Introduction
The first four cases of what would later be called severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) infection, or COVID-19, were reported in Wuhan, China, on December 31, 2019 [1,2], although later studies indicate that individuals probably were infected earlier, perhaps even in November [Reference Wang, Wang, Zhang, Jia, Li and Dang3–Reference Ma5]. The nucleotide sequence of the virus was made public by a consortium of Chinese and Australian institutions on January 10, 2020 [Reference Holmes6], establishing the causative agent as a coronavirus with genetic similarities to SARS-CoV and Middle East Respiratory Syndrome (MERS). Although its mode of transmission was unclear, early anecdotal reports indicated that single patients could infect large numbers of health care workers, raising the likelihood that person-to-person spread could occur readily, which was confirmed by January 21, 2020 [Reference Wang, Horby, Hayden and Gao7]. Later, it was appreciated that asymptomatic individuals could spread the virus to large numbers of contacts outside of the health care setting [Reference Zhang, Wu and Xu8]. The first US case was reported in a traveler who returned to Washington State from Wuhan on January 15, 2020; the first European cases of COVID-19 were reported on January 24 in France [Reference Spiteri, Fielding and Diercke9]. The US partially restricted travel to the United States from China on January 30 and declared the disease a Public Health Emergency on January 31. On the same day federal officials ordered a 14-day quarantine for a group of 195 citizens repatriated from China, but did not restrict travel from Europe.
Based on the DNA sequence of the virus a polymeric chain reaction test to detect SARS-CoV-2 viral DNA was developed by German investigators at Berlin’s Charité Hospital [Reference Wieler, Rexroth and Gottschalk10] and later adopted by the WHO, but not by the US CDC or Food and Drug Administration (FDA). The CDC prepared its own test but encountered substantial delays, thus seriously limiting and delaying testing in the United States [Reference Kaplan11,Reference Ravi, Cortade, Ng and Wang12]. For example, the CDC website on March 1 indicated it could perform only 350 tests per day and that it had material for only 75,000 tests for the entire country. In contrast, by March 16, the WHO had already distributed 1.5 million tests to 120 countries [Reference Adhanom13]. Data from Italy, Japan, South Korea, and Iran in early March demonstrated the enormously rapid spread of the virus, which overwhelmed medical facilities and taxed health care professionals to their limits. The WHO declared COVID-19 a pandemic on March 11 and that was soon followed by outbreaks in New York, New Jersey, Connecticut, Massachusetts, and other states. For example, on March 2, the US reported just 16 new cases that day, but by March 30, it reported 21,469 new cases.
