Abstract
Denmark implemented early widespread social distancing to reduce pressure on the healthcare system from the coronavirus disease 2019 (COVID-19) pandemic, with the aims to reduce mortality. Unintended consequences might be delays in treatment for other diseases and subsequent mortality. We examined national all-cause mortality comparing weeks 1–27 in 2020 and 2015–2019. This registry-based study used Danish national registry data until 5 July 2020. We examined all-cause mortality rates among all deaths recorded from 2015 to 2020 and among chronic conditions (cardiovascular (cardiac & circulatory), chronic pulmonary, chronic kidney disease, cancer, and diabetes), comparing each week in 2020 to weeks in 2015–2019. In 2020, there were 28,363 deaths in weeks 1–27 (30 December 2019–5 July 2020), the mean deaths in 2015–2019 were 28,630 deaths (standard deviation 784). Compared to previous years, the mortality rate in weeks 3–10 of 2020 was low, peaking in week 14 (17.6 per 100,000 persons in week 9, 19.9 per 100,000 in week 14). Comorbidity prevalence among deceased individuals was similar in 2020 and 2015–2019: 71.1% of all deceased had a prior cardiovascular diagnosis, 30.0% of all deceased had a prior cardiac diagnosis. There were 493 deaths with COVID-19 in weeks 11–27, (59.8% male), and 75.1% had a prior cardiovascular diagnosis. Weekly mortality rates for pre-existing chronic conditions peaked in week 14, and then declined. During the COVID-19 pandemic, due to timely lockdown measures, the mortality rate in Denmark has not increased compared to the mortality rates in the same period during 2015–2019.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic puts pressure on healthcare systems across the world, with 6.1% percent of cases in China classified as critical, and 12% of cases in Northern Italy requiring intensive care treatment [1]. Despite having above the European average of both critical care beds and physicians, the Italian healthcare system has been under pressure, with an 8-fold increase in pressure from 11 to 25 March 2020 [2]. In addition to the mortality due to COVID-19 itself (case fatality rate of 7.2% reported in Italy [3]), there may be indirect effects of COVID-19 on mortality. Indirect effects include changes in timely healthcare usage by patients and concerns about “bothering the doctor” [4, 5]. In addition, changes in treatment offered (when and if) for certain conditions (such as cardiac conditions) may also worsen patients’ health: deterioration in patient condition caused by postponement of treatment must be weighed against the risk of contracting coronavirus in hospital following treatment [5]. Monitoring of total mortality is recommended, as not all deaths occur in hospitals [6]. Italy reports a 45% excess total mortality, highest in the North [7].
To delay the spread of COVID-19, thereby reducing healthcare systems pressure, and hopefully mortality, lockdowns and social distancing measures have been implemented in many countries, affecting half of the world’s population on the Twentieth of April 2020 [8]. In the course of the COVID-19 pandemic, changes in health seeking behaviours may have occurred, with people less likely to seek help and delaying in doing so: In Denmark the amount of contacts to the general practitioner decreased by up to 40% [9]. In Hong Kong, acute myocardial infarction patients took longer time to call after developing symptoms, compared to before coronavirus [4]. Contrary to expectations in a stressful time period, there were less admissions for acute myocardial infarction both in the United States and Hong Kong [4, 10, 11]. Following the outbreak in Northern Italy, while significantly less patients have been admitted with acute coronary syndrome [12], more out-of-hospital cardiac arrests occurred, with 77.4% of the excess cases having suspected or confirmed COVID-19 [13]. Concerning healthcare pressure, in a past flu pandemic hospitals experiencing a high surge of patients, had increased case fatality rates for stroke and acute myocardial infarction compared to those under less pressure [14].
Restrictions in Denmark were put in early [15]. The first coronavirus patient was identified on 27 February 2020 [16]. On 11 March most people (in both public and private sectors) were instructed to work from home and schools to close from 13 March latest [15], from 13 March elective surgery and all non-urgent consultations at hospital were postponed to pre-empt a surge due to coronavirus [17]. On 18 March gatherings of over 10 people were banned. More extensive lockdown measures were not put into force. A timeline of events from weeks 9–31 is available in online supplementary figure 1. On 27 April 8 a.m, there were 8698 individuals with confirmed coronavirus infections [18]. A gradual return to ordinary hospital care was announced on 13 April [19]. The first death happened on 11 March, by 27 April, 427 people had died [18]. According to the European Monitoring of excess mortality for public health action (EuroMOMO), mortality in Denmark has not been substantially increased (i.e. exceeded 4 Z-scores above expected deaths) during the outbreak [20].
