Working with patients and the mental health of health care workers during the COVID-19 pandemic
Abstract
BACKGROUND:
Anxiety and concern are among the most common problems facing healthcare workers (HCWs) during epidemic diseases.
OBJECTIVE:
To identify the predictive factors of anxiety, fears, and psychological distress among healthcare workers during the COVID-19 pandemic.
METHODS:
An online survey method was used on a sample of 153 of HCWs; (110) frontline and (43) non-frontline HCWs. They answered on the Hamilton anxiety rating scale, the Kessler psychological distress scale (K10), and the COVID-19 Concerns Questionnaire.
RESULTS:
The results demonstrated that 47.05% of HCWs have a severe level of fear related to COVID-19, 43.13% have very severe anxiety, and 30.71% experience severe psychological distress. The differences between frontline and non-frontline HCWs, female and male HCWs, and HCWs working in medical clinics, on quarantine, or in another place were significant in the three scales. Predictive factors of anxiety, fear, and psychological distress include working on the front lines, being female, and being over 50 years old. Meanwhile, working in a workplace with COVID-19 patients predicted anxiety and psychological distress, but not fears associated with COVID-19.
CONCLUSION:
HCWs have a high prevalence of symptoms of mental disorders that may interfere with their work. These results may have therapeutic applications during pandemics.
1Introduction
Coronavirus (COVID-19) was discovered in December 2019 in Wuhan, and the virus has spread in most countries of the world. Since then, the number of cases has gradually increased, requiring the participation of a number of health practitioners in screening, detection of the injured, and the provision of health care for detainees. Meanwhile, with the widespread use of social media for spreading news, the psychological effects of COVID-19 have become more rapid and impacting, and may cause a real disaster even after the virus has ended, due to stress and psychological distress resulting from this pandemic [1–3]. It is expected that reactions to COVID-19 will increase due to the daily increasing number of injuries and deaths, which means that long-term mental health assessments might be necessary during and after the pandemic [4, 5].
Medical workers are taking on many burdens during the outbreak of COVID-19, which exposes them to severe stress due to the long hours they spend with patients [6–8]. They are subject to many psychological problems such as anxiety, stress, tension, depressive symptoms, PTSD, and psychological distress. During this pandemic, they suffered from many problems, including the large increase of daily infections and deaths, the lack of real information about COVID-19, the fear of transmission of infection to them or their families and friends, the fear of the failure of the medical care they provide to patients, the scarcity of resources, and the weak health infrastructure in many countries [1, 7]. Reports have shown that medical personnel involved in treating people with COVID-19 are at a higher risk of transmission, and because of this high risk, they suffer from mental health disorders, which impairs their ability to continue dealing with COVID-19 [1, 9, 10]. Therefore, anxiety, stress, tension, and fear are among the most common symptoms of mental health disorders among HCWs during epidemic diseases [11–13]. This means that there is a need for mental health care during an outbreak of COVID-19 [9, 10, 14].
Fadhel [6] stated that the frontline HCWs of the COVID-19 pandemic are in urgent need of psychological intervention programs that help them face the psychological and social crises resulting from COVID-19, especially in light of the severe shortage of psychiatrists and psychotherapists qualified to assist in these circumstances.
In this regard, studies examined medical personnel in the first wave of COVID-19 and found increases in anxiety, depressive symptoms, psychological distress, insomnia or poor sleep quality, and overall psychological problems [15–22]. Feingold and colleagues [23] found that, seven months following the first wave of COVID-19, 77% of frontline HCWs reported pandemic-related posttraumatic growth with greater severity of PTSD symptoms. Those with severe PTSD symptoms in the first wave were more likely to endorse most aspects of posttraumatic growth during the second wave.
The pooled prevalence rates were higher for anxiety and depression among medical staff—33% and 28%, respectively—and were similar to prevalence rates in the general population [24]. Meanwhile, another meta-analysis study reported that pooled prevalence rates for anxiety, depression, and insomnia were less than these results [25]. Xiao et al. [26] found that 55.1% of medical personnel had psychological stress, while 54.2% and 58% had symptoms of anxiety and depression, respectively. These prevalence rates decreased to 8.7% for anxiety, 5.3% for depression, 3.8% for psychological distress, and 2.2% for stress [27].
The researchers found a high prevalence of anxiety and tension among HCWs before the spread of COVID-19 in their country. The most common concern was about infecting family and friends rather than infecting oneself [28]. It was found that rural living, female gender, and contact with COVID-19 patients were the most common risk factors associated with anxiety, insomnia, obsessive-compulsive symptoms, and depression among HCWs [29]. The levels of hopelessness and anxiety were higher in HCWs than they were in non-HCWs, the level of hopelessness in nurses was higher than it was in doctors, and state anxiety was higher in nurses than it was in doctors or HCWs [30].
Psychological symptoms were common among HCWs in New York, with 57% of participants experiencing acute stress, 48% depression, and 33% symptoms of anxiety. The rates of this mental distress were higher in nurses and advanced training providers compared to attending physicians [31]. Kang et al. [12] indicated that health personnel in Wuhan during the COVID-19 outbreak suffered from isolation, excessive workload, and discrimination, and that they were more likely to suffer from fatigue, fear, sleep problems, and emotional disorders. While 50.7% of HCWs have depressive symptoms, over 44% have anxiety and 36% experience sleep problems [13].
Conversely, researchers found a significant decrease in symptoms of depression and anxiety among nurses and health care technicians during the second wave as compared to the first wave. During the first wave, 68% of respondents had anxiety and 49.6% had depression. This decreased in the second wave to 49.5% for anxiety and 35% for depression [32].
Unexpectedly, several studies found higher prevalence rates of mental disorders among HCWs during the second wave of COVID-19 than during the first wave. In a comparative study on mental health among frontline HCWs in the first and second waves of COVID-19, researchers found an increase in the prevalence of depression, anxiety, and post-traumatic stress disorder during the second wave [33].
