Efficacy and safety of ultrasound-guided core needle biopsies (US-CNBs) in cervical lymphadenopathy in patients with suspected head and neck cancer during the COVID-19 pandemic
Abstract
BACKGROUND:
Cervical lymphadenopathy can be benign or malignant. Its accurate diagnosis is necessary to determine appropriate treatment. Ultrasound-guided core needle biopsies (US-CNBs) are frequently used as a percutaneous sampling approach.
OBJECTIVES:
Our aim was to identify the efficacy and safety of US-CNBs in 125 patients with cervical lymphadenopathy and clinically suspected head and neck cancer during the COVID-19 pandemic with limited surgical resources.
METHODS:
US-CNBs of pathological lymph nodes were performed in 146 lymph nodes on 125 patients. Biopsies were performed ultrasound-guided with a reusable gun core biopsy system and a 10-cm-long 16-G needle. Standard of reference for the histological findings were panendoscopy, clinical and sonographic follow-up, surgical biopsy or a repeat US-CNB.
RESULTS:
Adequate material for histologic diagnosis was obtained in 111 patients (89%), of these 83 patients (75%) were diagnosed as malignant, whereas benign lymphadenopathy accounted for 28 patients (25%). Therefore, US-CNB was able to identify malignant or benign lymphadenopathy with an overall accuracy of 88% and 90%, respectively.
CONCLUSIONS:
Percutaneous US-CNB is a safe and effective alternative to surgical biopsy in the management of cervical lymphadenopathy in patients with clinically suspected head and neck cancer in a setting with limited resources.
1Introduction
Lymphadenopathy in the head and neck region can be benign or malignant. A medical history and physical examination, along with laboratory and radiological examinations, can help identify the cause of lymphadenopathy, although histopathology remains the standard requirement [1–7].
Accurate diagnosis of suspicious lymph nodes is necessary to determine appropriate treatment. In addition to medical history and clinical findings, various imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US) are used to assess masses of unclear character in the head and neck region. US has proven to be an inexpensive, simple, and accurate real-time imaging modality [7–10].
For patients with a presentation of cervical lymphadenopathy, fine needle aspiration cytology (FNAC) is commonly used as a diagnostic device, however this approach best gives cytomorphologic information [11–14]. FNAC is a non-invasive and useful method for assessing cervical lymphadenopathy, with reported diagnostic accuracy greater than 90% in malignant lymphadenopathy [15, 16]. Unfortunately, FNAC supplies nondiagnostic material in 10% to 15% of cases [8, 17]. Additionally, the diagnostic accuracy of FNAC differs with disease entity and is highly operator dependent [18–20].
Despite repeated FNAC, there is a significant number of cases where excisional biopsy is required to obtain the definite diagnosis. Histopathological examination of completely resected tumours remains the gold standard in the head and neck region, as histology is preserved and sufficient material is available for additional analysis [8, 17].
However, excisional biopsies are time consuming, invasive, tissue damaging, and often require hospitalization and general anaesthesia.
Additionally, this approach is not suitable for all patients, mainly due to surgical risks as well as the current scarce availability of surgical resources as during the coronavirus disease 2019 (COVID-19) pandemic. Alternative methods should not only have low technical risk and high diagnostic yield, but also be easy to implement and have low economic cost analysis [8, 17].
Recently, core needle biopsies (CNBs) were increasingly used as a percutaneous sampling approach [11, 21]. Needles with sizes of 14G–18 G can offer massive quantities of intact tissue fabric and thereby permit evaluation of structure as well [11, 21, 22].
CNBs are extensively commonplace as an efficient device for the analysis of carcinoma and for deep-seated tumour manifestations which can be best reachable through CT- or endoscopy-guided techniques [11, 23]. CNBs combined with ultrasound imaging has occasionally been used in the work-up of head and neck lesions [8, 24–28]. Furthermore, CNB is a minimally invasive, safe, and accurate method that produces histological specimens that preserve cytological appearance and tissue architecture [8, 17].
However, to the best of our knowledge, there are already several studies as well as reviews that have described the factors that influence the diagnostic accuracy of ultrasound-guided CNB (US-CNB), which has been performed for over 10 years at our center. Though there are only few data regarding only patients with suspected metastatic head and neck cancer, of which we have complete records for all these patients as well as an established standardized procedure. Therefore, the aim of our study was to determine the diagnostic yield, efficacy, and safety of US-CNB in patients with cervical lymphadenopathy and clinically suspected head and neck cancer and to identify the factors that influence the diagnostic accuracy of US-CNB during the COVID-19 pandemic.
2Material and methods
US-CNBs of pathological lymph nodes were performed in our Department of Diagnostic and Interventional Radiology on 125 consecutive patients between April 2020 and November 2022, who before had presented with cervical lymphadenopathy in our Department for Otorhinolaryngology and data was analysed retrospectively and in whom a histopathologic probe sampling was medically indicated by the referring clinician, only in patients with suspected primary head and neck cancer. Informed consent for the biopsy procedure was obtained before the procedure. The Independent Ethics Committee at the Regensburg University confirmed, that for the scientific project no ethics-approval or commission's opinion was necessary due to the fact, that according to applicable laws and guidelines such retrospective study without any study-related clinical intervention or use of patients’ personal data does not have to be submitted to the ethics committee.
International Normalized Ratio (INR) and platelet count (PC) were checked, and thresholds were INR≤2.0 and PC≥50×103 per μL. Acetylsalicylic acid or clopidogrel medication was continued; warfarin was stopped and replaced by heparins, which were paused on the day of biopsy. For patients with a medication of novel oral anticoagulants (NOACs), such as dabigatran, rivaroxaban, apixaban and edoxaban the US-CNB was classified as low-risk procedure and their medication was paused depending on the renal function and the particular drug for 1–2 days, respectively [11].
Patients were examined by palpation for enlarged lymph nodes or masses, and then assessed by ultrasound (Aplio 300, Toshiba, Tokyo, Japan) with a 5–14 MHz linear probe transducer (PLT-1005BT, Toshiba, Tokyo, Japan) for the feasibility of a core needle biopsy. In general, lymph nodes approximately 1.5 cm in diameter in each cervical lymph node station have been considered suitable targets. Smaller lymph nodes were exceptionally allowed. If multiple lymph nodes were present, the one that grew fastest or had the most questionable morphological features depending on medical history was selected [11].