Therefore, we examined the effect of lockdown on overall all-cause mortality, in comparison to previous years. In addition to overall mortality, we examined all-cause mortality by age group and gender, and among people with pre-existing chronic conditions, known to be more affected by COVID-19 [21], to see whether some groups were more affected by the lockdown.
Methods
Setting
Data from the Danish registries were used for a retrospective observational study. Included were all Danish residents from 29th December 2014 (start of week 1 of year 2015, per the International Organization for Standardization (ISO)) [22]. Data was available until 10th July 2020, due to the possibility of delays in registration of deaths in the Danish Civil Registration system, data to the end of week 27 (5th July) was used. I.e. for each year data were used from Monday in week 1 to Sunday in week 27. At the start of 2020, the Danish population was 5.82 million.
The Danish healthcare system is tax-funded and universal healthcare is provided to all citizens [23]. Following the pandemic outbreak, the healthcare system was reorganized, out-patient visits were converted to telemedicine or cancelled whenever possible, elective non-vital procedures were cancelled or postponed, emergency rooms and intensive care units were upgraded to care for the expected surge of patients with coronavirus [17].
Data sources
All residents in Denmark have a unique, personal civil registration number for administrative usage, which enables individual-level linkage between different national Danish registries. This study used data from: the Danish National Patient Registry, the Danish Civil Registration system and the Danish National Prescription Registry [23]. The Civil Population Registry registers date of birth, sex, migration status, municipality of residence, and date of death. Highest education level (until 2019) was available from the Danish Population education registry. The Prescription Registry holds information on every filled prescription from a Danish pharmacy, including date and Anatomical Therapeutic Chemical (ATC) code [23]. The Danish National Patient Registry holds information on every hospitalization in Denmark since 1977, with diagnosis codes for every hospital contact (in- and out-patient diagnosis codes and dates and times) according to the International Classification of Disease, Tenth Revision (ICD-10 codes) [24].
Variables
Covariates
Age and sex were obtained from the Danish Civil registration system. Residence in one of the five Danish regions was obtained through collation of the last municipality of residence after 2007 (data available until 2019) [25]. Chronic conditions were based on all-time hospital contacts (in-patient or outpatient, A- or B-diagnoses) recorded in the Danish National Patient Registry since 1977, conditions were: Cardiac diseases, other circulatory diseases, any cancer (except non-melanoma skin cancer), chronic pulmonary diseases (asthma, COPD, and interstitial lung diseases), diabetes, and chronic kidney disease, see Table 1 for details. Cardiac diseases and other circulatory diseases were also combined as “cardiovascular disease”. For diabetes we also considered having ever had a prescription for an antidiabetic medication, ATC A10. For hypertension we also considered having redeemed prescriptions for at least two antihypertensive medications within 180 days before the 1st of January each year [26]. All conditions were considered permanent, except cancer where only diagnoses ≤ 10 years ago were considered [27]. Week numbers were calculated using the ISO 8601 standard [22], where weeks start on a Monday. Coronavirus diagnoses (starting date of in- or outpatient contact with COVID-19 diagnosis) were also identified from the Danish National Patient Registry (ICD-10: B34.2, B97.2), if this had been registered following microbiological testing.
Outcomes
Deaths occurring within 30 days of COVID-19 diagnosis were counted as deaths with COVID-19, in line with the definition used by Statens Serum Institut (SSI, institute within the Danish Ministry of Health that monitors infectious diseases) [18]. Additionally, deaths occurring more than after 30 days after COVID-19 diagnosis were reported. This definition required that a ICD-10 diagnosis code for COVID-19 had been registered following hospital contact (in-patient or out-patient), therefore positive test results in the community and subsequent deaths (without hospital contact) were not captured by this definition; however these deaths are still counted in the total deaths for each week, although there may be delays in ascertainment.
Statistics
Person characteristics were presented by year for all deaths from 29 December 2014 to 5 July 2020. Age was categorized, and categorical variables were summarized with percentages. Sex and age group distribution was presented for the entire Danish population at the beginning of 2015-2020, and comorbidities for the entire Danish population at the beginning of 2020. Descriptive statistics were also presented, by sex, for all patients who had died within 30 days of COVID-19 diagnosis.
The weekly mortality rates were calculated by dividing the number of deaths during the week by the number of persons alive at the beginning of the week and reported as number of events per 100,000 persons. These rates were reported for the entire population, and the population divided by sex and age, and sex and comorbidities (with incidence of new comorbidities counted from the following first whole week), and by region of residence. The proportion of deaths with comorbidities among all deaths was calculated for each week.