The Clinical and Translational Science Award (CTSA) Consortium’s Response
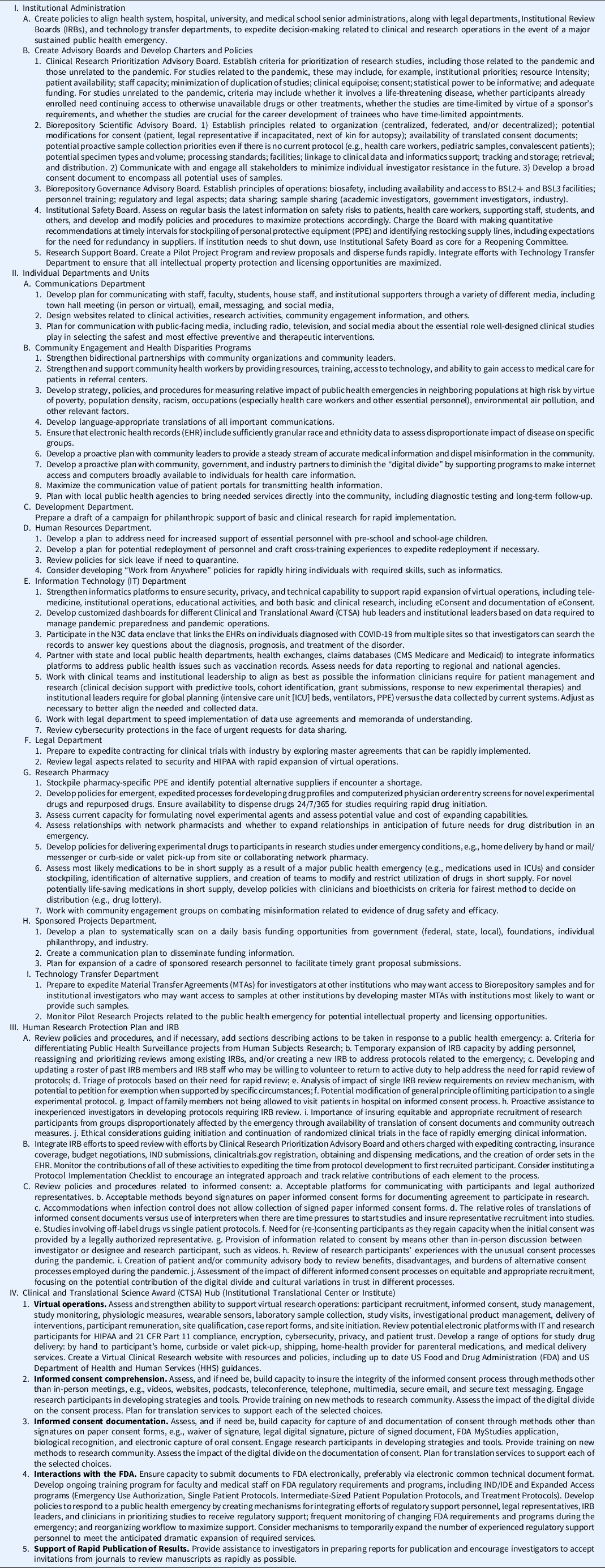
The National Institutes of Health (NIH) through its National Center for Advancing Translational Science (NCATS) supports approximately 60 academic hubs in its CTSA program. Nearly all of the CTSA hubs are affiliated with one or more health care systems across the country and are committed to the goal of enhancing national capacity, methods, and processes in clinical and translational research, focusing on the local needs of their communities. As the COVID-19 pandemic spread, the national CTSA Steering Committee devoted increasing attention to sharing best practices among CTSA sites as each hub addressed the challenges it faced in responding to the local manifestations of the pandemic, and as the Steering Committee collectively focused on advancing discovery and translational science targeting COVID-19 broadly. From those Steering Committee meetings emerged plans to capture the creative ideas developed by CTSA hubs in a series of papers focusing on different elements in the clinical research enterprise (Fig. 1). The outcome is this special issue of the Journal of Clinical and Translational Sciences.

Fig. 1. CTSAs and COVID-19. Major elements of the translational research enterprise at Clinical and Translational Award (CTSA) hubs and nationally related to the COVID-19 pandemic. FDA, US Food and Drug Administration; IRB, Institutional Review Board; N3C, National COVID Cohort Collaborative.
Each paper is flexibly organized by the following template:
-
1. What were the practices before the COVID-19 pandemic?
-
2. How were practices altered/redefined/modified/streamlined to address the challenges and exigencies of the COVID-19 pandemic?
-
3. What were the key lessons learned?
-
4. Which, if any, extraordinary practices developed as a response to COVID-19 should now become standard, and which, if any raised sufficient concerns that they should not be continued or perhaps even considered in the future in the face of a similar public health challenge?
-
5. If a similar public health challenge occurred in the future, what would be the sequence of actions you recommend to take in response?
We coupled this initiative with an extensive survey of the CTSA hubs created by the University of Rochester Center for Leading Innovation and Collaboration (CLIC) Survey Team by integrating the questions proposed by the each of the writing groups (Supplementary Table). A total of 60 hubs responded, providing robust data about measures that the hubs implemented, along with an assessment of best practices. The detailed results of the survey are included in the individual manuscripts. The most dramatic finding was that 87% of the CTSA hubs indicated that they were involved in creating institutional COVID-19-related governing policies, highlighting the importance of CTSAs in shaping the clinical research enterprise.
