of a novel pandemic and reported elevated levels of psychological outcomes such as depression, post-traumatic disorder, and anxiety (12). This in turn provides feasible rationale for the disparity in reported burnout levels seen between frontline and second-line HCWs. However, shortage of HCWs also led to increased workload of second-line workers, leading to higher prevalence of poor sleep quality and anxiety seen in this cohort (82). Further insight into prolonged high workload effect on the mental health and well-being of HCWs could be elucidated by comparing burnout prevalence in early and late pandemic periods.
The early pandemic period was found to be associated with higher prevalence of burnout compared to late pandemic period. However, a study by Melnikow et al. explored burnout prevalence in the first and second waves of the pandemic and found an increase in overall burnout prevalence in the second wave compared to the first wave (83). They also reported that the increased burnout prevalence applied to all frontline specialties except emergency medicine, who displayed reduced burnout results in the second wave compared to the first (Professional Fulfillment Index Burnout Composite Scale score difference: –0.09, 95% CI: –0.53, 0.34), though these differences were not significant. As the pandemic ensued, increased workload, cases, and strain on resources could explain the increase in burnout across the waves in non-emergency specialties as reported by Melnikow et al. Yet, despite this strain, the exercise of various personal resilience and institutional strategies to manage burnout would explain the observed prevalence rates of burnout being lower in the second wave when compared to the first. Also, COVID-19 knowledge and preparedness increased over time thus decreasing COVID-19 fear, which has been shown to correlate with higher levels of burnout among healthcare professionals (84). On the other hand, the differences in prevalence could be attributed to several confounding factors given that the early and late pandemic studies were conducted with different populations, with different sample sizes, and in different countries and regions.
Out of the three regions studied, HCW in MENA displayed a higher prevalence of burnout compared to Europe and South America (66.6, 48.8, and 42%). It is important to note that a contributor to this observation is the number of included studies. South America had the least amount of included studies for the subgroup analysis and an overall total of six studies (24, 40, 52, 54, 61, 75) whereas MENA (25, 32, 39, 44, 46, 49, 50, 64, 65, 70) and Europe (8, 26, 42, 48, 53, 57, 60, 62, 66, 69) both had ten included studies each. We could not estimate pooled prevalence from Asian studies due to wide variability in rating scales. MENA countries report a scarcer number of resources aimed at alleviating burnout compared to European countries (85). Other differences in prevalence can be attributed to cultural differences as well as variation in healthcare systems, as cultural differences may explain the roles physicians play in addition to patient’s attitudes toward their healthcare providers (86). The cultural context of healthcare systems is also thought to play a role in physician versus nurses’ social acknowledgment, affecting their mental health status (87).
Physicians were found to have a comparable risk of burnout with nurses, as well as comparable mean scores for emotional exhaustion, depersonalization, and personal accomplishment. These results are consistent with the findings of another systematic review by Kunz M., Strasser M., and Hasan A 2019 (88), showing comparable levels of general stress levels and burnout between nurses and physicians. However, that review found that overall mental health outcomes were lower for nurses, with higher levels of depression, posttraumatic stress disorder (PTSD), and anxiety. By virtue of the nature of their job, nurses are more psychologically and physically involved in patient care and for longer hours than physicians are, which could explain these results (88). Some studies in Belgium explored the working conditions of nurses, where they suffer from insufficient teamwork, organizational support, and social recognition (87, 89, 90). On the other hand, it is important to remember that there are several confounding factors to consider, such as gender proportions and mean age (88). Though there have been conflicting results regarding gender susceptibility to burnout in nurses, it has been reported that female nurses displayed higher levels of emotional exhaustion than male nurses (91). Burnout also presents higher incidences amongst young professionals under the age of thirty, possibly due to lack of experience and self-confidence exerting additional stress on their workload (92). The comparable burnout results between nurses and physicians may be understood best by the unique demands of the COVID-19 pandemic on these professionals. The increased workload, medical demand, and overall fear of COVID-19 due to proximity to patients were experienced by both physicians and nurses, explaining comparable burnout results (93).
