COVID-19 Pulmonary Infection with Pneumothorax in a Young Patient
By Okan Gurkan1, Ayhan Yilmaz1, Ferhat Cengel1, Elif Sargin Altunok2, Elif Evrim Ekin1Affiliations
doi: 10.29271/jcpsp.2020.06.43ABSTRACT
Coronavirus disease (COVID-19), first reported in December 2019 in Wuhan, China, has spread all over the world in a short time and was declared as a pandemic by the World Health Organization (WHO). During COVID-19 pandemic, chest computed tomography (CT) imaging has become an important tool with high sensitivity for diagnosis due to the low positive rate of the real-time reverse-transcriptase polymerase chain reaction (RT-PCR). Furthermore, the chest CT has played an important role in the diagnosis of underlying pulmonary lesions. In this case report, we present a patient who was admitted to the emergency department with fever, cough and left shoulder pain, and was subsequently diagnosed with both COVID-19 and pneumothorax following chest CT and RT-PCR test.
Key Words: COVID-19, Coronavirus, Pneumothorax, Tomography.
INTRODUCTION
On December 31st, 2019, Wuhan Municipal Health Commission declared that medical institutions have been reporting a substantial number of pneumonia cases that are related to South China Seafood City.1 On January 7, 2020, the cause of the pneumonia outbreak was isolated by Chinese scientists. This novel coronavirus was named as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) by Coronavirus Study Group and the disease was named coronavirus disease 2019 (COVID-19) by World Health Organization (WHO).2 On March 11th, 2020, WHO announced this outbreak as a pandemic.3 By May 2, 2020, a total of 3,416,458 confirmed cases and 239,894 deaths from all over the world were reported.4
Since real-time polymerase chain reaction (RT-PCR) has a low positive rate, chest computed tomography (CT) imaging has become an important tool with high sensitivity for the diagnosis of COVID-19, especially in epidemic areas.5 Furthermore, chest CT also plays an important role in the diagnosis of accompanying pulmonary lesions. Pneumothorax is one of the pulmonary emergencies in which early diagnosis and treatment initiation is crucial.
In this case report, we present a young patient having COVID-19 pneumonia associated with pneumothorax.
CASE REPORT
On March 26, 2020, a 24-year male was admitted to the hospital due to persistent dry cough for 4 days, fever for 2 days, and left shoulder pain for 2 hours. He had no medical history and was a non-smoker. The patient had a history of contact with an RT-PCR confirmed COVID-19 patient.
On admission, his oxygen saturation was 92% on room air, and blood gases demonstrated a pH of 7.42, pCO2 of 31.6 mmHg, pO2, 68.7 mmHg, and HCO3, 25 mmol/dL. Body temperature was 37.9°C. Laboratory findings reported, C-reactive protein of 50.5 mg/L (normal range: 0-5 mg/L), white blood cells, 5040 per μL (normal range: 4100-11,000 per μL), haemoglobin, 159 g/L (normal range: 110-180 g/L), platelets, 134,000 per μL (normal range: 150,000-400,000 per μL), and alanine aminotransferase, 12 U/L (normal range: 0-50 U/L). Blood pressure was 135/75 mmHg. Nasal and pharyngeal swabs were taken for RT-PCR test.
A posteroanterior chest X-ray showed a paracardiac thin lucent line in the left hemithorax, which raised the suspicion of pneumothorax. There were no findings suggestive of COVID-19. Chest CT was planned since the patient's symptoms and history were suggestive of viral pandemic disease. Chest CT examination showed left anterior pneumothorax and bilateral peripheral ground-glass opacities, suggestive of viral pneumonia. Also, he had emphysema-like lung parenchymal changes at the apices of both upper lobes (Figure 1 A,B,C). The patient was transferred to the COVID-19 isolation floor. He was given oxygen therapy at 3 L/min flow rate. The results of bacterial culture tests were negative. One day after admission, he was confirmed to have COVID-19 via RT-PCR test.