Morphological features indicative of malignant lymph nodes are loss of hilar architecture, rounded shape, large or bulky formations, and hyperperfusion of perilymphatic hilus and neovascularization as well as extracapsular extension and peripheral vascularization [1, 11]. Necrotic areas were avoided. Prior to biopsy, lymph node diameter was assessed and vascular perfusion of lesions and surrounding great vessels was examined with doppler ultrasound to minimize the risk of bleeding. Anatomical regions with a high risk of nerve lesion were avoided (Fig. 1).
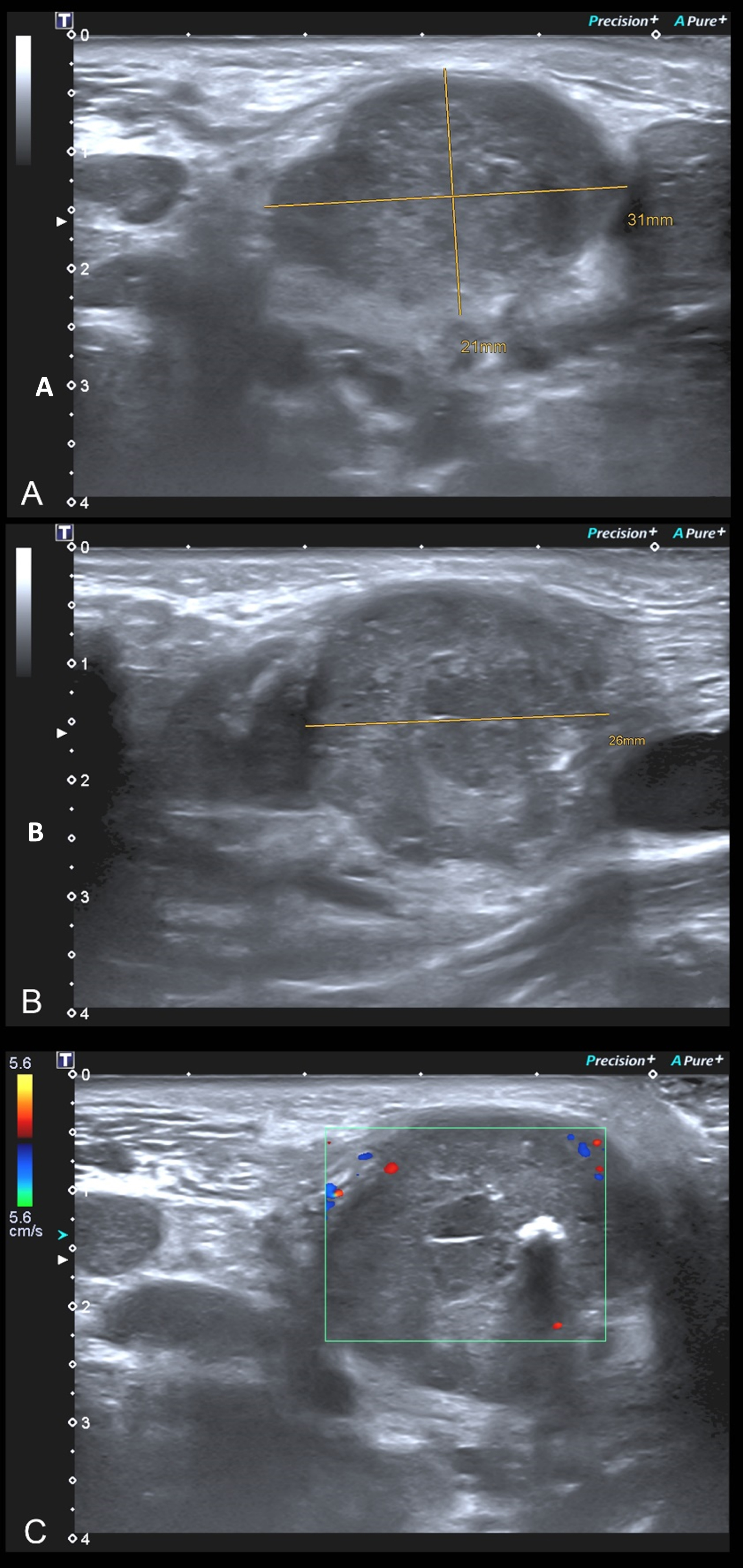
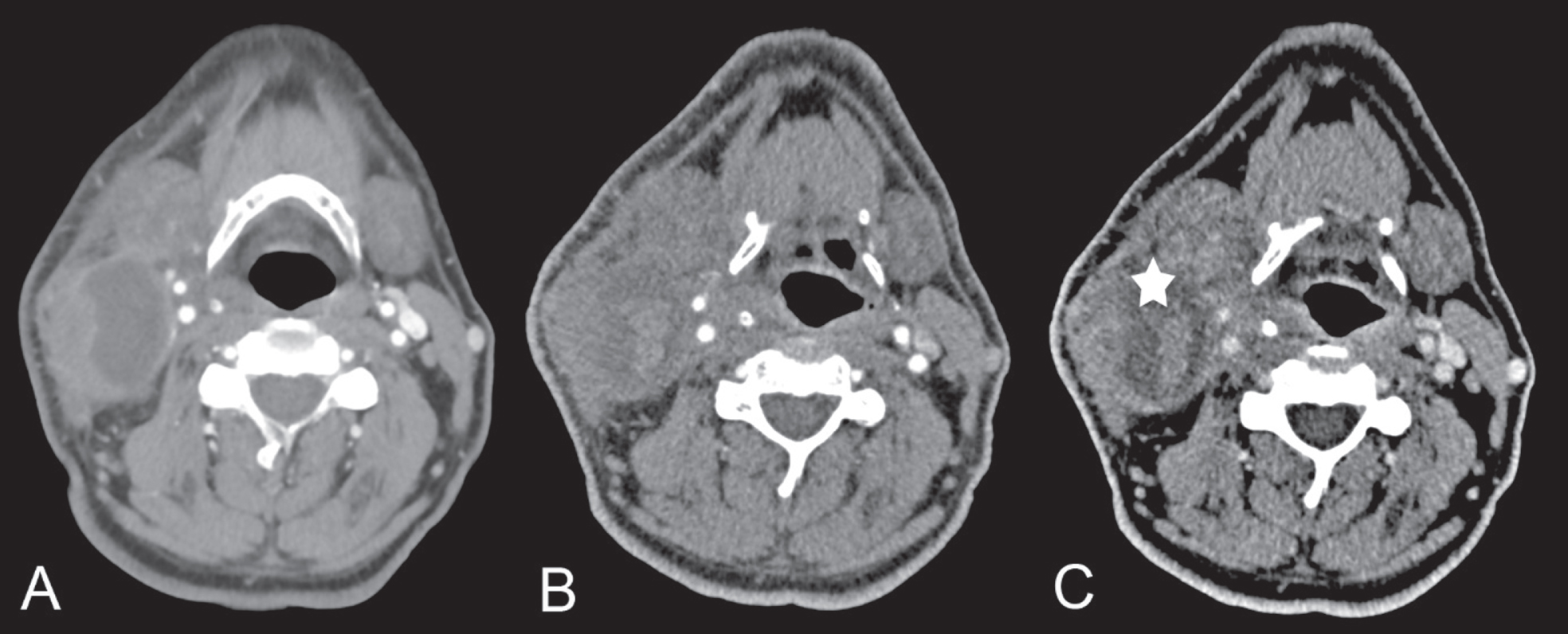
Fig. 1
B-Mode Sonography (A, B) and Doppler-Sonography (C), performed to identify and safely evaluate the lesion intended to be biopsied with US-CNB.