Levels of exhaustion, disengagement, and burnout among HCWs were higher in the second lockdown than they were in the first lockdown [34]. Azoulay and colleagues [35] found high prevalence rates of symptoms of anxiety, burnout, depression, and post-traumatic stress disorder among HCWs. The variables of sex, profession, personality characteristics, and fear associated with COVID-19 were predictive of mental health symptoms [35]. The prevalence of mental disorders among HCWs was high at the end of the pandemic in China [36].
Accordingly, we believe that the mental health of HCWs working during the COVID-19 pandemic has not been adequately evaluated in Saudi Arabia and the Middle East. This study starts from the main hypothesis that frontline HCWs have higher levels of fears, anxiety, and psychological distress compared to non-frontline HCWs. Also, frontline work may be a high-risk predictor of mental health impairment in HCWs.
Consequently, this study aims to assess fears, anxiety, and psychological distress among HCWs working with people infected with COVID-19 in Saudi Arabia and to explore the predictive factors of these disorders using pathway analysis.
2Methods
2.1Sample
The current research community consists of healthcare workers during the COVID-19 pandemic in Saudi Arabia. According to the Saudi Ministry of Health, nearly 100,000 HCWs participated in the response to the COVID-19 pandemic [37].
Eligible individuals were age 20 years and above, working in a hospital or medical center that receives COVID-19 patients, fluent in Arabic language, and resided in the Saudi Arabia.
Out of 13 regions, 3 regions (23.76%) were selected, including Riyadh, Makkah Al-Mukarramah, and Asir region. These regions were chosen based on two criteria: the high prevalence rates of COVID-19 and the number of new cases of COVID-19 during the past week. At this time (August 4, 2020), the provinces of Riyadh and Makkah were at the forefront of regions in terms of prevalence rate and cases reported daily, while Asir was among the regions in which daily infection rates were remarkably high.
In these three regions, we randomly selected a number of quarantine clinics and hospitals that receive patients with COVID-19, including three hospitals in three cities follow the Riyadh region, namely, Dallah Hospital in the capital, Riyadh (22.88% N = 35), Lutein Medical Center in Zulfi (13.73% N = 21), and King Khalid Hospital in Al Majmaah (9.80% N = 15), in addition to Mansour Medical Center in Jeddah in the Mecca region (27.45% N = 42) and Asir Hospital in Abha in the Asir region (26.14% N = 40).
Accordingly, a random sample consisting of (153) HCWs was selected: (110) frontline HCWs and (43) non-frontline HCWs.
2.2Measures
2.2.1Hamilton Anxiety Rating Scale (HARS)
The scale consists of 14 items that measure the symptoms of anxiety. The total score ranges between 0–56, where < 17 indicates mild severity, 18–24 moderate severity, 25–30 severe, and 31 or over very severe [38, 39]. It is a validated scale and is still widely used in research settings and clinical practice.
2.2.2Kessler Psychological Distress Scale (K10, KPDS)
This measures psychological distress through 10 questions about anxiety and depressive symptoms that appeared in the last 30 days. Scoring is based on a 1–5 Likert scale (None, A little of the time, Some of the time, Most of the time, All of the time). Scores range from 10 to 50. A score under 20 indicates normal; 20–24 indicates mild mental disorder, 25–29 indicates moderate mental disorder, and 30 or over indicates a severe mental disorder [40, 41].
2.2.3COVID-19 Concerns Questionnaire (CCQ)
This is a 12-item questionnaire prepared by researchers to measure fears, tension, and anxiety associated with COVID-19. Scoring is based on a 5-point Likert scale (None, A little of the time, Some of the time, Most of the time, All of the time). The total scores range from 0 to 48; scores between 0–12 are likely to be well, 13–24 mild, 25–36 moderate, and 37 or over severe.
The HARS and KPDS were translated into Arabic by the researchers; it was then reverse translated into English. The proportions of consistency were good. The reliability and validity of the tools were also calculated in the current study, and shown in the results section.
2.3Procedures
In line with the precautionary measures and to prevent the spread of COVID-19 through contact, an online survey was conducted on a sample of HCWs. Participants answered an online version of the questionnaires anonymously from 4 August 2020 to 16 August 2020. All participants provided their demographic data and answered three questionnaires that assessed their concerns related to COVID-19 (fears), anxiety, and psychological distress.
The respondents were informed that participation was voluntary, and they provided informed consent online.
The statistical analysis evaluated the effect of independent variables on anxiety, psychological distress, and fears of COVID-19. The independent variables included working with COVID-19 patients, specialization (consultant physician, nursing staff, supportive staff, and administrative staff), sex, age, and educational level. The pathway analysis method was used to identify the most predictive factors of anxiety, psychological distress, and fears of COVID-19 among HCWs.
Path analysis is a type of multiple regression analysis, which is used to evaluate causal models by examining the relationships between a dependent variable and two or more independent variables. Using this method, researchers can estimate the magnitude and importance of causal links between variables, and identify predictive factors, according to the hypothesis that researchers have previously established.
3Results
3.1Demographic characteristics of participants
Table 1 shows the demographic characteristics of the research sample.