Aside from understanding the trends of burnout in HCW, it is also important to address the results of this study and put forth solutions to this crisis. Aryankhesal et al. conducted a systematic review on effective interventions for burnout in nurses and physicians. Per their findings, psychosocial training and mindfulness techniques had a positive effect on improving mental health and burnout in nurses, whereas, e-mental health approaches, communication skills training, and online programs had a positive effect for physicians (94). Innovative approaches to encouragement and motivation were also shown to reduce burnout and improve mental health in nurses (95). For HCW in general, a frequent suggestion has been to increase the availability and accessibility of Personal Protective Equipment (PPE), as well training on their usage (96–98).
Other possible solutions to address burnout in HCW include recruitment and training of volunteers to relieve the heavy workload first and second-line workers experience (99). Longitudinal departmental burnout assessment as well as off-duty social gatherings which provide an opportunity to share challenges and boost morale are potential ways to keep track of workers mental health and assess stressors (10). Updating electronic medical record keeping techniques increases efficiency and minimizes the stress of documentation (100, 101). Lastly, providing stress management and resiliency training aid in addressing perceived loss of control and autonomy could prove helpful (10). The implementation of these interventions coupled with the understanding of burnout trends during the COVID-19 pandemic are useful steps in alleviating the healthcare crisis posed by burnout in HCW.
5. Limitations
High heterogeneity was found in the meta-analysis results; however, this was expected since the studies had been conducted in different periods of the pandemic and different countries. The studies included all had different sample sizes, ranging from 40 to 3,203, which also posed a limitation and contributed to the heterogeneity of the meta-analysis results. Additionally, the study outcomes were assessed using self-reported questionnaires in uncontrolled settings, therefore introducing reporting bias. The MBI used to assess burnout in most of the studies was not used in a standardized manner thus leading to differences in results; different Likert scales were used and cut off values for outcome results as well as definition of burnout varied across studies. To address the issue of different Likert scales, meta-analysis was conducted separately between studies that reported mean overall burnout and subscale score results using the same MBI version and Likert scale measure. To resolve the challenge proposed by inconsistent cut-off scores, the cut-off values used in this study were derived from a systematic review of 41 studies that used the MBI questionnaire for burnout evaluation (62). Included studies used different scales for burnout assessment which led to the exclusion of several studies from the meta-analysis. As sampling error is an inherent limitation in meta-analyses, it was not accounted for. Instead, studies were assessed using the Newcastle Ottawa Assessment Scale, which investigates sample selection and representativeness. Furthermore, handsearching of journals and recurrent searches on google scholar during the completion of the study in order to pick up new articles that might not be indexed in the databases selected was not performed, in accordance to Cochrane guidelines (37). At the time of this review, previous study had compared between early and late pandemic burnout or between region burnout, therefore limiting the discussion on the results of said subgroup analyses.
6. Conclusion
The purpose of this study was to explore the burnout prevalence in frontline medical healthcare and second-line workers during the COVID-19 pandemic as well as differences in prevalence according to region, healthcare profession and COVID-19 timeline. Our findings showed that frontline workers were at higher risk of experiencing burnout compared to their second-line workers colleagues, the early pandemic was associated with a higher burnout prevalence compared to late pandemic period and MENA had a higher burnout prevalence than Europe or South America. Burnout prevalence between physicians and nurses were found to be comparable. Though there have been studies on this phenomenon, this study specifically studied burnout in medical healthcare providers that work in a hospital setting. Possible solutions for burnout were also discussed, especially since burnout had significant consequential effects on HCW, patients, and the healthcare system. Further studies comparing burnout according to pandemic waves as well as regional analyses should be conducted so that more concrete evidence can be obtained on timeline and regional effects to better prepare for future pandemics A standardized diagnostic inventory for burnout assessment, as well as uniform cut-off scores, should be implemented to make measuring and grading of burnout easier.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MM: conceptualization, methodology, investigation, data curation, writing – original draft, writing – review and editing, visualization, and project administration. OS-O: investigation, data curation, writing – original draft, writing – review and editing, and visualization. RM: conceptualization, methodology, software, formal analysis, investigation, writing – review and editing, visualization, and supervision. AB: data curation, validation, and writing – review and editing. HN: conceptualization, validation, writing – review and editing, software, and supervision. CT and OA: conceptualization, project administration, writing – review and editing, and supervision. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Leslie C. Hassett M.L.S for the literature search and Dr. Ao Shi for the assistance with data extraction.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1071397/full#supplementary-material
Supplementary Item 1 | Search strategy.
Supplementary Item 2 | Methodological quality assessment.