All biopsies were performed ultrasound-guided with a reusable gun core biopsy system (Magnum Reusable Biopsy Gun, Bard, New Providence, New Jersey, USA) and a 10-cm-long 16-G needle (Bard, New Providence, New Jersey, USA) with an extendible inner trocar with a 2 cm groove for the sample using ultrasound control. Skin was disinfected with alcohol, a local anaesthesia of the cutis and subcutaneous tissue was performed with approximately 5 to 8 ml of a 1% prilocainhydrochlorid local anaesthetic solution (Xylonest 1%, Aspen Pharma Trading, Durban, South Africa), and a 3–4 mm incision was made near to the lesion of interest. At least two and up to four samples from the same lymph node were routinely obtained (Fig. 2). Manual compression of the puncture site was carried out in all patients for 5 to 15 minutes to stop or to avoid bleeding. US-CNBs were performed by three operators with at least 10 years of experience with this procedure.
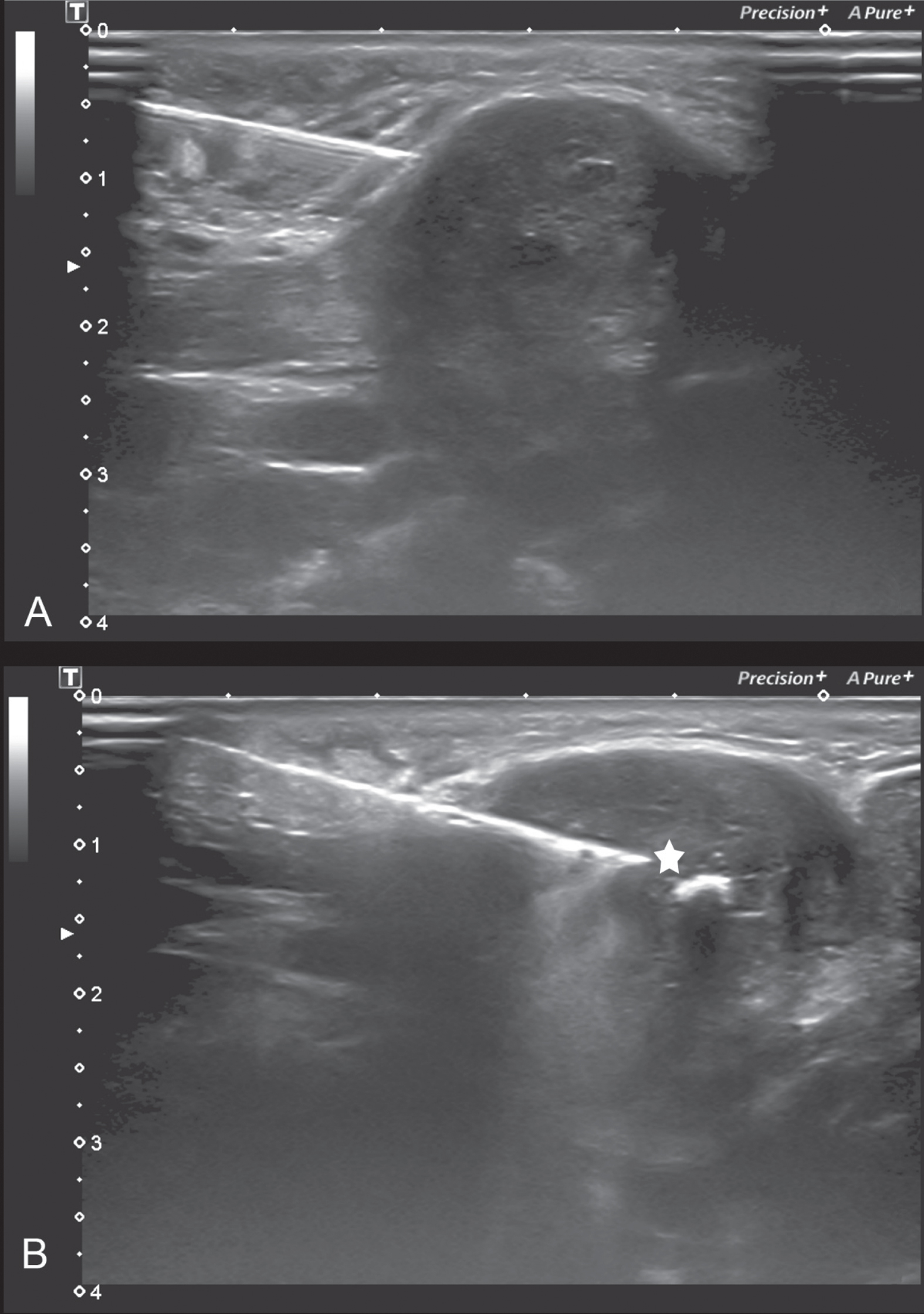
Fig. 2
US-CNB is performed in B-Mode Sonography and the local anaesthesia is placed first (A) in the sample surrounding as well as (sub-)cutaneous before the 10-cm-long 16-G needle of the reusable gun corebiopsy system is put into the target (B); the tip of the needle is marked witha white star (*).
Time elapsed for performing the US-CNB by the conducting physician was assessed, beginning with the entering of the examination room by the performing physician till the end of manual compressing of the puncture site.
Some samples were rolled off for air-dried cytology stains and then were immediately fixated in 4% buffered formaldehyde. Potential bleeding was stopped by compression and a routine US control of the biopsied lesion was performed (Fig. 3) as proposed before [11].