Table 1
Demographic characteristics of the participants
| Sex | Male | Female | |||
| Frequency | 101 | 52 | |||
| Percent (%) | 66 | 33.99 | |||
| Age | 20-30 | 31-40 | 41-50 | 51-60 | More than 60 |
| Frequency | 28 | 41 | 46 | 38 | 0 |
| Percent (%) | 18.3 | 26.8 | 30.1 | 24.8 | 0 |
| Education | Diploma | Bachelor | Board | MD | PhD |
| Frequency | 30 | 81 | 12 | 18 | 12 |
| Percent (%) | 19.6 | 52.9 | 7.8 | 11.8 | 7.8 |
| Social status | Single | Married | Divorced/widow | ||
| Frequency | 32 | 108 | 13 | ||
| Percent (%) | 20.9 | 70.6 | 8.5 | ||
| Specialization | Doctors | Nursing staff | Supportive staff | Administrative staff | |
| Frequency | 55 | 27 | 58 | 13 | |
| Percent (%) | 35.94 | 17.65 | 37.91 | 8.5 | |
| Working with COVID-19 patients | Non-frontline HCWs | Frontline HCWs | |||
| Frequency | 43 | 110 | |||
| Percent (%) | 28.1 | 71.9 | |||
| Working in a workplace with COVID-19 patients | Quarantine | Medical clinics | Other | ||
| Frequency | 31 | 56 | 66 | ||
| Percent (%) | 20.3 | 36.6 | 43.1 |
3.2Psychometric properties of the study tools
The Hamilton Anxiety Rating Scale is a validated scale. In our study, good reliability was achieved; it was (0.979) in Cronbach’s alpha and (0.898) in the split-half reliability (the Spearman-Brown Coefficient was 0.949). The internal consistency was good; the correlation ranged between 0.834 and 0.923 and was significant at the 0.01 level. The Kessler Scale of Psychiatric Disorder has good psychometric properties and is used internationally. In the current study, we have found good reliability (0.969) in Cronbach’s alpha and (0.884) in the split-half (the Spearman-Brown Coefficient was 0.938). The internal consistency also was good and the correlation ranged between 0.839 and 0.925 with significance at the 0.01 level.
The COVID-19 Concerns Questionnaire has good reliability and validity; it was (0.926) in Cronbach’s alpha and (0.915) in the split-half reliability (the Spearman-Brown Coefficient was 0.955). The internal consistency was calculated by a correlation between the item score and the overall score of the questionnaire. The correlation ranged between 0.558 and 0.884 with significance at the 0.01 level.
The Exploratory Factor Analysis was used in the COVID-19 Concerns Questionnaire and produced one factor that explained (55.728%) of the total variance, and the items load ranged from 0.573 to 0.884.
3.3Level of anxiety, psychological distress, and concerns related to COVID-19 in frontline and non-frontline HCWs
The results of this study showed that 41.83% (24.84% N = 38 Frontline HCWs, and 16.99% N = 26 Non-Frontline HCWs) have a mild severity of anxiety. A total of 9.80% (3.27% N = 5 Frontline HCWs, and 6.53% N = 10 Non-Frontline HCWs) have a moderate level of anxiety, 5.23% (3.27% N = 5 Frontline HCWs, and 1.96% N = 3 Non-Frontline HCWs) have severe anxiety, and 43.13% (40.52% N = 62 Frontline HCWs, and 2.61% N = 4 Non-Frontline HCWs) have very severe anxiety.
Our results showed that 53.59% N = 82 (28.75% N = 44 Frontline HCWs, and 24.84% N = 38 Non-Frontline HCWs) are likely to be well. A total of 7.84% N = 12 (6.54% N = 10 Frontline HCWs, and 1.30% N = 2 Non-Frontline HCWs) have mild psychological distress, 7.84% N = 12 (7.19% N = 11 Frontline HCWs, and 0.65% N = 1 Non-Frontline HCWs) have moderate psychological distress, and 30.71% N = 47 (29.41% N = 45 Frontline HCWs, and 1.30% N = 2 Non-Frontline HCWs) have severe psychological distress.
Meanwhile, 2.60% N = 4 (1.3% N = 2 Frontline HCWs, and 1.3% N = 2 Non-Frontline HCWs) appear to have no fears related to COVID-19. A total of 24.18% N = 37 (10.46% N = 16 Frontline HCWs, and 13.72% N = 21 Non-Frontline HCWs) have a mild level of fears, 26.14% N = 40 (15.69% N = 24 Frontline HCWs, and 10.45% N = 16 Non-Frontline HCWs) have a moderate level of fears, and 47.05% N = 72 (44.44% N = 68 Frontline HCWs, and 2.61% N = 4 Non-Frontline HCWs) have severe levels of concerns related to COVID-19.
3.4Differences in anxiety, psychological distress, and concerns related to COVID-19 between frontline and non-frontline HCWs, and between male and female
The independent sample t test was used as shown in Table 2. There are significant differences in all scales between HCWs who work or do not work with COVID-19 patients. The differences between male and female HCWs are significant in all three scales. Females appeared more fearful, anxious, and distressed than males.
Table 2
Differences between frontline and non-frontline HCWs
| Measurements | Working with COVID-19 Patients | N | Mean | SD | t | Sig. (2-tailed) |
| Anxiety | Yes | 110 | 29.7818 | 19.30555 | 4.726 | 0.000 |
| No | 43 | 14.9535 | 11.27567 | |||
| Psychological distress | Yes | 110 | 21.5727 | 13.15083 | 5.010 | 0.000 |
| No | 43 | 10.8140 | 7.97990 | |||
| Fears of COVID | Yes | 110 | 35.6545 | 10.43234 | 5.864 | 0.000 |
| No | 43 | 24.9070 | 9.53393 | |||
| Measurements | Gender | N | Mean | SD | t | Sig0. (2-tailed) |
| Anxiety | Male | 101 | 21.1683 | 18.53271 | 4.349 | 0.000 |
| Female | 52 | 34.2500 | 15.68173 | |||
| Psychological distress | Male | 101 | 15.3168 | 12.99071 | 4.616 | 0.000 |
| Female | 52 | 24.8269 | 10.02296 | |||
| Fears of COVID | Male | 101 | 30.9307 | 11.19576 | 2.661 | 0.009 |
| Female | 52 | 35.9423 | 10.71450 |
3.5Differences between HCWs in anxiety, psychological distress, and concerns related to COVID-19 according to workplace with COVID-19 patients
One-way ANOVA showed significant differences between HCWs depending on where they work with COVID-19 patients, as shown in Table 3. There are significant differences between HCWs in all scales due to where they work with COVID-19 patients. The Scheffe test was used to determine the direction of these differences (see results in Table 4). As per Table 4, workers in the medical clinic with COVID-19 patients have more fears, anxiety, and psychological distress than workers in quarantine or in other locations. In this case, the differences were statistically significant.