Among the dead in weeks 1–27 of years 2015–2019 and 2020 all possible combinations of four comorbidities (cardiovascular disease, chronic pulmonary disease, cancer and kidney disease) were counted. For each combination, the percentage of total mortality in each date range was also calculated.
Data management and analyses were performed with R [28].
Results
Mortality in 2015–2020
296,789 deaths occurred from 29th December 2014 to 10 July 2020, 32 were excluded due to ambiguous dates of death, and 477 deaths occurred in week 28 of 2020, leading to 296,280 deaths included. A total of 28,363 deaths were identified between 28 December 2019 and 5 July in 2020 (weeks 1–27). In 2015–2019 between 27,887 and 29,948 deaths occurred in weeks 1–27, mean 28,630 deaths, standard deviation 784 (Table 2). The age at time of death was comparable across years, with on average 50.8% ≥ 80 at time of death.
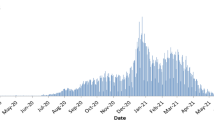
In Fig. 1 the rate of deaths observed in weeks 1–27 of 2020 is shown with rates in 2015–2019. The highest mortality rate in the years 2015–2020 rate was 23.1 per 100,000 and occurred in week 10 of 2018. In 2020, the overall rate of deaths in weeks 3–10 was low, the lowest was in week 9 (17.6 per 100,000), rising to 19.9 per 100,000 in week 14. In weeks 16 and 17 in 2020 the overall death rate was higher than previous years. Investigating the mortality rate by sex and age groups, in 2020 deaths rates in men aged 65-79 were highest in weeks 13–15 (59.9 per 100,000 in week 14). Death rates in men ≥ 80 years in 2020 were 191 per 100,000 in week 9 and 270 per 100,000 in week 13 (Fig. 2).
Mortality rates, divided by sex and age groups, in weeks 1–27 in 2020 compared to years 2015–2019. Grey lines are individual years. Vertical lines at weeks 9 and 11 indicate the first coronavirus case and lockdown measures, respectively. Years and week numbers according to the ISO 8601 standard. (i.e. 3 days in 2014 included in week 1 of 2015). The blue shaded space represents deaths with COVID-19, only displayed for > 3 deaths per week. Note, different Y-axis scale for different age-groups. Table lists the population distribution of sex and age groups in week 1 of each year, deaths in parentheses
Comorbidities
Generally small differences between each year from 2015 to 2020 were identified in the proportion of people dying with comorbidities. The proportion of people in 2020 dying with pre-existing conditions including cardiac disease, other circulatory diseases, cancer diagnoses ≤ 10 years ago, chronic kidney disease, chronic pulmonary disease, and diabetes was found to be very similar to those observed from the previous years (Table 2). The scatter-pie chart in Fig. 3 illustrates the combination of the pre-existing conditions among people dying in 2020 and the averaged combination observed for 2015–2019 in the same weeks. Cardiovascular disease appeared often in combination with other conditions, on its own it was the single most common disease in both populations (30.0% in 2020 and 29.7% in 2015–2019). In 2020 12.2% of people died without one of the specified comorbidities, in 2015–2019 this figure was 12.1%.
Combinations of pre-existing comorbidities in patients dead in weeks 1–27, 2020 compared to the average of years 2015–19. Each circle’s area represents the amount of people in this combination of conditions. Each person only appears once, in the circle corresponding to their combinations of comorbidities. Percentages are percentages of the total deaths (of the averages in 2015–2019) and of the total for 2020. The segmentation of the circles shows the amount of conditions in this combination, and the colours show the chronic conditions in question. Average number of deaths in 2015–2019:28,630.2, deaths in 2020: n = 28,363 deaths
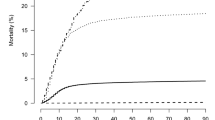
The weekly rate of deaths was equally examined in subgroups of pre-existing comorbidities and sex (Fig. 4). There were fluctuations in the weekly mortality rates, both before and after the first case of COVID-19. While chronic kidney disease was uncommon among the general population, the mortality rate was generally high and variable, with 47 deaths in week 9 and 62 deaths in week 10 among ~ 29,100 males resulting in 162 and 213 deaths per 100,000, similar variations were seen in females (Fig. 4). Among men with cardiac, chronic kidney or chronic pulmonary disease, lower mortality was seen in week 9, compared to preceding weeks, and followed by a subsequent rise. The most recent peak mortality rate was in week 14 for all comorbidities, followed by a gradual decline.