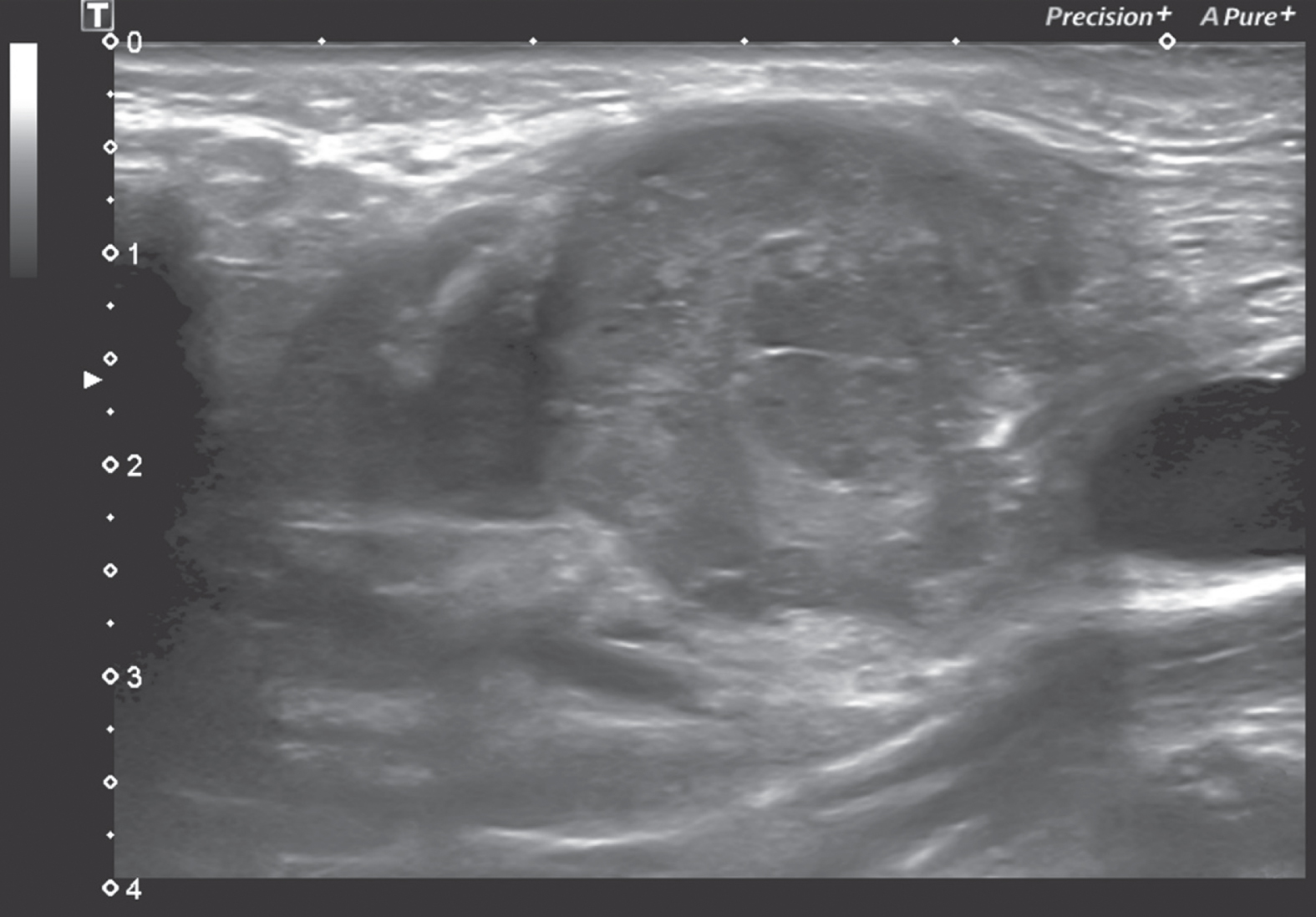
Fig. 3
US control of the biopsied lesion is performed to rule out potential bleeding in B-Mode sonography.
After a short time of observation of approximately 30 min, the patient could leave the intervention room and was transferred to station in case of inpatient or allowed to leave the clinic in case of outpatient handling.
Histopathological results were collected and statistical analysis was performed using Excel Tables (Microsoft Excel 2019, Microsoft, Redmond Washington, USA) and SPSS (version 28, Statistical Package for Social Science, IBM Corp., Armonk, NY, USA); measurement data were expressed as mean and its standard deviation (SD) and percentages (%) were calculated using descriptive statistics as required by scientific standards.
3Results
3.1Patient characteristics
Of the 125 patients in this study, 45 (36%) were female, and 80 (64%) were male. The age range was from 18 to 89 years (mean 52 years with a SD of 8 years). In total, 107 (86%) patients had a history of malignant disease yet. A total of 146 lymph nodes in those 125 patients were biopsied in this study, 76 (52%) on the right side and 70 (48%) on the left side. The mean short-axis diameter of the lymph nodes was 1.6 cm (range 0.8–8.8 cm) with a SD of 0.8 cm.
3.2Quality of achieved US-CNBs
Adequate material for histologic diagnosis was obtained in 111 patients (89%), whereas inadequate samples were reported in 14 cases (11%). In those 14 failed US-CNB procedures inadequate samples were obtained due to only necrotic debris or fibroadipose tissue and no nodal tissue in the sample acquired (n = 5; 36%) or insufficient tissue obtained from an accurately sampled node (n = 9; 64%). Those patients underwent surgical biopsy to make the final diagnosis.
3.3Diagnosis made by histopathology
Of these 111 patients, 83 patients (75%) were diagnosed as malignant by US-CNB, including 72 cases of metastatic carcinoma (65%) and 11 cases of lymphoma (10%). So, US-CNB was able to identify malignancy in head and neck lymph nodes with an overall accuracy of 88% with 83 detected cases of 94 overall patients with proven malignancy (Table 1).