Table 3
Differences between HCWs according to workplace with COVID-19 patients
| Measurements | Sum of squares | df | Mean square | F | Sig. | |
| Anxiety | Between groups | 17953.235 | 2 | 8976.617 | 38.682 | 0.000 |
| Within groups | 34809.013 | 150 | 232.060 | |||
| Total | 52762.248 | 152 | 49.505 | 0.000 | ||
| Psychological distress | Between groups | 9981.615 | 2 | 4990.808 | ||
| Within groups | 15122.267 | 150 | 100.815 | |||
| Total | 25103.882 | 152 | ||||
| Fears of COVID | Between groups | 4742.348 | 2 | 2371.174 | 24.514 | 0.000 |
| Within groups | 14509.156 | 150 | 96.728 | |||
| Total | 19251.503 | 152 |
Table 4
Multiple comparisons of differences according to workplace with COVID-19 patients
| Dependent variable | (I) Participation with patients COVID-19 | (J) Participation with patients COVID-19 | Mean difference (I-J) | Std. error | Sig. | 95% Confidence interval | |
| Lower bound | Upper bound | ||||||
| Fears of COVID | Quarantine | Other | 9.40860* | 2.14145 | 0.000 | 4.1141 | 14.7031 |
| Medical clinics | Other | 12.00595* | 1.78686 | 0.000 | 7.5881 | 16.4238 | |
| Anxiety | Quarantine | Medical clinics | –10.43664-* | 3.41024 | 0.011 | –18.8681- | –2.0052- |
| Other | 13.78739* | 3.31691 | 0.000 | 5.5867 | 21.9881 | ||
| Medical clinics | Other | 24.22403* | 2.76767 | 0.000 | 17.3813 | 31.0668 | |
| Psychological distress | Quarantine | Medical clinics | –8.83813-* | 2.24775 | 0.001 | –14.3955- | –3.2808- |
| Other | 9.29228* | 2.18623 | 0.000 | 3.8871 | 14.6975 | ||
| Medical clinics | Other | 18.13041* | 1.82422 | 0.000 | 13.6202 | 22.6406 | |
*The mean difference is significant at the 0.05 level.
3.6Results of path analysis
The path analysis method was used to reveal the most predictive factors of anxiety, psychological distress, and fears related to COVID-19 among HCWs. The researchers proposed the path analysis model as shown in Fig. 1. The path analysis model resulted in many goodness-of-fit indicators (see Table 5), showing the validity of the proposed theoretical path analysis model through the goodness-of-fit indicators. Therefore, we can predict fears, anxiety, and distress among HCWs from these factors. CMIN/DF is (1.162), RMSEA, with the value of 0.03 less than 0.1 and the NFI of 0.977, the RFI of 0.925, the IFI of 0.997, the TLI of 0.989, and the CFI of 0.997, the default model for the AIC (default model: 118.272), the default model—the Brown-Cudeck BCC (default model: 126.299), and the default cross—Expected ECVI (default model: 0.778), far surpassed its independent models, which are equal to 738.163, 741.283, and 4.856, respectively. All of these indicators increase the availability of the measurement model on a fit. These results are shown in Fig. 2 and Table 6.
Fig. 1
The proposed path analysis model to predict fears, anxiety, and psychological distress among HCWs.
Table 5
Fit indices of the hypothesized path analysis model
| Indicators | Psychological services empowerment | |||
| Cn | 1.162 | |||
| GFI | 0.97 | |||
| RAMSEA | 0.03 | |||
| NFI | 0.977 | |||
| RFI | 0.925 | |||
| IFI | 0.997 | |||
| CFI | 0.997 | |||
| AIC | Model | Value | ||
| Default | 118.272 | |||
| Independence | 738.163 | |||
| BCC | Model | Value | ||
| Default | 126.299 | |||
| Independence | 741.283 | |||
Fig. 2
Standard path parameters of the default path analysis to predict fears, anxiety, and psychological distress among HCWs.
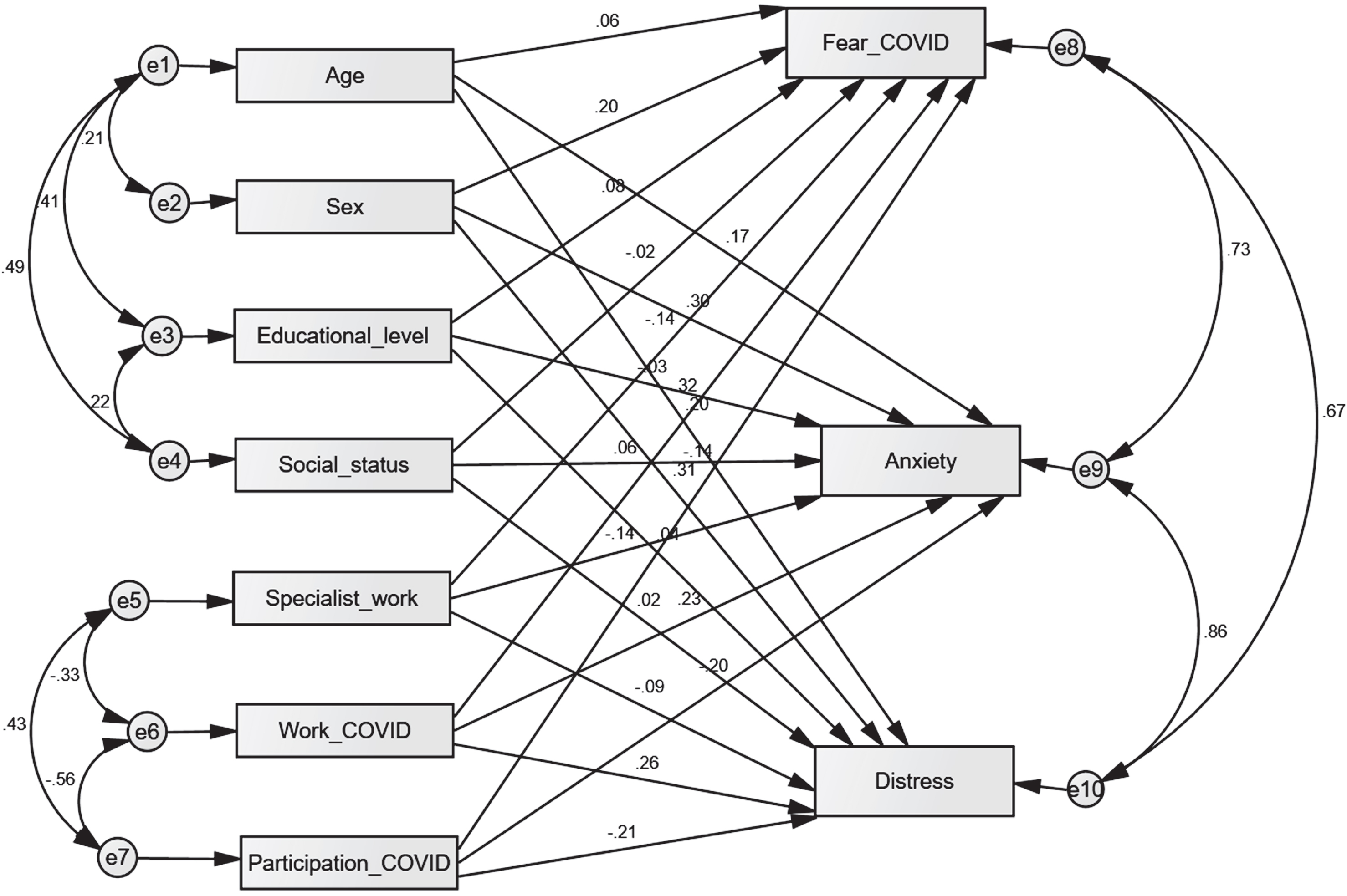
Table 6
Regression weights: (Group number 1 –Default model)
| Dependent variable | Independent variable | C.R. | Pa |
| Anxiety | Social status | 0.816 | 0.414 |
| Psychological distress | Specialty | –1.289 | 0.197 |
| Fears of COVID-19 | Working with COVID-19 patients | –1.635 | 0.102 |
| Fears of COVID-19 | Work with COVID-19 patients | 3.927 | 0.00** |
| Fears of COVID-19 | Specialty | –1.783 | 0.075 |