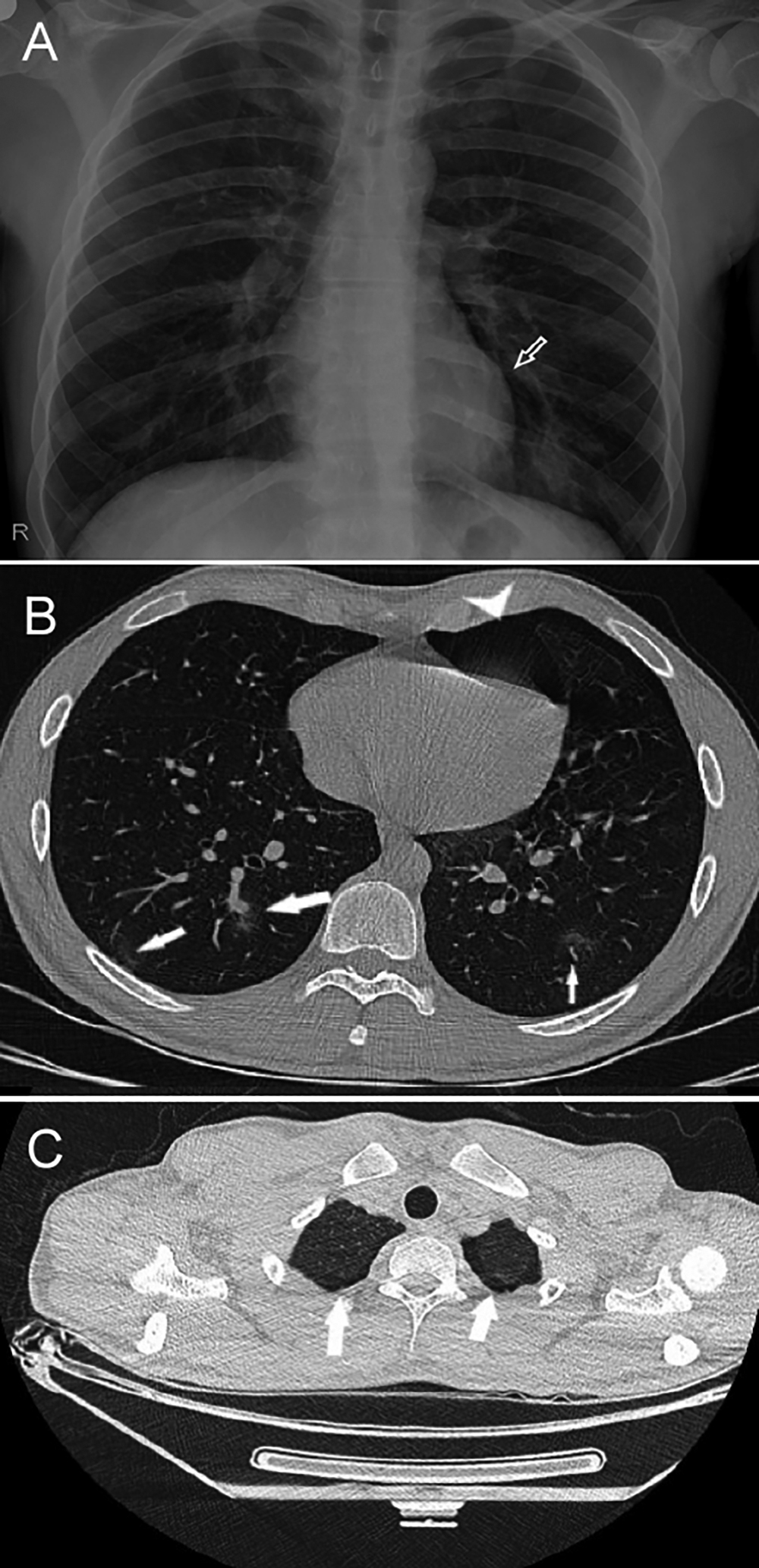 Figure 1: X-ray and axial thin-slice CT images taken on first day of admission. (A) A paracardiac thin lucent line in the left hemithorax raising the possibility of pneumothorax (arrow). (B) Bilateral peripheral ground-glass opacities (arrows) and left anterior pneumothorax (arrowhead). During this pandemic, peripheral ground-glass opacities are suggestive of COVID-19. (C) Emphysema-like lung parenchymal changes at the apices of both upper lobes (arrows).
Figure 1: X-ray and axial thin-slice CT images taken on first day of admission. (A) A paracardiac thin lucent line in the left hemithorax raising the possibility of pneumothorax (arrow). (B) Bilateral peripheral ground-glass opacities (arrows) and left anterior pneumothorax (arrowhead). During this pandemic, peripheral ground-glass opacities are suggestive of COVID-19. (C) Emphysema-like lung parenchymal changes at the apices of both upper lobes (arrows).
The patient was treated with hydroxycloroquine 200 mg (2x2 loading dose followed by 2x1 oral), azithromycin 250 mg (2x1 first day followed by 1x1), oseltamivir 75 mg (2x1 oral), and enoxaparin sodium 0.4 ml (1x1 sc), for five days as recommended by the national guidelines of the Ministry of Health of Turkey. Within two days after admission, his clinical status was stable. Oxygen saturation was 95% without oxygen therapy. Within three days, the patient was afebrile and left shoulder pain almost disappeared.