Table 1
Detailed overview of the 94 histological malignant diagnoses of which 83 were made using the US-CNB procedure in enlarged cervical lymph nodes
| Definite histological diagnosis made | Number of cases detected by US-CNB | Number of cases detected by all modalities in summary | Diagnostic performance of US-CNB (%) |
| Malignant lymphadenopathy | 83 | 94 | 88% |
| Squamous cell carcinoma | 58 | 65 | 89% |
| Adenocarcinoma | 6 | 8 | 75% |
| Neuroendocrine sinunasal carcinoma | 2 | 3 | 66% |
| Mucoepidermoid carcinoma | 2 | 2 | 100% |
| Malignant melanoma | 2 | 2 | 100% |
| Undifferentiated carcinoma | 2 | 2 | 100% |
| Hodgkin’s lymphoma | 6 | 7 | 86% |
| Non-Hodgkin’s lymphoma | 3 | 3 | 100% |
| Multiple myeloma | 2 | 2 | 100% |
Benign lymphadenopathy accounted for 28 of 111 patients (25%) with adequate US-CNBs tissue samples. Reactive hyperplasia, the most common benign condition, was detected in 18 patients (16%) in US-CNB, while the second most common benign condition, tuberculosis, was detected in 6 cases (5%), followed by 4 patients (4%) with different infectious lymphadenopathy. US-CNB was able to identify benign conditions in head and neck lymph nodes with an overall accuracy of 90% with 28 proven cases of 31 overall patients with swollen lymph nodes due to benign conditions (Table 2).
Table 2
Detailed overview of the 31 histological benign diagnoses of which 28 were made using the US-CNB procedure in enlarged cervical lymph nodes
| Definite histological diagnosis made | Number of cases detected by US-CNB | Number of cases detected by all modalities in summary | Diagnostic performance of US-CNB (%) |
| Benign lymphadenopathy | 28 | 31 | 90% |
| Reactive hyperplasia | 18 | 20 | 90% |
| Tuberculosis | 6 | 6 | 100% |
| Infectious mononucleosis | 2 | 2 | 100% |
| Fungal infection | 1 | 2 | 50% |
| Cat-scratch disease | 1 | 1 | 100% |
3.4Confirmation of diagnosis made by US-CNB
The adequate biopsy samples obtained were confirmed either by the histological findings of tissue sampling of the suspected primary following panendoscopy (n = 66, 53%); the combination of surgical biopsy and clinical follow-up (n = 20; 16%), sole clinical and sonographic follow-up (n = 16, 13%); surgical biopsy (n = 14, 11%) or a repeat US-CNB (n = 9, 7%), respectively. Clinical follow-up lasting for a mean of 12 months with a range 1–31 months (SD 8.5 months).
Table 1 provides a detailed analysis of the 83 malignant histological final diagnoses made using the US-CNB procedure, whereas table 2 provides an overview of the 28 diagnoses made in benign lymphadenopathy.
3.5Complications
Tumour-cell seeding. Seeding after US-CNB is specifically discussed in the literature. No cases of tumour-cell seeding were observed in our cohort during follow-up.
Bleeding. Immediate sonographic control of the target site was performed when complications were suspected. Only 4 complications (3%) in 125 patients were reported. The most common complication observed was minor hematomas in 2 patients (50%), followed by one major bleeding (25%) at the puncture site (Figs. 4 and 5) and by one local infection (25%). No deaths, or nerve injuries were reported.
Fig. 4
Images of a 66-years old patient with a large partial cystic lymph node metastasis on the right side in whom a US-CNB of the lesion was performed and a major bleeding occurred afterwards. Fig. 4 A and B demonstrate the B-Mode sonography of the lesion with the US-CNB placement in the solid rim of the lesion (marked with a white star (*)).
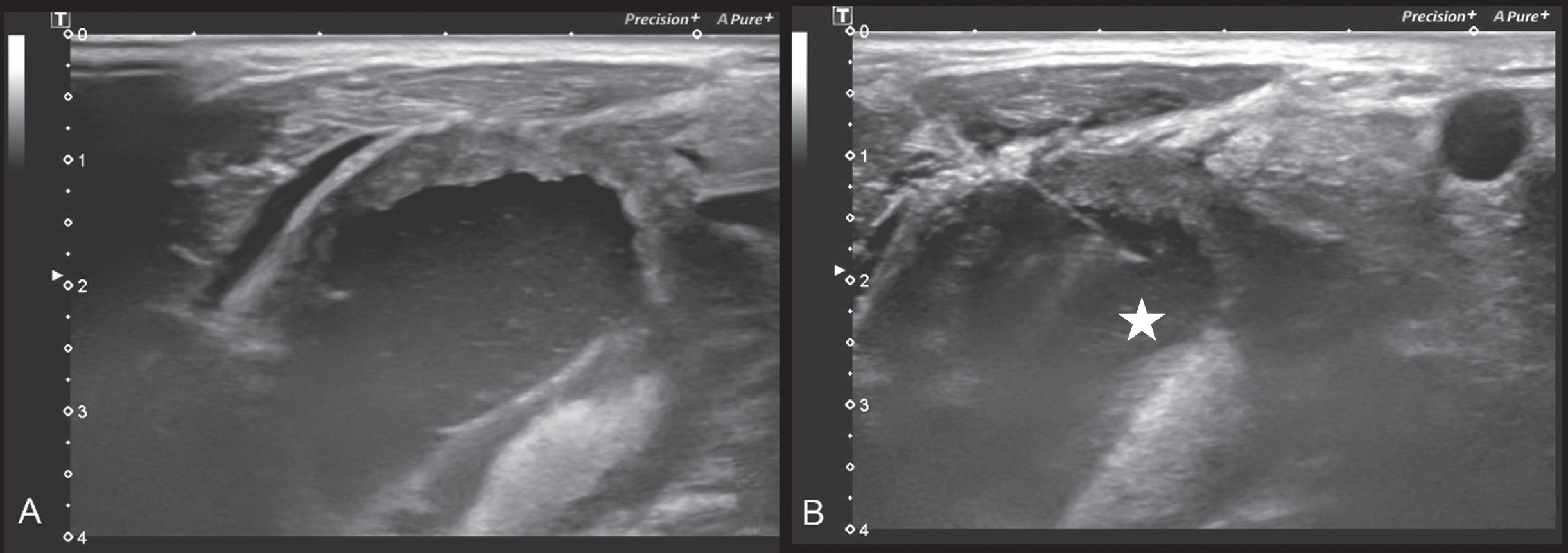
Fig. 5
A shows the lesion in CT before the US-CNB and Fig. 5 B and C represent the CT in arterial (B) and venous phase (C) which was performed after the US-CNB to potentially detect the bleeding site (but no acute bleeding was detected) and to document the hematoma size (*) within the cystic part of the metastatic lymph node.
3.6Duration
Mean intervention time was 29 minutes with a range from 17 minutes to 88 minutes and a SD of 10 minutes. This including the time from the physician entering the examination room, palpation for enlarged lymph nodes or masses, assessment by ultrasound and accomplishing a sterile environment as well as setting local anaesthesia of the cutis and subcutaneous tissue, incision, performing the US-CNB and compressing the puncture site afterwards.