Mortality rates in weeks 1–27 in for patients with pre-existing chronic conditions in. Incident cases only counted at the start of the next whole week. Vertical lines at weeks 9 and 11 indicate the first coronavirus case and lockdown measures, respectively. Week numbers according to the ISO 8601 standard (i.e. week 1 of 2020 starts on 30 December). The blue shaded space represents deaths with COVID-19, only displayed for > 3 deaths per week. Note, different sum than in Table 2, due to only counting incident cases in the following week. Also note different Y-axis scales for the rows
The proportion of comorbidities among deaths in each week is shown in online supplementary figure 2, with the biggest variation seen in women with chronic pulmonary disease from the lowest value in week 4 to highest in week 5, followed by a gradual downward descent.
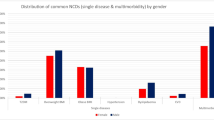
COVID-19 related deaths
There were 493 deaths after 30 days where the deceased had a coronavirus diagnosis. Pre-existing comorbidities were common, with only 11.0% of patients not having had a condition. 75.1% of patients had a prior diagnosis of a cardiovascular disease. Diabetes and peripheral vascular disease were more common among men than women (Table 3). An additional 86 individuals died more than 30 days after COVID-19 diagnosis. The distribution of deaths by region varied: of the 493 deaths within 30 days of COVID-19 diagnosis, 275 deaths occurred in the Capital region of Denmark and 62 Region Zealand corresponding to 3.4% and 2.1% of all deaths respectively in weeks 1–27. In the North Denmark Region 19 deaths occurred (0.62% of deaths in weeks 1–27) (Online supplementary figure 3).
Discussion
This nationwide study examined all-cause mortality following the first case of COVID-19 and subsequent lockdown and social distancing measures, as part of national strategies to prevent the spread of SARS-CoV-2. We compared the first 27 weeks of 2020 to the same weeks in years 2015–2019.
Our study showed that the overall weekly mortality has to date (5 July) only slightly exceeded mortality rates in all the previous 5 years in weeks 14–17. In the subgroup of the population of males 65–79 and ≥ 80 slight increases in death rates were observed from week 9 to 15, but still similar to rates in previous years. Despite this small change, it did not have an effect of overall causing excess mortality in the population, even though other studies have found that elderly men are at increased risk of death [7]. There was no marked change in death rates among those with comorbidities, which following a peak declined gradually, suggesting that no collateral damage has occurred due to lockdown, or restrictions in hospital services. Most deaths following a coronavirus diagnosis were among older males, with multiple comorbidities.
That Danish mortality is currently not in excess, is confirmed by EuroMOMO, who show that mortality in Denmark has not exceeded 4 Z-scores above expected deaths during the outbreak [20]. A recent publication from the EuroMOMO group mentions Denmark as one of the European countries with little or no excess mortality [29]. It appears that government policies towards social distancing and changes in individual behaviour were timely in Denmark. According to SSI, social distancing measures in Denmark had the immediate effect of reducing the prevalence of flu: while similar amounts of people were tested in weeks 11 (when social distancing measures were implemented) and 12, a lower percentage of tests were positive (20% and 7% in weeks 11 and 12, respectively) and the incidence of flu fell from 884 to 260 [30]. Social distancing measures have been reported as being effective in Asia, to flatten the epidemic curve [31].
One consequence of the lockdown is less movement of people. One Danish hospital, compared accidents in March/April to March/April last year, half as many people have been at hospital due to an accident (at home, in school/at work, in traffic) [32], which may explain changes in mortality.
In Denmark, in March 2020 after lockdown, fewer cases of new-onset atrial fibrillation (47%) and heart failure (30%) have been diagnosed [33, 34]. For patients with pre-existing heart failure, there were less hospitalizations for worsening heart failure after lockdown; the authors report that 90 heart failure patients (0.08% of all diagnosed heart failure patients in Denmark) contracted COVID-19, following which 25 died (37%, 95% CI 23–50%) [33]. In the months since lockdown we find the overall mortality for pre-existing comorbidities and proportion of deaths with pre-existing comorbidities to be within a similar range, suggesting that collateral damage due to changes in health-care utilization or pressure has yet to happen.
Yearly variations in seasonal mortality are apparent in our data, likely caused by weather extremes and influenza outbreaks. The high mortality in week 9–10 of spring 2018 is possibly explained by high influenza prevalence, with 2822 deaths between week 40 in 2017 and week 20 in 2018 estimated to be caused by Influenza (Influenza B and A H1N1) [35]. Corresponding estimated excess mortality figures for weeks 40–20 of 2016/2017 were 751 and in 2018/19 790. In weeks 40–20 of 2019/2020 only 97 people died within 30 days of a positive influenza test, leading to estimates of 119 (interval 41–196) excess deaths due to influenza [36]. This lower excess mortality due to influenza in 2020 likely explains the lower mortality in the beginning of 2020 in our study. One group working with flu outbreaks and pooled European data concluded that excess mortality in Spring 2018 was mainly attributable to flu, but also to concurrent low average temperatures [37].