Supplementary Item 3 | Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram.
Supplementary Item 4 | Burnout scales.
References
1. Maslach C, Jackson S, Leiter M. The maslach burnout inventory manual. In: Zalaquett CP, Wood RJ editors. Evaluating Stress: A Book of Resources. Lanham, MA: The Scarecrow Press (1997). p. 191–218.
2. Rossi AM, Perrewe PL, Sauter SL. Stress and Quality of Working Life: Current Perspectives in Occupational Health. Charlotte, NC: Information Age Publishing (2006).
3. Stamm B. The Concise Manual for the Professional Quality of Life Scale. West Harrison, NY: Eastwoods, LLC (2010).
4. Demerouti E, Bakker AB. The oldenburg burnout inventory: a good alternative to measure burnout and engagement. In: Halbesleben JRB editor. Handbook of Stress and Burnout in Health Care. New York, NY: Nova Science (2008). p. 65–78.
5. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. (2005) 19:192–207. doi: 10.1080/02678370500297720
6. Vetter M, Vetter M, Cohn D, Yeager K, Fowler J. Utility of the Stanford Professional Fulfillment Index as a single survey instrument to assess holistic physician wellbeing. Gynecol Oncol. (2021) 162:S327–8. doi: 10.1016/S0090-8258(21)01272-5
7. The Institute for Professional Worklife. Mini Z Survey. Minneapolis, MN: The Institute for Professional Worklife (2020).
8. Treluyer L, Tourneux P. Burnout among paediatric residents during the COVID-19 outbreak in France. Eur J Pediatr. (2021) 180:627–33. doi: 10.1007/s00431-020-03907-x
9. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Internal Med. (2018) 283:516–29. doi: 10.1111/joim.12752
10. Bhardwaj A. COVID-19 pandemic and physician burnout: ramifications for healthcare workforce in the United States. J Healthc Leadersh. (2022) 14:91–7. doi: 10.2147/JHL.S360163
11. De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz S-A, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. (2021) 21:104. doi: 10.1186/s12889-020-10070-3
12. Billings J, Ching BCF, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Services Res. (2021) 21:923. doi: 10.1186/s12913-021-06917-z
14. Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, Azmand SA. Systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry. (2021) 12:758849. doi: 10.3389/fpsyt.2021.758849
15. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:43. doi: 10.1007/s11920-020-01166-z
16. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. (2021) 16:e0247679. doi: 10.1371/journal.pone.0247679
17. van den Boogaard M, Zegers M. Mental preparedness for prolonged periods of high workload – What did we learn from the covid-19 pandemic? Intensive Crit Care Nurs. (2022) 71:103258. doi: 10.1016/j.iccn.2022.103258
18. West CP, Tan Ad Fau – Habermann TM, Habermann Tm Fau – Sloan JA, Sloan Ja Fau – Shanafelt TD, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. (2009) 302:1294–300.
19. Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA (2011) 305:2009–10. doi: 10.1001/jama.2011.652
20. Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. (2016) 91:422–31. doi: 10.1016/j.mayocp.2016.02.001
21. Vahey DC, Aiken Lh Fau – Sloane DM, Sloane Dm Fau – Clarke SP, Clarke Sp Fau – Vargas D, Vargas D. Nurse burnout and patient satisfaction. Med Care. (2004) 42:II57–66. doi: 10.1097/01.mlr.0000109126.50398.5a
22. Moher D, Liberati A, Fau – Tetzlaff J, Tetzlaff J Fau – Altman DG, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
23. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
24. Fumis RRL, Costa ELV, Dal’Col SVC, Azevedo LCP, Pastore Junior L. Burnout syndrome in intensive care physicians in time of the COVID-19: a cross-sectional study. BMJ Open. (2022) 12:e057272. doi: 10.1136/bmjopen-2021-057272
25. Ismail TI, Shehata SF, Mahrous RSS. Occupational stress and burnout among frontline Egyptian anesthesiologists during COVID-19 outbreak in Egypt. Egypt J Anaesth. (2021) 37:91–9. doi: 10.1080/11101849.2021.1891704
26. Mosolova E, Sosin D, Mosolov S. Stress, anxiety, depression and burnout in frontline healthcare workers during two peaks of COVID-19 pandemic in Russia. Psychiatry Res. (2021) 306:114226. doi: 10.1016/j.psychres.2021.114226
27. Singh V, Young JQ, Malhotra P, McCann-Pineo M, Rasul R, Corley SS, et al. Evaluating burnout during the COVID-19 pandemic among physicians in a large health system in New York. Arch Environ Occupat Health. (2022) 77:819–27. doi: 10.1080/19338244.2021.2023084
28. Jiang W, Zhao X, Jiang J, Zhou Q, Yang J, Chen Y, et al. Hospital ethical climate associated with the professional quality of life among nurses during the early stage of COVID-19 pandemic in Wuhan, China: a cross-sectional study. Int J Nurs Sci. (2021) 8:310–7. doi: 10.1016/j.ijnss.2021.05.002
29. Tipa RO, Tudose C, Pucarea VL. Measuring burnout among psychiatric residents using the oldenburg burnout inventory (OLBI) instrument. J Med Life. (2019) 12:354–60. doi: 10.25122/jml-2019-0089
30. Steil A, Pereira Tokeshi AB, Bernardo LS, da Silva Neto GP, Davi RFJ, Bárbara AFS, et al. Medical residents’ mental distress in the COVID-19 pandemic: an urgent need for mental health care. PLoS One. (2022) 17:e0266228.