4Discussion
The present study has shown that US-CNB is an effective method for the characterisation of cervical lymphadenopathy in a setting of prolonged limited surgical resources in patients with clinically suspected head and neck cancer, with an accuracy of 88% and 90% in the recognition of malign or benign lymphadenopathy, respectively.
In our series 125 patients were diagnosed by US-CNBs for the assessment of cervical lymphadenopathy during the COVID-19 pandemic, adequate samples were obtained in 111 patients (89%), which is consistent with the 90–94% rate of adequate sampling reported in previous studies [3, 8, 25, 26, 29].
Of the unsatisfactory specimens, 5 (36%) were due solely necrotic debris or fibro-adipose tissue, with no nodular tissue in the collected specimens. This failure results from insertion of the biopsy needle into necrotic tissue. By reviewing ultrasonography, hypoechogenecity on ultrasound and lack of internal vasculature on Colour Doppler indicate possible central necrosis; contrast enhanced ultrasound (CEUS) could be helpful to safely recognize vital tumour areas but has not yet been evaluated in this field. It is important to perform the biopsy in the solid or peripheral portion of the lymph nodes to avoid the necrotic tissue in the central region [3, 8, 30, 31]. Mu W et al. conducted a study in a total of 168 patients who required puncture of lymph nodes with 76 patients punctured with conventional ultrasound guidance, of which 37 received FNA and 39 received US-CNB. Moreover, 92 patients in contrary were guided by CEUS, of which 41 received FNA and 51 received US-CNB. They found a diagnostic accuracy of FNA and CNB guided by CEUS being higher than that guided by conventional ultrasound, with a statistically significant (p < 0.05) difference [32].
In total, 9 (64%), of inadequate samples had been sampled correctly but contained insufficient material for a definitive diagnosis. Crushing of the tissue may be a cause of this error, as cell rupture and morphological distortion make it difficult to interpret such tissue samples. In addition, lymphoma may be a cause of failure of US-CNB diagnosis. Many studies have reported that CNB in general is an effective procedure for lymphoma, with a high diagnostic yield. However, for follicular lymphoma, composite lymphoma, and other rare types of lymphoma, surgical biopsy is superior to CNB [33–35].
In patients with multiple lymphadenopathies, it is recommended to collect the lymph nodes with the most questionable morphological features rather than the largest lymph nodes. This is because harvesting the largest lymph nodes with normal morphological features can also lead to false-negative diagnoses [3].
Furthermore, short axis diameter, malignant lymphadenopathy, and tending to longer penetrating distances are known to be associated with a higher diagnostic yield. First, it is much easier to locate and sample large lymph nodes, making it more likely that such nodes will yield an adequate sample. Second, since malignant nodules are stiffer than benign nodules, they can be targeted more precisely, thus allowing deeper penetration distances to be safely used for these nodules. Because needle size does not affect the diagnostic accuracy of US-CNB, only 16 G needle systems were used in this study [3, 26, 33].
Moreover, US-CNB has been proven superior to free-handed biopsies, which should be limited to superficial lesions; the use of US-CNB can reduce the need of repeat biopsies [36].
Serious complications have rarely been reported in previous studies of US-CNB from cervicofacial masses. The most common complication is bleeding, with a reported incidence of 1–3% [37, 38].
In our study, only 4 complications (3%) in 125 patients were reported. The most common complication observed was minor hematomas in 2 patients (50%), followed by one major bleeding (25%) at the puncture site (which led to a 48 hour lasting hospitalization of this outpatient without the need for further treatment) and by one local infection (25%). No deaths, or nerve injuries were reported. Therefore, we recommend that a thorough ultrasound examination be performed before the biopsy procedure, and that the puncture points be compressed for a slightly longer time after the biopsy in patients with a higher risk of bleeding [3, 39–41].
The study is limited by the population size, the missing analysis of morphologic features of the targeted lesions and the missing execution of CEUS in the planning or conducting of US-CNB, which both has the potential to optimize the results of US-CNB.
Further studies with regard to morphological features and analyzation of microvascularization of the targeted lesions should be performed, especially with regard to the possibility of CEUS-guided US-CNB with the aim of an optimization of sample validity and the further reduction of repeat biopsies [32, 42–45].
5Conclusion
In our clinical experience, percutaneous US-CNB is a safe and effective alternative to surgery in the management of cervical lymphadenopathy in patients with clinically suspected head and neck cancer especially in times of limited surgical capacities as it was during COVID-19 pandemic.