| Fears of COVID-19 | Social status | –0.274 | 0.784 |
| Fears of COVID-19 | Educational level | 1.107 | 0.268 |
| Fears of COVID-19 | Sex | 2.792 | 0.005* |
| Anxiety | Age | 2.083 | 0.037* |
| Anxiety | Working with COVID-19 patients | –2.457 | 0.014* |
| Anxiety | Work with COVID-19 patients | 2.931 | 0.003* |
| Anxiety | Educational level | –0.470 | 0.638 |
| Anxiety | Specialty | –1.985 | 0.047* |
| Psychological distress | Work with COVID-19 patients | 3.394 | 0.00** |
| Psychological distress | Educational level | 0.501 | 0.616 |
| Psychological distress | Social status | 0.330 | 0.742 |
| Fears of COVID | Age | 0.685 | 0.493 |
| Anxiety | Sex | 4.508 | 0.00** |
| Psychological distress | Sex | 4.733 | 0.00** |
| Psychological distress | Age | 2.425 | 0.015* |
| Psychological distress | Working with COVID-19 patients | –2.594 | 0.009* |
a *, p < 0.05, **, p < 0.01.
4Discussion
This study sought to assess concerns, anxiety, and psychological distress among frontline and non-frontline HCWs in the COVID-19 pandemic and to reveal the factors that predict these mental symptoms using the pathway analysis method.
Our results found high levels of fears, anxiety, and psychological distress among HCWs. The HCWs on the frontlines suffered more from mental health symptoms than did non-frontline HCWs, and the differences between the two groups were significant. We find that these results are reasonable, given the amount of stress to which frontline workers are exposed.
This is also due to the media momentum that accompanied the spread of the COVID-19 and cemented in the minds of many people that the disease is transmitted quickly through contact with infected patients, via droplets, shaking hands, or touching surfaces and tools contaminated with COVID-19.
Many media outlets, news sites, newspapers, social media, and even scientific and research centers in the world, including those of the World Health Organization, have intensified the publication of warnings and preventive instructions to limit the spread of the virus. However, the news that accompanied these warnings about methods of transmitting the infection, the number of daily infections in every country, and the most affected groups have caused many doctors and health professionals to approach cases with extreme caution and thereby suffer from anxiety, tension, psychological distress, and the fear of being infected due to their work with COVID-19 patients.
Therefore, it has been found that knowing a person with the disease increases health workers’ fears, anxiety, and mental disorders [33]. In this regard, it was found that more than half of healthcare workers were afraid of being infected with COVID-19 and that 80.4% of them believed that there was a very high probability of infection [8]. During the Corona pandemic, Que et al. [20] found high prevalence rates for symptoms of anxiety, depression, insomnia, and overall psychological problems in HCWs. About one-third of resident physicians had higher levels of stress at work [42].
HCWs who participate on the frontline had a higher risk of mental health problems compared to HCWs who did not participate in frontline work. Frontline medical personnel showed higher scores on the scale of fears, anxiety, and depression compared to non-frontline workers [43]. Our results are consistent with those of many studies that found high rates of psychological symptoms among first-line workers during the COVID-19 pandemic [e.g., 9, 16, 18, 19, 20, 25, 28, 44, 45].
However, some studies have found low prevalence rates of fears, anxiety, and other psychological symptoms such as depressed mood and insomnia among HCWs [22, 24–28, 33, 40]. It was also found that the vicarious traumatization scores in the frontline nurse were lower than those of non-frontline nurses [46].