While pursuing the case fatality rate of COVID-19 infection is important, it requires knowing the amount of people infected [31]. Given that many cases of COVID-19 infection are asymptomatic, this is likely difficult to calculate. Based on data from the Diamond Princess cruise ship, the case fatality rate has been estimated as being 2.6%, while the infection fatality rate has been estimated as 1.3% as approximately half of individuals who tested positive were asymptomatic and thus would only contribute to the infection fatality rate, and not the case fatality rate if they had not been tested [38]. In Denmark serology in mid-April has revealed that overall 4.04% of tested healthcare workers in the Capital Region appear to have developed antibodies [39]. Test results of Danish blood donors (17–69 years), donating blood from 6 April–3 May, indicate that the overall seroprevalence of COVID-19 in Denmark is 1.9 (C.I. 0.8–2.3), highest in the Capital region (3.2%) compared to other regions (1.2%), difference 2.0%, CI for difference 1.4–2.6 [40]. This is reflected by the higher mortality after COVID-19 diagnosis in the Capital Region in our results. The total positive confirmed swab tests were 3355 on 2 April and 7912 on 22 April [41, 42], Denmark’s population is 5.82 million. A representative sample of the Danish population was drawn, of which 1071 participated, estimating the seroprevalence of COVID-19 antibodies (until May) to be between 0.5 and 1.8% in the general population [43].
Strategies, testing, and mortality differed in Scandinavia. Denmark (population 5.8 million) tested 104,580 in week 27, Sweden (population 10.3 million) tested 75,151 in week 26, and Finland (population 5.4 million) tested 17,777. In week 26 (inclusive) total tests were ~ 1.04 million in Denmark (~ 180,000 tests per million), and ~ 0.52 million in Sweden (~ 50.5 tests per million) [44,45,46]. The Oxford COVID-19 Government Response Tracker (OxCGRT) has related stringency of government policies relative to case amounts. They show that Denmark & Finland had implemented more stringent control measures than Sweden, and more rapidly reaching their maximal levels after identification of the first case [47]. By 6 August Denmark had recorded 14,185 cases and 616 deaths, Sweden 81,540 cases and 5760 deaths, Finland 7512 cases and 331 deaths [48]. Even since the gradual societal reopening Danes still exhibit the appropriate behaviour (avoiding hugs/kisses, cough in elbow, use alcogel, stay home if sick, maintain distance), with high degrees of knowledge efficacy; however through July the amount of close contacts (<1m distance) lasting over 15 min has increased to 8–9 per fortnight, and Danes experience that fellow citizens are less compliant to the recommendations [49]. Since release on 18 June the Danish COVID-19 smartphone app has been downloaded more than 824,000 times. 209 people have notified the app of infection, leading to at least 48 people being notified of possible exposure to an infected individual [50].
Excess all-cause mortality may be a better estimate for the pandemic’s mortality in the setting of limited testing and many asymptomatic cases. EuroMOMO report that overall, the total deaths in Europe exceeded the level of an “substantial increase” in weeks 11–20, with overall excess deaths reported from weeks 9 to 22 and again in 26–27 [51]. A comparison has been made between historical mortality in countries across the world and deaths with COVID-19, but also excess deaths, which estimates that 36,000 (as of 23 April 2020) more deaths have occurred following COVID-19 than those figuring in official reports for COVID-19—which might be either COVID-19 deaths or people unable to get treated for other diseases [52].
Strengths and limitations
Strengths were the database quality, reported with limited delays
Limitations were that we used registered diagnosis of pre-existing comorbidities and not causes of death, on death certificates, which were unavailable. For deaths in patients with coronavirus, coronavirus is not necessarily the primary cause of death, but a contributing part, however review of death certificates, by another group, for the first 278 Danish deaths with COVID-19 indicate that only one patient likely died due to another cause [53]. We did not have actual test results from the Danish Microbiology database, only diagnoses from the Danish National Patient Registry. At the end of 5 July, we could count 493 deaths with COVID-19; however, the figures released from SSI show 607 deaths counted on 5 July [18]. Comparison of weekly deaths with COVID-19 to SSI’s data indicate that we are underreporting between 8 and 23 deaths with COVID-19 per week in weeks 13–19, and 1–5 in weeks 11–12 and 20–27, on average 7 less deaths per all weeks [54]. An explanation could be that general practitioners may order the test [55], if the patient is otherwise not in contact with the hospital, the diagnosis of COVID-19 will not be visible in the Danish National Patient Registry.