References
[1] | Künzel J , Brandenstein M , Zeman F , Symeou L , Platz Batista da Silva N , Jung EM , Multiparametric Ultrasound of Cervical Lymph Node Metastases in Head and Neck Cancer for Planning Non-Surgical Therapy. Diagnostics (Basel). (2022) ;12: (8):1842. doi: 10.3390/diagnostics12081842 |
[2] | Rennert J , Grosse J , Einspieler I , Bäumler W , Stroszczynski C , Jung EM , Complementary imaging of ultrasound and PET/CT: A new opportunity? Clin Hemorheol Microcirc. (2021) ;79: (1):39–54. doi: 10.3233/CH-219105 |
[3] | Han F , Xu M , Xie T , Wang JW , Lin QG , Guo ZX , Zheng W , Han J , Lin X , Zou RH , Zhou JH , Li AH , Efficacy of ultrasound-guided core needle biopsy in cervical lymphadenopathy: A retrospective study of 6,695 cases. Eur Radiol. (2018) ;28: (5):1809–17. doi: 10.1007/s00330-017-5116-1 |
[4] | Lachar WA , Shahab I , Saad AJ , Accuracy and cost-effectiveness of core needle biopsy in the evaluation of suspected lymphoma: a study of 101 cases. Arch Pathol Lab Med. (2007) ;131: (7):1033–9. doi: 10.5858/2007-131-1033-AACOCN |
[5] | Zhao D , He N , Shao YQ , Yu XL , Chu J , Yang G , The diagnostic value of contrast-enhanced ultrasound for cervical tuberculous lymphadenitis. Clin Hemorheol Microcirc. (2022) ;81: (1):69–79. doi: 10.3233/CH-211355 |
[6] | Shao S , Yao M , Li X , Li C , Chen J , Li G , Jia C , Wu R , Conventional and contrast-enhanced ultrasound features in sclerosing adenosis and correlation with pathology. Clin Hemorheol Microcirc. (2021) ;77: (2):173–81. doi: 10.3233/CH-200943 |
[7] | Troeltzsch D , Shnayien S , Gaudin R , Bressem K , Kreutzer K , Heiland M , Hamm B , Niehues S , Diagnostic performance of dynamic volume perfusion CT for differentiation of head and neck cancer from healthy tissue and post-therapeutic changes. Clin Hemorheol Microcirc. (2021) ;78: (1):93–101. doi: 10.3233/CH-200919 |
[8] | Novoa E , Gürtler N , Arnoux A , Kraft M , Role of ultrasound-guided core-needle biopsy in the assessment of head and neck lesions: a meta-analysis and systematic review of the literature. Head Neck. (2012) ;34: (10):1497–503. doi: 10.1002/hed.21821 |
[9] | Gritzmann N , Hollerweger A , Macheiner P , Rettenbacher T , Sonography of soft tissue masses of the neck. J Clin Ultrasound. (2002) ;30: (6):356–73. doi: 10.1002/jcu.10073 |
[10] | Todsen T , Ewertsen C , Jenssen C , Evans R , Kuenzel J , Head and Neck Ultrasound - EFSUMB Training Recommendations for the Practice of Medical Ultrasound in Europe. Ultrasound Int Open. (2022) ;8: (1):E29–34. doi: 10.1055/a-1922-6778 |
[11] | Groneck L , Quaas A , Hallek M , Zander T , Weihrauch MR , Ultrasound-guided core needle biopsies for workup of lymphadenopathy and lymphoma. Eur J Haematol. (2016) ;97: (4):379–86. doi: 10.1111/ejh.12742 |
[12] | Das DK , Francis IM , Sharma PN , Sathar SA , John B , George SS , Mallik MK , Sheikh ZA , Haji BE , Pathan SK , Madda JP , Mirza K , Ahmed MS , Junaid TA , Hodgkin’s lymphoma: diagnostic difficulties in fine-needle aspiration cytology. Diagn Cytopathol. (2009) ;37: (8):564–73. doi: 10.1002/dc.21064 |
[13] | Das DK , Value and limitations of fine-needle aspiration cytology in diagnosis and classification of lymphomas: A review. Diagn Cytopathol. (1999) ;21: (4):240–9. doi: 10.1002/(sici)1097-0339(199910)21:4<240::aid-dc3>3.0.co;2-z |
[14] | Nicol TL , Silberman M , Rosenthal DL , Borowitz MJ , The accuracy of combined cytopathologic and flow cytometric analysis of fine-needle aspirates of lymph nodes. Am J Clin Pathol. (2000) ;114: (1):18–28. doi: 10.1309/MN6J-4NJY-C5CG-1PLH |
[15] | Mitra S , Ray S , Mitra PK , Analysis of FNAC of cervical lymph nodes: experience over a three-year period. J Indian Med Assoc. (2013) ;111: (9):599–602. |
[16] | Rajbhandari M , Dhakal P , Shrestha S , Sharma S , Shrestha S , Pokharel M , Shrestha I , Shrestha B , Makaju R , The correlation between fine needle aspiration cytology and histopathology of head and neck lesions in Kathmandu University Hospital. Kathmandu Univ Med J (KUMJ). (2013) ;11: (44):296–9. doi: 10.3126/kumj.v11i4.12525 |
[17] | Pfeiffer J , Kayser L , Ridder GJ , Minimal-invasive core needle biopsy of head and neck malignancies: clinical evaluation for radiation oncology. Radiother Oncol. (2009) ;90: (2):202–7. doi: 10.1016/j.radonc.2008.10.018 |
[18] | Schelkun PM , Grundy WG , Fine-needle aspiration biopsy of head and neck lesions. J Oral Maxillofac Surg. (1991) ;49: (3):262–7. doi: 10.1016/0278-2391(91)90216-9 |
[19] | Chow LS , Gharib H , Goellner JR , van Heerden JA , Nondiagnostic thyroid fine-needle aspiration cytology: management dilemmas. Thyroid. (2001) ;11: (12):1147–51. |
[20] | Alexander EK , Heering JP , Benson CB , Frates MC , Doubilet PM , Cibas ES , Marqusee E , Assessment of nondiagnostic ultrasound-guided fine needle aspirations of thyroid nodules. J Clin Endocrinol Metab. (2002) ;87: (11):4924–7. doi: 10.1089/10507250152740993 |
[21] | Zhao D , Shao YQ , Hu J , Liu D , Tang W , He N , Role of contrast-enhanced ultrasound guidance in core-needle biopsy for diagnosis of cervical tuberculous lymphadenitis. Clin Hemorheol Microcirc. (2021) ;77: (4):381–9. doi: 10.3233/CH-201038 |
[22] | Hu Q , Naushad H , Xie Q , Al-Howaidi I , Wang M , Fu K , Needle-core biopsy in the pathologic diagnosis of malignant lymphoma showing high reproducibility among pathologists. Am J Clin Pathol. (2013) ;140: (2):238–47. doi: 10.1309/AJCP9ZAGKVJ8PDAX |
[23] | Gimeno-García AZ , Elwassief A , Paquin SC , Sahai AV , Endoscopic ultrasound-guided fine needle aspiration cytology and biopsy in the evaluation of lymphoma. Endosc Ultrasound. (2012) ;1: (1):17–22. doi: 10.7178/eus.01.004 |
[24] | Cheung YC , Wan YL , Lui KW , Lee KF , Sonographically guided core-needle biopsy in the diagnosis of superficial lymphadenopathy. J Clin Ultrasound. (2000) ;28: (6):283–9. doi: 10.1002/1097-0096(200007/08)28:6<283::aid-jcu3>3.0.co;2-t |