31. Papaefstathiou E, Tsounis A, Malliarou M, Sarafis P. Translation and validation of the Copenhagen Burnout Inventory amongst Greek doctors. Health Psychol Res. (2019) 7:7678. doi: 10.4081/hpr.2019.7678
32. Alsulimani LK, Farhat AM, Borah RA, AlKhalifah JA, Alyaseen SM, Alghamdi SM, et al. Health care worker burnout during the COVID-19 pandemic: a cross-sectional survey study in Saudi Arabia. Saudi Med J. (2021) 42:306–14. doi: 10.15537/smj.2021.42.3.20200812
33. Trockel M, Bohman B, Lesure E, Hamidi MS, Welle D, Roberts L, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. (2018) 42:11–24. doi: 10.1007/s40596-017-0849-3
34. Shanafelt TD, Makowski MS, Wang H, Bohman B, Leonard M, Harrington RA, et al. Association of burnout, professional fulfillment, and self-care practices of physician leaders with their independently rated leadership effectiveness. JAMA Netw Open. (2020) 3:e207961. doi: 10.1001/jamanetworkopen.2020.7961
35. Wu J, Scarabel F, McCarthy Z, Xiao Y, Ogden NH. A window of opportunity for intensifying testing and tracing efforts to prevent new COVID-19 outbreaks due to more transmissible variants. Can Commun Dis Rep. (2021) 47:329–38. doi: 10.14745/ccdr.v47i78a06
36. Higgins JP, Thompson Sg Fau – Deeks JJ, Deeks Jj Fau – Altman DG, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
37. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. New York, NY: John Wiley & Sons (2019). doi: 10.1002/9781119536604
38. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
39. Alwashmi AH, Alkhamees AA. Burnout and the psychological impact among physiatrists in Saudi Arabia during COVID-19. Int J Environ Res Public Health. (2021) 18:13. doi: 10.3390/ijerph18189621
40. Appiani FJ, Rodriguez Cairoli F, Sarotto L, Yaryour C, Basile ME, Duarte JM. Prevalence of stress, burnout syndrome, anxiety and depression among physicians of a teaching hospital during the COVID-19 pandemic. Arch Argent Pediatr. (2021) 119:317–24. doi: 10.5546/aap.2021.eng.317
41. Asghar MS, Yasmin F, Alvi H, Shah SMI, Malhotra K, Farhan SA, et al. Assessing the mental impact and burnout among physicians during the COVID-19 pandemic: a developing country single-center experience. Am J Trop Med Hygiene. (2021) 104:2185–9. doi: 10.4269/ajtmh.21-0141
42. Di Mattei VE, Perego G, Milano F, Mazzetti M, Taranto P, Di Pierro R, et al. The “Healthcare Workers’ wellbeing (benessere operatori)” project: a picture of the mental health conditions of italian healthcare workers during the first wave of the COVID-19 Pandemic. Int J Environ Res Public Health. (2021) 18:15. doi: 10.3390/ijerph18105267
43. Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Aust Psychiatry. (2021) 29:26–30. doi: 10.1177/1039856220965045
44. Etesam F, Akhlaghi M, Vahabi Z, Akbarpour S, Sadeghian MH. Comparative study of occupational burnout and job stress of frontline and non-frontline healthcare workers in hospital wards during COVID-19 pandemic. Iran J Public Health. (2021) 50:1428–35. doi: 10.18502/ijph.v50i7.6633
45. Gupta MD, Jha MK, Bansal A, Yadav R, Ramakrishanan S, Girish MP, et al. COVID 19-related burnout among healthcare workers in India and ECG based predictive machine learning model: Insights from the BRUCEE- Li study. Indian Heart J. (2021) 73:674–81. doi: 10.1016/j.ihj.2021.10.002
46. Haji Seyed Javadi SA, Rezaei B, Shafikhani A, Sarichloo ME. Comparative study of burnout and other aspects of mental health in medical staff working in Covid-19 and Non-Covid-19 Wards. Iran Red Crescent Med J. (2021) 23:1293.