Conclusion
During the COVID-19 epidemic we found that the total number of deaths in Denmark in the first half of 2020 has not increased above the observed number of deaths in the same period during 2015–2019. Comorbidities among the deceased were comparable, and there were no changes in mortality in those with pre-existing chronic conditions.
References
Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–17. https://doi.org/10.1016/S2213-2600(20)30161-2.
Verelst F, Kuylen E, Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases. Eurosurveillance. 2020;25:2000323. https://doi.org/10.2807/1560-7917.ES.2020.25.13.2000323.
Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–6. https://doi.org/10.1001/jama.2020.4683.
Tam C-CF, Cheung K-S, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment–Elevation Myocardial Infarction Care in Hong Kong. China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. https://doi.org/10.1161/CIRCOUTCOMES.120.006631.
Rosenbaum L. The Untold Toll—The Pandemic’s Effects on Patients without Covid-19. N Engl J Med. 2020. https://doi.org/10.1056/NEJMms2009984.
ECDC (2020) Strategies for the surveillance of COVID-19. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-surveillance-strategy-9-Apr-2020.pdf. Accessed 25 May 2020.
Michelozzi P, De’Donato F, Scortichini M, et al. Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: rapid mortality surveillance system, Italy. Euro Surveill. 2020;25:1–5. https://doi.org/10.2807/1560-7917.ES.2020.25.19.2000620.
AFP (2020) Europe plans slow reopening, New York passes peak in virus battle. In: AFP. https://www.afp.com/en/news/3954/europe-plans-slow-reopening-new-york-passes-peak-virus-battle-doc-1qo9l25. Accessed 22 Apr 2020.
Lange Olsen T, Olsgaard G (2020) Markant færre sendes til kræfttjek på hospitaler: “Det er potentielt ret alvorligt det her.” In: DR. https://www.dr.dk/nyheder/indland/markant-faerre-sendes-til-kraefttjek-paa-hospitaler-det-er-potentielt-ret-alvorligt. Accessed 6 May 2020.
Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
Solomon MD, McNulty EJ, Rana JS, et al (2020) The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N Engl J Med NEJMc2015630. https://doi.org/10.1056/NEJMc2015630.
De Filippo O, D’Ascenzo F, Angelini F, et al (2020) Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med NEJMc2009166. https://doi.org/10.1056/NEJMc2009166.
Baldi E, Sechi GM, Mare C, et al (2020) Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N Engl J Med NEJMc2010418. https://doi.org/10.1056/NEJMc2010418.
Rubinson L, Mutter R, Viboud C, et al. Impact of the fall 2009 influenza A(H1N1)pdm09 pandemic on US hospitals. Med Care. 2013;51:259–65. https://doi.org/10.1097/MLR.0b013e31827da8ea.
(2020) Nye tiltag mod COVID-19, pressemøde 11. marts. In: Regeringen (Danish Gov. https://www.regeringen.dk/nyheder/2020/pressemoede-11-marts-i-spejlsalen/. Accessed 27 Apr 2020.
Statens Serum institut (2020) Første dansker testet positiv for COVID-19. https://www.ssi.dk/aktuelt/nyheder/2020/02_27_foerste-tilfaelde-af-ny-coronavirus-i-dk. Accessed 17 Apr 2020.
Sundhedsstyrelsen (2020) Notat om reduktion af hospitalsaktivitet ifm COVID-19. https://www.sst.dk/-/media/Udgivelser/2020/Corona/Hospitalskapacitet/Notat-om-reduktion-af-hospitalsaktivitet-ifm-med-COVID-19. Accessed 16 Apr 2020.
Staten Serum Institut (2020) COVID-19 i Danmark, Epidemiologisk overvågningsrapport 27 April. https://files.ssi.dk/COVID19-overvaagningsrapport-27042020-ce23. Accessed 11 May 2020.
Sundhedsstyrelsen (2020) Håndtering af COVID-19: Plan for omstilling og gradvis øget aktivitet i Sundhedsvæsenet. https://www.sst.dk/-/media/Udgivelser/2020/Corona/Haandtering-af-COVID-19/Haandtering-af-COVID-19_omstilling-og-oeget-aktivitet-i-Sundhedsvaesenet. Accessed 17 Apr 2020.
Statens Serum institut (2020) Dødsfald i Danmark, undtaget Grønland og Færøerne. In: EuroMOMO. https://www.ssi.dk/-/media/arkiv/dk/sygdomme-beredskab-og-forskning/sygdomsovervaagning/momo/dk_momo.pdf?la=da. Accessed 11 Aug 2020.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3.