The results of the current study revealed significant differences between male and female HCWs in all three scales. Females appeared more fearful, anxious, and psychologically distressed than males. According to Hacimusalar and his colleagues [30], the prevalence of anxiety was higher among females and among those in close contact with a high-risk COVID-19 patient.
The results of the present study indicated that age is a statistically significant predictor of anxiety and psychological distress but not of fears of COVID-19. Sex is a statistically significant predictor of anxiety, fears of COVID-19, and psychological distress. Education level and social status are not significant predictors of anxiety, fears of COVID-19, or psychological distress. Specialization is not a significant predictor of fears of COVID-19 or psychological distress but is a significant predictor of anxiety. Working on the frontline is a significant predictor of fears of COVID-19, anxiety, and psychological distress. A workplace with COVID-19 patients is a significant predictor of anxiety and psychological distress but not fears of COVID-19.
Working on the frontline of the COVID-19 pandemic includes a lot of daily stress and anxiety, in addition to fear of transmitting the infection to a person or his/her family and friends. The COVID-19 pandemic has imposed much psychological distress and stress on all members of society; frontline HCWs bear the greatest burden in combating this pandemic, limiting its spread, and treating patients. Long shifts are imposed on them in clinics or quarantine centers, with severe restrictions on their movement. Also, strict preventive measures were imposed on them. Some of them spend a long time in the workplace. All these circumstances and other conditions are related to work requirements, e.g., the lack of professionals or participation on the frontlines, the lack of health tools for the prevention and treatment of disease (such as breathing apparatuses and medicines needed to alleviate the suffering of patients), the increasing daily numbers of patients in the hospitals (possibly resulting in the hospital going over its capacity), and the lack of a vaccine or effective treatment. All this has imposed on frontline HCWs more anxiety, fear, tension, and stress. In line with these increasing stresses, the woman-doctor found herself faced with increasing concerns about her work on the frontlines of COVID-19 and the dispersion of her interests in the home and family. Most of the requirements for working with COVID-19 were also completely new, and there was not enough information about the epidemic, with severe restrictions imposed on freedom of movement. Perhaps the female-doctor suffers more from these conditions.
Consistent with these findings, Spoorthy et al. [47] point out that demographic variables, including sex, profession, age, workplace, department, and psychological variables, including poor social support and self-efficacy, were associated with increased anxiety, stress, insomnia, and depressive symptoms in health care providers. In another study, common risk factors included being female, being a nurse, belonging to a lower socioeconomic status, having a high probability of contacting a COVID-19 patient, and social isolation [24]. High prevalence rates of depression, anxiety, loneliness, and sleep disturbance were reported among healthcare professionals in Bangladesh. These disorders were associated with many factors including gender differences, educational level, region of residence, marital status, and occupational category [48, 49].
Meanwhile, being female, engaging in avoidance strategies, seeking social support, and working on the frontlines with COVID-19 patients were risk factors affecting the mental health of healthcare professionals [47]. Zhang and his colleagues [29] found that female gender, rural living, and contact with COVID-19 patients were the most common risk factors of anxiety and other psychological symptoms.
According to the results of this study, working on the frontline, being female, and being over 50 years old are the predicted factors of fears, anxiety, and psychological distress. While working in a workplace with COVID-19 patients predicts anxiety and psychological distress, it does not predict concerns about COVID-19.
5Conclusions
We found a high prevalence of anxiety, fears, and psychological distress among HCWs during the COVID-19 epidemic, with significant differences between frontline and non-frontline HCWs in all three scales. Over one-third of frontline HCWs have very severe anxiety, one-third have severe psychological distress, and just less than half have a severe level of concerns related to COVID-19.
Frontline HCWs, females, and those over 50 years old of age seem to have more severe fears, anxiety, and psychological distress than non-frontline workers, males, or younger people. Therefore, the most predictive factors of mental health of HCWs were working with COVID-19 patients, age, and female gender. These factors may play an important role in mental health of HCWs and should be included in psychological intervention plans. Therefore, psychological interventions targeting frontline HCWs are urgent.
6Limitations
There are several limitations in this study. First, it relied on a cross-sectional assessment and used self-report measures. Second, the survey was conducted via the Internet, but use of this measure was to be expected due to the total lockdown in the country, and increased restrictions on contact with HCWs with COVID-19 patients to prevent further spread of the virus. Because of these restrictions, the sample size was relatively small. However, the participants constitute an adequate representation of the healthcare worker community in Saudi Arabia who have been involved in responding to the COVID-19 pandemic. The strengths of this study are that it used scales with good psychometric properties, it used the path analysis method, which is a more accurate statistical method for detecting predictive factors, and it revealed interesting results.
Acknowledgments
The authors are grateful to Professor Dr. Kay M. Mach for proofreading and editing this article.
Conflict of interest
The researchers declare that there is no conflict of interest.
Data availability
Data are available from the corresponding author upon reasonable request.
Funding
This research did not receive grants from any funding agency in the public, commercial or not-for-profit sectors.