47. Kanneganti A, Tan BY, Nik Ab Rahman NH, Leow AS, Denning M, Goh ET, et al. Safety attitudes, burnout and wellbeing among healthcare workers during the COVID-19 pandemic: an Indo-Pacific regional cross-sectional study. Singapore Med J. (2022) 10:10. doi: 10.11622/smedj.2022014
48. Kashtanov A, Molotok E, Yavorovskiy A, Boyarkov A, Vasil’ev Y, Alsaegh A, et al. A comparative cross-sectional study assessing the psycho-emotional state of intensive care units’ physicians and nurses of COVID-19 hospitals of a Russian Metropolis. Int J Environ Res Public Health. (2022) 19:06. doi: 10.3390/ijerph19031828
49. Sarikhani Y, Khatami K, Salehi-Marzijarani M, Sivandzadeh GR, Kouhi P, Shahabi S, et al. Burnout assessment among physicians and medical students: comparing time-periods of coronavirus disease outbreak in Shiraz. Shiraz E Med J. (2022) 23:e116275. doi: 10.5812/semj.116275
50. Khoodoruth MAS, Al-Nuaimi SK, Al-Salihy Z, Ghaffar A, Khoodoruth WNCK, Ouanes S. Factors associated with mental health outcomes among medical residents exposed to COVID-19. BJPsych Open. (2021) 7:e52. doi: 10.1192/bjo.2021.12
51. Kim C, Park KH, Eo EK, Kim Y-M, Eo SK, Han J. Burnout and resilience among emergency physicians at Korean University Hospitals during the COVID-19 pandemic: a cross-sectional analysis. Yonsei Med J. (2022) 63:372–9. doi: 10.3349/ymj.2022.63.4.372
52. Steil A, Tokeshi ABP, Bernardo LS, da Silva Neto GP, Davi RF, Barbara AFS, et al. Medical residents’ mental distress in the COVID-19 pandemic: an urgent need for mental health care. PLoS One. (2022) 17:e0266228.
53. Naldi A, Vallelonga F, Di Liberto A, Cavallo R, Agnesone M, Gonella M, et al. COVID-19 pandemic-related anxiety, distress and burnout: prevalence and associated factors in healthcare workers of North-West Italy. BJPsych Open. (2021) 7:e27. doi: 10.1192/bjo.2020.161
54. Faria AR, Coelho HFC, Silva AB, Damascena LCL, Carneiro RR, Lopes MT, et al. Impact of the COVID-19 pandemic on the development of burnout syndrome in frontline physicians: prevalence and associated factors. Rev Assoc Med Bras. (2021) 67:942–9. doi: 10.1590/1806-9282.20210244
55. Shiu C, Chen W-T, Hung C-C, Huang EP-C, Lee TS-H. COVID-19 stigma associates with burnout among healthcare providers: evidence from Taiwanese physicians and nurses. J Formosan Med Assoc. (2021) 09:09. doi: 10.1016/j.jfma.2021.09.022
56. Teo I, Sung SC, Cheung YB, Wong WHM, Abu Bakar Aloweni F, Ang HG, et al. Burnout, anxiety and depression in healthcare workers during the early COVID-19 period in Singapore. Singapore Med J. (2021) 10:07. doi: 10.11622/smedj.2021156
57. Torrente M, Sousa PAC, Sanchez-Ramos A, Pimentao J, Royuela A, Franco F, et al. To burn-out or not to burn-out: a cross-sectional study in healthcare professionals in Spain during COVID-19 pandemic. BMJ Open. (2021) 11:e044945. doi: 10.1136/bmjopen-2020-044945
58. Tuna T, Ozdin S. Levels and predictors of anxiety, depression, and burnout syndrome in physicians during the COVID-19 Pandemic. Int J Mental Health Addict. (2021) 19:2470–83. doi: 10.1007/s11469-021-00505-2
59. Turan C, Acar T, Acar BA, Unlubas Y, Erdogan R, Guzey Aras Y, et al. Specialist physicians battle against the COVID-19 pandemic: the relationship between specialist physicians working conditions and levels of burnout during the COVID-19 pandemic. Eur Rev Med Pharmacol Sci. (2022) 26:1403–13.