Hocken V (2020) Are There 52 or 53 Weeks in a Year ? In: Time date.com. https://www.timeanddate.com/date/week-numbers.html. Accessed 20 Apr 2020.
Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–91. https://doi.org/10.2147/CLEP.S179083.
Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83. https://doi.org/10.1186/1471-2288-11-83.
Danmarks Statistik (2007) Regioner, landsdele og kommuner, v1:2007. https://www.dst.dk/da/Statistik/dokumentation/nomenklaturer/regioner–landsdele-og-kommuner. Accessed 26 Jul 2020.
Olesen JB, Lip GYH, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. https://doi.org/10.1136/bmj.d124.
Hvidberg MF, Johnsen SP, Glümer C, et al. Catalog of 199 register-based definitions of chronic conditions. Scand J Public Health. 2016;44:462–79. https://doi.org/10.1177/1403494816641553.
Core Team R. R: A language and environment for statistical computing. Vienna: Austria; 2019.
Vestergaard LS, Nielsen J, Richter L, et al. Excess all-cause mortality during the COVID-19 pandemic in Europe – preliminary pooled estimates from the EuroMOMO network. Eurosurveillance. 2020;25(26):2001214. https://doi.org/10.2807/1560-7917.ES.2020.25.26.2001214.
Statens Serum institut (2020) Markant fald i influenza i de seneste to uger Markant fald i influenza i de seneste to uger. In: Statens Serum Inst. Nyheder. https://www.ssi.dk/aktuelt/nyheder/2020/03-markant-fald-i-influenza-i-de-seneste-to-uger-31032020. Accessed 23 Apr 2020.
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–4. https://doi.org/10.1016/S0140-6736(20)30567-5.
Jensen KB (2020) Efter coronalukning : Halvt så mange danskere på skadestuen efter ulykker. In: Ugeskr. Laeger. https://ugeskriftet.dk/nyhed/efter-coronalukning-halvt-sa-mange-danskere-pa-skadestuen-efter-ulykker. Accessed 8 Apr 2020.
Andersson C, Gerds T, Fosbøl E, et al. Incidence of New-Onset and Worsening Heart Failure Before and After the COVID-19 Epidemic Lockdown in Denmark: A Nationwide Cohort Study. Circ Heart Fail. 2020;13:e007274. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007274.
Holt A, Gislason GH, Schou M, et al (2020) New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J 1–8. https://doi.org/10.1093/eurheartj/ehaa494.
Statens Serum institut (2019) Infuenza season 2018/19. https://en.ssi.dk/surveillance-and-preparedness/surveillance-in-denmark/annual-reports-on-disease-incidence/influenza-season-2018-2019. Accessed 16 Apr 2020.
Statens Serum institut (2020) Influenzasæsonen - opgørelse over sygdomsforekomst 2019/2020. https://www.ssi.dk/sygdomme-beredskab-og-forskning/sygdomsovervaagning/i/influenzasaesonen—opgoerelse-over-sygdomsforekomst-2019-20. Accessed 8 May 2020.
Nielsen J, Vestergaard LS, Richter L, et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season: should the burden of influenza B be reconsidered? Clin Microbiol Infect. 2019;25:1266–76. https://doi.org/10.1016/j.cmi.2019.02.011.
Russell TW, Hellewell J, Jarvis CI, et al. Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship. Eurosurveillance. 2020. https://doi.org/10.2807/1560-7917.ES.2020.25.12.2000256.
Iversen K, Bundgaard H, Hasselbalch RB, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020;2:3–10. https://doi.org/10.1016/S1473-3099(20)30589-2.
Erikstrup C, Hother CE, Pedersen OBV, et al (2020) Estimation of SARS-CoV-2 infection fatality rate by real-time antibody screening of blood donors. Clin Infect Dis 2020:ciaa849. https://doi.org/10.1093/cid/ciaa849.
Statens Serum institut (2020) COVID-19 i Danmark 2 April. In: Epidemiol. overvågningsrapport. https://files.ssi.dk/COVID19-overvaagningsrapport-02042020-kl45. Accessed 16 Apr 2020.
Statens Serum institut (2020) COVID-19 i Danmark 22 April. In: Epidemiol. overvågningsrapport. https://files.ssi.dk/covid19-overvaagningsrapport-22042020-lj45. Accessed 24 Apr 2020.
Statens Serum institut (2020) De første foreløbige resultater af undersøgelsen for COVID-19 i befolkningen er nu klar. https://www.ssi.dk/aktuelt/nyheder/2020/de-forste-forelobige-resultater-af-undersogelsen-for-covid-19-i-befolkningen-er-nu-klar. Accessed 20 May 2020.