References
[1] | Zhu Y , Chen L , Ji H , Xi M , Fang Y , Li Y . The Risk and Prevention ofNovel Coronavirus Pneumonia InfectionsAmong Inpatients in Psychiatric Hospitals. Neuroscience. Bulletin. (2020) ;36: (3):299–302. https://doi.org/10.1007/s12264-020-00476-9. |
[2] | Al Eid NA , Arnout BA , Alqahtani M , Fadhel FH , Abdelmotelab AS . The mediating role of religiosity and hope for the effect of self-stigma on psychological well-being among COVID-19 patients. Work. (2021) ;68: (3):525–41. https://doi.org/10.3233/WOR-203392 |
[3] | Arnout BA . Application of structural equation modeling to develop a conceptual model for entrepreneurship for psychological serviceworkers during theCOVID-19 pandemic. Work. (2021) ;69: (4):1127–41. https://doi.org/10.3233/WOR-205245 |
[4] | Alqahtani M , Arnout BA , Fadhel FH , Sufyan N . Risk perceptions of COVID-19 and its impact on precautionary behavior: A qualitative study. Patient Education and Counseling. (2021) ;104: (8):1860–7. https://doi.org/10.1016/j.pec.2021.02.025 |
[5] | Das R , Hasan MR , Daria S , Islam R . Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open (2021) ;11: :e045727,. doi: 10.1136/bmjopen-2020-045727 |
[6] | Fadhel FH . Psychological Intervention in Crisis Related to the COVID-19 Outbreak Epidemic: Theoretical Approach. Médecine Palliative—Soins de support —Accompagnement —Éthique. (2021) ;20: (5):267–70. https://doi.org/10.1016/j.medpal.2020.08.009 |
[7] | Jin H , Chen Y , Fu Q , Qu Q . Occupational risk factors of contracting COVID-19 among health workers: A systematic review. Work. (2021) ;69: (3):721–34. https://doi.org/10.3233/WOR-210477 |
[8] | Türktemiz H , Ünal Ö , Aydın DB . Assessment of healthcare professionals’ perceptions and attitudes towards the COVID-19 pandemic in Turkey. Work. (2021) ;69: (4):1163–70. https://doi.org/10.3233/WOR-205305 |
[9] | Chen Q , Liang M , Li Y . Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry (2020) ;7: (4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X |
[10] | Xiang Y-T , Yang Y , Li W , Zhang L , Zhang Q , Cheung T , Ng CH . Timely mental health care for the novel coronavirus outbreak is urgently needed. Lancet Psychiatry (2020) ;7: (3):228–9. doi: 10.1016/S2215-0366(20)30046-8 |
[11] | Al Ghobain M , Aldrees T , Alenezi A , Alqaryan S , Aldabeeb D , Aldhabib A , et al. Perception and Attitude of Emergency Room Resident Physicians toward Middle East Respiratory Syndrome Outbreak. Emergency Medicine International. (2017) ;2017: :1–4. doi: 10.1155/2017/6978256 |
[12] | Kang L , Li Y , Hu S , Chen M , Yang C , Yang BX , et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) ;7: (3):e14. https://doi.org/10.1016/S2215-0366(20)30047-X |
[13] | Liu S , Yang L , Zhang C , Xiang YT , Liu Z , Hu S , Zhang B . Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) ;7: (4):e17–e18. https://doi.org/10.1016/S2215-0366(20)30077-8 |
[14] | Arnout BA . Predicting psychological service providers’ empowerment in the light of the COVID-19 pandemic outbreak: A structural equation modelling analysis. Counselling and Psychotherapy Research (2020) ;20: (3):1–13. doi: 10.1002/capr.12328 |
[15] | Cai Q , Feng H , Huang J , Wang M , Wang Q , Lu X , et al. The mental health of Frontline and non-Frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. Journal of Affective Disorders. (2020) ;275: :210–215. https://doi.org/10.1016/j.jad.2020.06.031 |
[16] | Huang Y , Zhao N . Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Research. (2020) ;288: :112954. https://doi.org/10.1016/j.psychres.2020.112954 |
[17] | Huang Y , Zhao N . Chinese mental health burden during the COVID-19 pandemic. Asian Journal of Psychiatry. (2020) ;51: :102052. https://doi.org/10.1016/j.ajp.2020.102052 |
[18] | Liang Y , Chen M , Zheng X , Liu J . Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. Journal of Psychosomatic Research. (2020) ;133: :110102. https://doi.org/10.1016/j.jpsychores.2020.110102 |
[19] | Mo Y , Deng L , Zhang L , Lang Q , Liao C , Wang N , et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. Journal of Nursing Management. (2020) ;28: :1002–9. https://doi. org/10.1111/jonm.13014 |
[20] | Que J , Shi L , Deng J , Liu J , Zhang L , Wu S , et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General Psychiatry (2020) ;33: :e100259. |
[21] | Alonso J , Vilagut G , Mortier P , Ferrer M , Alayo I , Aragón-Peña A , et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Revista de Psiquiatria y Salud Mental. (2021) ;14: (2):90–105. https://doi.org/10.1016/j.rpsm.2020.12.001 |
[22] | Mediavilla R , Fernández-Jiménez E , Martínez-Alés G , Moreno-Küstner B , Martínez-Morata I , Jaramillo F , et al. Role of access to personal protective equipment, treatment prioritization decisions, and changes in job functions on health workers’ mental health outcomes during the initial outbreak of the COVID-19 pandemic [published online ahead of print, Aug 29]. Journal of Affective Disorders (2021) ;295: :405–9. doi: 10.1016/j.jad.2021.08.059 |
[23] | Feingold JH , Hurtado A , Feder A , Peccoralo L , Southwick SM , Ripp J , et al. Posttraumatic growth among health care workers on the frontlines of the COVID-19 pandemic. Journal of Affective Disorders. (2021) ;296: :35–40. https://doi.org/10.1016/j.jad.2021.09.032 |
[24] | Luo M , Guo L , Yu M , Jiang W , Wang H . The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Research. (2020) ;291: :113190. https://doi.org/10.1016/j.psychres.2020.113190 |
[25] | Pappa S , Ntella V , Giannakas T , Giannakoulis VG , Papoutsi E , Katsaounou P . Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity (2020) ;88: :901–7. doi: 10.1016/j.bbi.2020.05.026 |