60. Enea V, Candel OS, Zancu SA, Scrumeda A, Barbuselu M, Largu AM, et al. Death anxiety and burnout in intensive care unit specialists facing the COVID-19 outbreak: the mediating role of obsession with COVID-19 and coronaphobia. Death Stud. (2021) 46:2306–15. doi: 10.1080/07481187.2021.1928331
61. Ibar C, Fortuna F, Gonzalez D, Jamardo J, Jacobsen D, Pugliese L, et al. Evaluation of stress, burnout and hair cortisol levels in health workers at a University Hospital during COVID-19 pandemic. Psychoneuroendocrinology. (2021) 128:105213. doi: 10.1016/j.psyneuen.2021.105213
62. Kapetanos K, Mazeri S, Constantinou D, Vavlitou A, Karaiskakis M, Kourouzidou D, et al. Exploring the factors associated with the mental health of frontline healthcare workers during the COVID-19 pandemic in Cyprus. PLoS One. (2021) 16:e0258475. doi: 10.1371/journal.pone.0258475
63. Karacan FA, Yilmaz S, Kirpinar I. Psychosocial adjustment of healthcare professionals during the COVID-19 pandemic: resident doctors, nurses, and caregivers need extra attention. Med J Bakirkoy. (2021) 17:375–85. doi: 10.4274/BMJ.galenos.2021.46338
64. Mousavi-Asl B, Firouzifar M, Noury L, Khamushian P, Mousavi-Asl D, Heidari F. Burnout among health care providers during covid-19 outbreak. Acta Med Iran. (2021) 59:108–12. doi: 10.18502/acta.v59i2.5577
65. Mutleq A, Alghazo M, Al-Faouri I, Alarsan S. Burnout among jordanian frontline physicians and nurses during covid-19 outbreak. N Armenian Med J. (2021) 15:64–8.
66. Stocchetti N, Segre G, Zanier ER, Zanetti M, Campi R, Scarpellini F, et al. Burnout in intensive care unit workers during the second wave of the covid-19 pandemic: a single center cross-sectional Italian study. Int J Environ Res Public Health. (2021) 18:6102. doi: 10.3390/ijerph18116102
67. Zakaria MI, Remeli R, Ahmad Shahamir MF, Md Yusuf MH, Azizah Ariffin MA, Noor Azhar AM. Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong J Emerg Med. (2021) 28:254–9. doi: 10.1177/1024907921989499
68. Zhang X, Wang J, Hao Y, Wu K, Jiao M, Liang L, et al. Prevalence and factors associated with burnout of frontline healthcare workers in fighting against the COVID-19 pandemic: evidence from China. Front Psychol. (2021) 12:680614. doi: 10.3389/fpsyg.2021.680614
69. Azoulay E, Pochard F, Reignier J, Argaud L, Bruneel F, Courbon P, et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest. (2021) 160:944–55. doi: 10.1016/j.chest.2021.05.023
70. Babamiri M, Bashirian S, Khazaei S, Sohrabi MS, Heidarimoghadam R, Mortezapoor A, et al. Burnout and mental health of COVID-19 frontline healthcare workers: results from an online survey. Iran J Psychiatry. (2022) 17:136–43. doi: 10.18502/ijps.v17i2.8903
71. Yilmaz Y, Erdogan A, Bahadir E. Fear, anxiety, burnout, and insomnia levels of healthcare workers during COVID-19 pandemic in Turkey. Psychiatr Danubina. (2021) 33(Suppl 13):350–6. doi: 10.22541/au.164864621.11164274/v1
72. Zhou T, Xu C, Wang C, Sha S, Wang Z, Zhou Y, et al. Burnout and well-being of healthcare workers in the post-pandemic period of COVID-19: a perspective from the job demands-resources model. BMC Health Serv Res. (2022) 22:284. doi: 10.1186/s12913-022-07608-z
73. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. (2020) 29:4321–30. doi: 10.1111/jocn.15469
74. Akova I, Kilic E, Ozdemir ME. Prevalence of burnout, depression, anxiety, stress, and hopelessness among healthcare workers in COVID-19 Pandemic in Turkey. Inquiry. (2022) 59:469580221079684. doi: 10.1177/00469580221079684