Chest X-ray taken seven days after admission was normal (Figure 2). There were no abnormal findings on laboratory tests as well. The patient was discharged from the hospital as his complaints were significantly reduced and was home isolated for 14 days after discharge.
Figure 2: Normal chest X-ray, taken seven days after admission.
DISCUSSION
Pneumothorax is characterized by the presence of air between visceral and parietal pleural layers. It is classified as traumatic and nontraumatic (spontaneous). One of the most common thoracic diseases affecting adolescents and young adults is primary spontaneous pneumothorax (PSP).6 PSP's clinical course varies with a risk of recurrence ranging from 25% to 54%. An essential determinant of recurrence appears to be the presence of underlying chronic lung disease. Although most patients with PSP have emphysema-like lung parenchymal changes, PSP also occurs in patients with no clinically evident lung disease.7 Nonetheless, the position of bullae and blebs as the sole cause of PSP is doubtful, as only about 20% of patients demonstrate it. The cough has also been reported as a possible cause of spontaneous pneumomediastinum and pneumothorax.8
Although our patient was non-smoker, he had emphysema-like lung parenchymal changes at both upper lobes' apices. However, he also had a severe and persistent cough for four days due to COVID-19 pneumonia. Our patient improved promptly with nearly complete symptom resolution in less than three days and with normal chest X-ray findings in 7 days.
Chest CT has been considered as the standard imaging tool for definitive diagnosis of COVID-19 as well as for follow-up in particular cases. It facilitates the detection of the lesions at early stages.9 The most common finding is peripheral ground-glass opacity with lower lobe predominance. Chest CT has been a frequently used imaging modality for rapid and accurate diagnosis of patients with suspected COVID-19 in emergency departments during the current pandemic. Thus, patients having positive findings on CT are directed for treatment and isolation immediately.
To the best of our knowledge, this is the first case report of a patient with COVID-19 and pneumothorax simultaneously at admission. In one case report, pneumothorax has been reported in a COVID-19 patient during stay in the hospital, possibly occuring as a complication following non-invasive ventilation therapy.10
Precise severity assessment of COVID-19 pneumonia can be made on chest CT, which can help in management decisions, especially in critical cases. X-ray is also essential for the diagnosis and follow-up in COVID-19 patients.
In our patient, X-ray was not sufficient for the diagnosis of COVID-19. On CT chest, both diseases were diagnosed and the necessary treatments were initiated in a short time interval. The positive RT-PCR results were also used for confirming the diagnosis.
Alveolar damage or prolonged coughing due to COVID-19 may possibly have contributed to the development of pneumothorax and the emphysema-like appearance in our patient, but it needs further corroboration and research.
PATIENT'S CONSENT:
Informed consent was obtained from the patient for publication of this case report.
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
OG: Manuscript writing, data collection, revision, submission.
AY: Design, data collection, revision.
FC: Revision, proofreading.
ESA: Data collection, analysis.
EEE: Revision, analysis, proofreading.
REFERENCES
- World Health Organization. 2020. Pneumonia Of Unknown Cause – China. [Internet] Available from: https:// www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [Cited 2 May 2020].
- Gorbalenya A, Baker S, Baric R, de Groot R, Drosten C, Gulyaeva A, et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses – a statement of the Coronavirus Study Group 2020; 1-15.
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020; 91(1):157-60.
- Worldometers.info. 2020. Coronavirus Update (Live): 3,416,458 Cases And 239,894 Deaths From COVID-19 Virus Pandemic - Worldometer. [Internet] Available from: https:// www.worldometers.info/coronavirus/ [Cited 2 May 2020].
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223):497-506.
- Bobbio A, Dechartres A, Bouam S, Damotte D, Rabbat A, Regnard J, et al. Epidemiology of spontaneous pneumo-thorax: Gender-related differences. Thorax 2015; 70(7): 653-8.
- Lesur O, Delorme N, Polu JM, Fromaget JM, Bernadac P. Computed tomography in the etiologic assessment of ıdiopathic spontaneous pneumothorax. Chest 1990; 98(2):341-7.
- WEISSBERG D. Spontaneous mediastinal emphysema. Eur J Cardio-Thoracic Surg 2004; 26(5):885-8.
- Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: Relationship to negative RT-PCR testing. Radiology 2020; 200343.
- Zhou C, Gao C, Xie Y, Xu M. COVID-19 with spontaneous pneumomediastinum. Lan Infec Dis 2020; 20(4):510.