[25] | Kim BM , Kim EK , Kim MJ , Yang WI , Park CS , Park SI , Sonographically guided core needle biopsy of cervical lymphadenopathy in patients without known malignancy. J Ultrasound Med. (2007) ;26: (5):585–91. doi: 10.7863/jum.2007.26.5.585 |
[26] | Kraft M , Laeng H , Schmuziger N , Arnoux A , Gürtler N , Comparison of ultrasound-guided core-needle biopsy and fine-needle aspiration in the assessment of head and neck lesions. Head Neck. (2008) ;30: (11):1457–63. doi: 10.1002/hed.20891 |
[27] | Screaton NJ , Berman LH , Grant JW , Head and neck lymphadenopathy: evaluation with US-guided cutting-needle biopsy. Radiology. (2002) ;224: (1):75–81. doi: 10.1148/radiol.2241010602 |
[28] | Yamashita Y , Kurokawa H , Takeda S , Fukuyama H , Takahashi T , Preoperative histologic assessment of head and neck lesions using cutting needle biopsy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2002) ;93: (5):528–33. doi: 10.1067/moe.2002.123867 |
[29] | Oh KH , Woo JS , Cho JG , Baek SK , Jung KY , Kwon SY , Efficacy of ultrasound-guided core needle gun biopsy in diagnosing cervical lymphadenopathy. Eur Ann Otorhinolaryngol Head Neck Dis. (2016) ;133: (6):401–4. doi: 10.1016/j.anorl.2016.01.013 |
[30] | Ho UC , Chen CN , Lin CY , Hsu YC , Chi FH , Chou CH , Chen TC , Wang CP , Lou PJ , Ko JY , Hsiao TY , Yang TL , Application of ultrasound-guided core biopsy to minimize the non-diagnostic results and the requirement of diagnostic surgery in extrapulmonary tuberculosis of the head and neck. Eur Radiol. (2016) ;26: (9):2999–3005. doi: 10.1007/s00330-015-4159-4 |
[31] | Werner JM , Zidek M , Kammerer S , da Silva NPB , Jung F , Schlitt HJ , Hornung M , Jung EM , Intraoperative contrast-enhanced ultrasound can have a crucial role in surgical decision-making during hepato-pancreatico-biliary surgery - Analysis of impact and input. Clin Hemorheol Microcirc. (2021) ;78: (1):103–16. doi: 10.3233/CH-201031 |
[32] | Mu WN , Li JH , Liu Y , Liang HQ , Liu X , Comparative study of core needle biopsy and fine needle aspiration in the treatment of metastatic lymph nodes guided by contrast-enhanced ultrasound. Pak J Med Sci. (2022) ;38: (6):1477–82. doi: 10.12669/pjms.38.6.5471 |
[33] | Burke C , Thomas R , Inglis C , Baldwin A , Ramesar K , Grace R , Howlett DC , Ultrasound-guided core biopsy in the diagnosis of lymphoma of the head and neck. A 9 year experience. Br J Radiol. (2011) ;84: (1004):727–32. doi: 10.1259/bjr/60580076 |
[34] | Pedersen OM , Aarstad HJ , Løkeland T , Bostad L , Diagnostic yield of biopsies of cervical lymph nodes using a large (14-gauge) core biopsy needle. APMIS. (2013) ;121: (12):1119–30. doi: 10.1111/apm.12058 |
[35] | Carbone A , Ferlito A , Devaney KO , Rinaldo A , Ultrasound-guided core-needle biopsy: is it effective in the diagnosis of suspected lymphomas presenting in the head and neck? J Surg Oncol. (2008) ;98: (1):4–5. doi: 10.1002/jso.21003 |
[36] | Ward ST , Shepherd JA , Khalil H , Freehand versus ultrasound-guided core biopsies of the breast: reducing the burden of repeat biopsies in patients presenting to the breast clinic. Breast. (2010) ;19: (2):105–8. doi: 10.1016/j.breast.2009.12.003 |
[37] | Bahn YE , Lee SK , Kwon SY , Kim SP , Sonographic appearances of mucosa-associated lymphoid tissue lymphoma of the submandibular gland confirmed with sonographically guided core needle biopsy. J Clin Ultrasound. (2011) ;39: (4):228–32. doi: 10.1002/jcu.20754 |
[38] | Youk JH , Kim EK , Kwak JY , Son EJ , Atypical papilloma diagnosed by sonographically guided 14-gauge core needle biopsy of breast mass. AJR Am J Roentgenol. (2010) ;194: (5):1397–402. doi: 10.2214/AJR.09.3699 |
[39] | Mauri G , Cova L , Tondolo T , Ierace T , Baroli A , Di Mauro E , Pacella CM , Goldberg SN , Solbiati L , Percutaneous laser ablation of metastatic lymph nodes in the neck from papillary thyroid carcinoma: preliminary results. J Clin Endocrinol Metab. (2013) ;98: (7):E1203–7. doi: 10.1210/jc.2013-1140 |
[40] | Mauri G , Cova L , Ierace T , Baroli A , Di Mauro E , Pacella CM , Goldberg SN , Solbiati L , Treatment of Metastatic Lymph Nodes in the Neck from Papillary Thyroid Carcinoma with Percutaneous Laser Ablation. Cardiovasc Intervent Radiol. (2016) ;39: (7):1023–30. doi: 10.1007/s00270-016-1313-6 |
[41] | Guang Y , Luo Y , Zhang Y , Zhang M , Li N , Zhang Y , Tang J , Efficacy and safety of percutaneous ultrasound guided radiofrequency ablation for treating cervical metastatic lymph nodes from papillary thyroid carcinoma. J Cancer Res Clin Oncol. (2017) ;143: (8):1555–62. doi: 10.1007/s00432-017-2386-6 |
[42] | Wu W , Jing X , Xue GQ , Zhu XL , Wang J , Du RQ , Lv B , Wang KF , Yan JP , Zhang ZY , Li MD , Kono Y , Yan K , A Multicenter Randomized Controlled Study of Contrast-enhanced US versus US-guided Biopsy of Focal Liver Lesions. Radiology. (2022) ;305: (3):721–8. doi: 10.1148/radiol.212317 |
[43] | Zhou D , Zhang Y , Chen W , Jiang J , Chen Y , Zhou X , Tang Q , Enhanced ultrasound-guided versus non-enhanced ultrasound-guided percutaneous needle biopsy in tissue cellularity of lung malignancies: a propensity score matched study. Quant Imaging Med Surg. (2022) ;12: (11):5056–67. doi: 10.21037/qims-22-119 |
[44] | Cao X , Liu Z , Zhou X , Geng C , Chang Q , Zhu L , Feng W , Xu T , Xin Y , Usefulness of real-time contrast-enhanced ultrasound guided coaxial needle biopsy for focal liver lesions. Abdom Radiol (NY). (2019) ;44: (1):310–7. doi: 10.1007/s00261-018-1713-y |
[45] | Fan P , Cao J , Jin Y , Han H , Wang W , Xu H , Ji Z , Efficacy of contrast-enhanced ultrasound-guided percutaneous core needle biopsy in anterior mediastinal masses. J Interv Med. (2022) ;5: (3):159–65. doi: 10.1016/j.jimed.2022.04.006 |