75. Mendonca VS, Steil A, Teixeira de Gois AF. COVID-19 pandemic in Sao Paulo: a quantitative study on clinical practice and mental health among medical residency specialties. Sao Paulo Med J. (2021) 139:489–95. doi: 10.1590/1516-3180.2021.0109.r1.27042021
76. Khan N, Palepu A, Dodek P, Salmon A, Leitch H, Ruzycki S, et al. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open. (2021) 11:e050380. doi: 10.1136/bmjopen-2021-050380
77. Doulougeri K, Georganta K, Montgomery A. “Diagnosing” burnout among healthcare professionals: can we find consensus? Cogent Med. (2016) 3:1. doi: 10.1080/2331205X.2016.1237605
78. Vagni M, Giostra V, Maiorano T, Santaniello G, Pajardi D. Personal accomplishment and hardiness in reducing emergency stress and burnout among COVID-19 emergency workers. Sustainability. (2020) 12:9071. doi: 10.3390/su12219071
79. Buselli R, Corsi M, Veltri A, Baldanzi S, Chiumiento M, Lupo ED, et al. Mental health of Health Care Workers (HCWs): a review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry Res. (2021) 299:113847. doi: 10.1016/j.psychres.2021.113847
80. Khoo EA-O, Lantos JA-O. Lessons learned from the COVID-19 pandemic. Acta Paediatr. (2020) 109:1323–5. doi: 10.1111/apa.15307
81. Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJG. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. (2020) 75:102289. doi: 10.1016/j.janxdis.2020.102289
82. Al-Otaibi T, Abbas A, Nagib AM, Gheith OA, Nair P, Farid MM, et al. COVID-somnia: anxiety, insomnia, and poor sleep among second-line healthcare workers during COVID-19 pandemic. Egypt J Bronchol. (2022) 16:47. doi: 10.1186/s43168-022-00143-9
83. Melnikow J, Padovani A, Miller M. Frontline physician burnout during the COVID-19 pandemic: national survey findings. BMC Health Serv Res. (2022) 22:365. doi: 10.1186/s12913-022-07728-6
84. Karagöl A, Törenli Kaya Z. Healthcare workers’ burn-out, hopelessness, fear of COVID-19 and perceived social support levels. Eur J Psychiatry. (2022) 36:200–6. doi: 10.1016/j.ejpsy.2022.01.001
85. Chemali ZA-O, Ezzeddine FL, Gelaye B, Dossett ML, Salameh J, Bizri M, et al. Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Public Health. (2019) 19:1337. doi: 10.1186/s12889-019-7713-1
86. Abdo SAM, El-Sallamy RM, Elsherbini A, Kabbash I. Burnout among physicians and nursing staff working in the emergency hospital of Tanta University, Egypt. Eastern Mediterran Health J. (2016) 21:906–15. doi: 10.26719/2015.21.12.906
87. Siebens K, Casterlé BD, Abraham I, Dierckx K, Braes T, Darras E, et al. The professional self-image of nurses in Belgian hospitals: a cross-sectional questionnaire survey. Int J Nurs Stud. (2006) 43:71–82. doi: 10.1016/j.ijnurstu.2005.04.004
88. Kunz M, Strasser M, Hasan A. Impact of the coronavirus disease 2019 pandemic on healthcare workers: systematic comparison between nurses and medical doctors. Curr Opin Psychiatry. (2021) 34:413–9. doi: 10.1097/YCO.0000000000000721
89. Vandenbroeck S, Van Gerven E, De Witte H, Vanhaecht K, Godderis L. Burnout in Belgian physicians and nurses. Occupat Med. (2017) 67:546–54. doi: 10.1093/occmed/kqx126
90. Boumans NPG, De Jong AHJ, Vanderlinden L. Determinants of early retirement intentions among Belgian nurses. J Adv Nurs. (2008) 63:64–74. doi: 10.1111/j.1365-2648.2008.04651.x