[26] | Xiao X , Zhu X , Fu S , Hu Y , Li X , Xiao J . Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. Journal of Affective Disorders. (2020) ;274: :405–10. https://doi.org/10.1016/j.jad.2020.05.081 |
[27] | Chew N , Lee G , Tan B , Jing M , Goh Y , Ngiam N , et al. A multinational, multicenter study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity (2020) ;88: :559–65. |
[28] | Temsah MH , Al-Sohime F , Alamro N , Al-Eyadhy A , Al-Hasan K , Jamal A , et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. Journal of Infection and Public Health. (2020) ;13: :877–82. https://doi.org/10.1016/j.jiph.2020.05.021 |
[29] | Zhang WR , Wang K , Yin L , Zhao WF , Xue Q , Peng M , et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and Psychosomatics. (2020) ;89: (4):242–50. https://doi.org/10.1159/000507639 |
[30] | Hacimusalar Y , Kahve AC , Yasar AB , Aydin MS . Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. Journal of Psychiatric Research. (2020) ;129: :181–8. https://doi.org/10.1016/j.jpsychires.2020.07.024 |
[31] | Shechter A , Diaz F , Moise N , Anstey DE , Ye S , Agarwal S , et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry. (2020) ;66: :1–8. https://doi.org/10.1016/j.genhosppsych.2020.06.007 |
[32] | Sánchez-Sánchez E , García-Álvarez JÁ , García-Marín E , Gutierrez-Serrano M , Alférez MJM , Ramirez-Vargas G . Impact of the COVID-19 Pandemic on the Mental Health of Nurses and Auxiliary Nursing Care Technicians-A Voluntary Online Survey. Int J Environ Res Public Health. (2021) ;18: (16):8310. https://doi.org/10.3390/ijerph18168310 |
[33] | Murphy J , Spikol E , McBride O , Shevlin M , Bennett KMP , Hartman TK , et al. The psychological wellbeing of frontline workers in the United Kingdom during the COVID-19 pandemic: First and second wave findings from the COVID-19 Psychological Research Consortium (C19PRC) Study [Internet]. PsyArXiv; 2020. Available from: psyarxiv.com/dcynw. https://doi.org/10.31234/osf.io/dcynw |
[34] | El Haj M , Allain P , Annweiler C , Boutoleau-Bretonnière C , Chapelet G , Gallouj K , et al. High Exhaustion in Geriatric Healthcare Professionals During the COVID-19 Second Lockdown. Journao of Alzheimers Disease (2021) ;83: (4):1841–8. doi: 10.3233/JAD-210615 |
[35] | Azoulay E , Pochard F , Reignier J , Argaud L , Bruneel F , Courbon P , et al. Symptoms of Mental Health Disorders in Critical Care Physicians Facing the Second COVID-19 Wave: A Cross-Sectional Study. Chest (2021) ;160: (3):944–55. doi: 10.1016/j.chest.2021.05.023 |
[36] | Yang C , Liu W , Chen Y , Zhang J , Zhong X , Du Q , et al. Prevalence and risk factors for mental health symptoms in community epidemic prevention workers during the postpandemic era of COVID-19 in China. Psychiatry Research (2021) ;304: :114132. doi: 10.1016/j.psychres.2021.114132 |
[37] | Al-Hamid F . In the Time of a Pandemic: Health Practitioners Unknown Soldiers. Health heroes are spearheading. Okaz newspaper. 2020, April 17. https://www.okaz.com.sa/investigation/na/2019983. (Accessed November 21, 2021). |
[38] | Hamilton M . The assessment of anxiety states by rating. British Journal of Medical Psychology. (1959) ;32: :50–5. https://doi.org/10.1016/S2215-0366(20)30047-X |
[39] | Maier W , Buller R , Philipp M , Heuser I . The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. Journal of Affective Disorders (1988) ;14: (1):61–8. |
[40] | Kessler RC , Andrews G , Colpe LJ , Hiripi E , Mroczek DK , Normand SLT , et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. (2002) ;32: :959–76. doi: 10.1017/s0033291702006074 |
[41] | Andrews G , Slade T . Interpreting scores on the Kessler Psychological Distress Scale (k10). Australian and New Zealand Journal of Public Health (2001) ;25: :494–7. |
[42] | Barac A , Krnjaic P , Vujnovic N , Matas N , Runjic E , Rogoznica M , et al. The impact of the COVID-19 pandemic on resident physicians: A cross-sectional study. Work. (2021) ;69: (3):751–8. https://doi.org/10.3233/WOR-205253 |
[43] | Lu W , Wang H , Lin Y , Li L . Psychological status of medical workforce during the COVID-19 pandemic: A crosssectional study. Psychiatry Research. 2020288:112936. https://doi.org/10.1016/j.psychres.2020.112936 |
[44] | Cai W , Lian B , Song X , Hou T , Deng G , Li H . A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian Journal of Psychiatry. (2021) ;51: :102111. https://doi.org/10.1016/j.ajp.2020.102111 |
[45] | Sheraton M , Deo N , Dutt T , Surani S , Hall-Flavin D , Kashyap R . Psychological effects of the COVID 19 pandemic on healthcare workers globally: A systematic review. Psychiatry Research. (2020) ;292: :113360. https://doi.org/10.1016/j.psychres.2020.113360 |
[46] | Li Z , Ge J , Yang M , Feng J , Qiao M , Jiang R , et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, Behavior, and Immunity. (2020) ;88: :916–9. https://doi.org/10.1016/j.bbi.2020.03.007 |
[47] | Spoorthy MS , Pratapa SK , Mahant S . Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian Journal of Psychiatry. (2021) ;51: :102119. https://doi.org/10.1016/j.ajp.2020.102119 |
[48] | Repon M , Pakhe SA , Quaiyum S , Das R , Daria S , Islam MR . Effect ofCOVID-19 pandemic on mental health among Bangladeshi healthcare professionals: A cross-sectional study. Science Progress. (2021) ;104: (2):368504211026409. https://doi.org/10.1177/00368504211026409 |
[49] | Islam MR , Quaiyum S , Pakhe SA , Repon M , Bhuiyan MA . Dataset concerning the mental health of healthcare professionals during COVID-19 pandemic in Bangladesh. Data in Brief. (2021) ;39: :107506. https://doi.org/10.1016/j.dib.2021.107506 |