Finnish Institute for Health and Welfare (2020) COVID-19-epidemian hybridistrategian seuranta – tilannearvioraportti 8.7.2020. https://thl.fi/documents/533963/5860112/COVID-19-epidemian+hybridistrategian+seuranta+–+tilannearvioraportti+8.7.2020_.pdf. Accessed 7 Aug 2020.
Folkhälsomyndigheten Tidigare data för antal individer som har testats för covid-19. In: Folkhälsomyndigheten. https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/genomforda-tester-for-covid-19/tidigare-data/. Accessed 5 Aug 2020.
Institut SS (2020) Testaktivitet (den 4. August 2020). In: Statens Serum Inst. https://files.ssi.dk/Test_table_04082020. Accessed 6 Aug 2020.
Hale T, Webster S, Petherick A, et al (2020) Oxford COVID-19 Government Response Tracker Regional report - Europe and Central Asia. In: Blavatnik Sch. Gov. https://raw.githubusercontent.com/OxCGRT/covid-policy-scratchpad/master/regional_reports/LatestEuropeCentralAsiaRegionalSummary.pdf. Accessed 7 Aug 2020.
ECDC (2020) COVID-19 situation update for the EU/EEA and the UK, as of 6 July 2020. https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea. Accessed 7 Aug 2020.
Lindholt MF, Jørgensen F, Bor A, Petersen MB (2020) COVID-19 Adfærdsindikatorer: Danskernes Smitteforebyggende Adfærd og Opfattelser. In: HOPE-Projektet (www.hope-project.dk). https://raw.githubusercontent.com/mariefly/HOPE/master/Danskernes_Smitteforebyggende_Adfærd_Og_Opfattelser_0804.pdf. Accessed 7 Aug 2020.
Sundheds- og ældreministeriet (2020) Appen smitte | stop er et effektivt redskab i smitteopsporing. 30 July. https://sum.dk/Aktuelt/Nyheder/Coronavirus/2020/Juli/Appen-smitte-stop-er-et-effektivt-redskab-i-smitteopsporing.aspx. Accessed 7 Aug 2020.
European Monitoring of excess mortality for public health action (2020) EuroMOMO Graphs and maps. In: EuroMOMO. https://www.euromomo.eu/graphs-and-maps. Accessed 11 Aug 2020.
Wu J, McCann A, Katz J, Peltier E (2020) 28,000 Missing Deaths: Tracking the True Toll of the Coronavirus Crisis. In: New York Times. https://www.nytimes.com/interactive/2020/04/21/world/coronavirus-missing-deaths.html?referringSource=articleShare. Accessed 23 Apr 2020.
Statens Serum institut (2020) COVID-19 i Danmark, Epidemiologisk trend og fokus: Dødelighed, 30. April 2020. https://files.ssi.dk/COVID19-epi-trendogfokus-30042020-61ls. Accessed 22 May 2020.
Statens Serum institut (2020) Deaths_over_time. https://files.ssi.dk/Data-epidemiologisk-rapport-06082020-hba1. Accessed 7 Aug 2020.
Sundhedsstyrelsen (2020) Information om PCR test for COVID-19 til almen praksis. https://www.sst.dk/-/media/Udgivelser/2020/Corona/IRF-Almen-praksis/Kommunikation-til-almen-praksis_test-af-COVID. Accessed 23 May 2020.
Funding
This study was supported by Grant Number R122-A8403, from the Danish Heart Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by C. Torp-Pedersen, M. Phelps, M. Andersen and T. Gerds. Analysis was performed by, and the first draft written by E. Mills, A. Møller, N. Zylyftari, B. Jensen and F. Gnesin and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Schou reports to have received lecture grants from Novo, Bohringer, Novartis and Astra Zeneca outside the clinical study. Dr. Køber reports personal fees from Novartis, AstraZeneca and Boehringer for presentations at meetings, outside the submitted work. Dr. Torp-Pedersen reports grants for studies from Bayer and Novo Nordisk.
Ethical approval
Registry-based studies do not require informed consent or ethical approval in Denmark. The reference number from the Data Responsibility institute in the Capital Region of Denmark was P-2019-191.
Availability of data, code and materials
Analyses were performed on Statistics Denmark’s secure database of registries, using pseudonymised data. Access is possible, upon reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mills, E.H.A., Møller, A.L., Gnesin, F. et al. National all-cause mortality during the COVID-19 pandemic: a Danish registry-based study. Eur J Epidemiol 35, 1007–1019 (2020). https://doi.org/10.1007/s10654-020-00680-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-020-00680-x