91. Vitale E, Galatola V, Mea R. Exploring within and between gender differences in burnout levels in Italian nurses engaged in the Covid-19 health emergency: a cohort observational study. Mine Psichiatr. (2020) 61:162–70. doi: 10.23736/S0391-1772.20.02090-7
92. França SPDS, De Martino MMF, Aniceto EVDS, Silva LL. Predictors of burnout syndrome in nurses in the prehospital emergency services. Acta Paul Enfermagem. (2012) 25:68–73. doi: 10.1590/S0103-21002012000100012
93. Corlade-Andrei M, Mãirean C, Nedelea P, Grigoraşi G, Cimpoeşu D. Burnout syndrome among staff at an emergency department during the COVID-19 Pandemic. Healthcare. (2022) 10:258. doi: 10.3390/healthcare10020258
94. Aryankhesal A, Mohammadibakhsh R, Hamidi Y, Alidoost S, Behzadifar M, Sohrabi R, et al. Interventions on reducing burnout in physicians and nurses: a systematic review. Med J Islam Repub Iran. (2019) 33:77. doi: 10.47176/mjiri.33.77
95. Ziaei M, Yarmohammadi H, Karamimatin B, Yarmohammadi S, Nazari Z, Gharagozlou F. Prevalence and risk factors of occupational burnout among nurses of a hospital in Kermanshah in 2013. Iran-J-Ergon. (2014) 2:67–74.
96. Chaka EE, Mekuria M, Melesie G. Access to essential personal safety, availability of personal protective equipment and perception of healthcare workers during the COVID-19 in Public Hospital in West Shoa. Infect Drug Resist. (2022) 15:2315. doi: 10.2147/IDR.S344763
97. El-Sokkary RH, Khater WS, El-Kholy A, Mohy Eldin S, Gad DM, Bahgat S, et al. Compliance of healthcare workers to the proper use of personal protective equipment during the first wave of COVID-19 pandemic. J Infect Public Health. (2021) 14:1404–10. doi: 10.1016/j.jiph.2021.07.017
98. Murthy VH. Confronting health worker burnout and well-being. N Engl J Med. (2022) 387:577–9. doi: 10.1056/NEJMp2207252
99. Bazan D, Nowicki M, Rzymski P. Medical students as the volunteer workforce during the COVID-19 pandemic: polish experience. Int J Disaster Risk Reduct. (2021) 55:102109. doi: 10.1016/j.ijdrr.2021.102109
100. Almulhem JA, Aldekhyyel RN, Binkheder SA-OX, Temsah MA-O, Jamal AA-O. Stress and burnout related to electronic health record use among healthcare providers during the COVID-19 Pandemic in Saudi Arabia: a Preliminary National Randomized Survey. Healthcare. (2021) 9:1367. doi: 10.3390/healthcare9101367
Keywords: burnout, healthcare workers, COVID-19, systematic review, meta-analysis, physicians
Citation: Macaron MM, Segun-Omosehin OA, Matar RH, Beran A, Nakanishi H, Than CA and Abulseoud OA (2023) A systematic review and meta analysis on burnout in physicians during the COVID-19 pandemic: A hidden healthcare crisis. Front. Psychiatry 13:1071397. doi: 10.3389/fpsyt.2022.1071397
Received: 16 October 2022; Accepted: 28 December 2022;
Published: 12 January 2023.
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Muna Ahmead, Al-Quds University, PalestineNkereuwem Ebiti, Federal Neuropsychiatric Hospital Kaduna, Nigeria
Copyright © 2023 Macaron, Segun-Omosehin, Matar, Beran, Nakanishi, Than and Abulseoud. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Osama A. Abulseoud,  Abulseoud.osama@Mayo.edu
Abulseoud.osama@Mayo.edu
†These authors have contributed equally to this work
 Marie Michele Macaron
Marie Michele Macaron Omotayo Ayomide Segun-Omosehin
Omotayo Ayomide Segun-Omosehin Reem H. Matar
Reem H. Matar Azizullah Beran4
Azizullah Beran4 Osama A. Abulseoud
Osama A. Abulseoud