This theme issue of The Journal of Clinical Translational Science brings all of these papers together, and this paper provides a summary of the key recommendations proposed by the authors of each of the papers. We have focused our recommendations on things to do now (Table) based on the CTSA experience and best practices because careful planning now will facilitate and speed implementation of measures to address a future public health challenge. The same table should serve as a checklist if we are confronted with another public health emergency of comparable magnitude. In this way, we hope to provide a “playbook” as a resource for those called upon to lead the clinical research enterprise at their institution in response to new public local, regional, or global health crises.
The topics covered in Table 1 are wide ranging because major public health emergencies impact virtually every phase of research operations. The impact of COVID-19 on educational programs has been particularly profound, requiring an enormous effort to sustain trainees’ productivity. This topic is being addressed in a separate publication by the CTSA career and workforce development group [Reference McCormack, Bredella and Ingbar14]. Based on a survey of TL1 trainees and KL2 scholars, they found that lack of access to research facilities, clinics, team members, and human subjects, coupled with the need for homeschooling, were major challenges. Strategies to maintain research productivity involved trying to focus on writing, time management, virtual connections with colleagues, and shifting to research activities not requiring laboratory/clinic settings. They also described serious concerns by trainees and scholars that their decreased productivity during the pandemic might have a negative impact on their long-term research and career goals and their ability to obtain research funding. They offered a series of actions that programs, institutions, and the NIH can take to mitigate the impact of the pandemic on translational trainees and scholars.
Table 1. Things to do now and a Checklist for a future similar public health emergency
BSL, biosafety level; CMS, Centers for Medicare & Medicaid Services; CFR, Code of Feral Regulations; IND, Investigational New Drug; IDE, Investigational Device Exemption.
Many of the recommendations detailed in Table 1 are ones that are valuable to implement even without the threat of another public health emergency, highlighting that emergencies offer opportunities to garner broad support to implement things that would be beneficial under any conditions, but have faced one or more obstacles or have not risen to a high enough priority because of inertia. Some recommendations will require additional resources, which are likely to be in short supply as institutions face severe budgetary challenges, especially state medical schools that rely on public funds. This can potentially be balanced by an appeal for philanthropic support since the public now appreciates more than ever the vital role that translational research plays in protecting the health of the country and in developing novel diagnostic tests and therapies. The COVID-19 pandemic has provided the public with a thorough education in the roles of the NIH, FDA, and CDC, with otherwise esoteric topics such as Emergency Use Authorizations, and the statistical power of different clinical trial designs, now in the news on a regular basis. It has also more indirectly highlighted the crucial role of biomedical research, especially translational research, with vaccine development center stage in a way that has not occurred since the polio vaccine in the early 1950s [Reference Oshinsky15]. This provides opportunities to build on the public interest with sustained public educational programs about the role and importance of translational research more broadly. This will also provide an opportunity to highlight the crucial role of the CTSA program in responding to the pandemic and other important health needs.
The CTSA program houses a Trial Innovation Network (TIN) to coordinate multisite clinical studies. The TIN has championed a number of innovative projects to support multiple COVID-19 studies transitioning to remote operations and the Recruitment Innovation Center (RIC) assisted investigators in engaging diverse communities via virtual Community Engaged Studios. The TIN also has played a role in maximizing the amount of information that can be extracted from studies of hydroxychloroquine and convalescent plasma and is playing an important role in implementing several NIH-supported studies for COVID-19. Similarly, the CTSA program is actively supporting the National COVID-19 Cohort Collaborative (N3C), a major initiative to link the electronic health records (EHRs) from patients with COVID-19 into a single searchable data enclave to speed the identification of important diagnostic, prognostic, and treatment information. The details of these initiatives are beyond the scope of this manuscript, but they are vital elements in a comprehensive response.
Perhaps the single greatest failing of the US response to the pandemic has been the fragmentation of clinical trials into mostly institution-specific units that have not been informative because of failure to meet the required number of participants. There have been complex challenges in sizing and completing trials, including tremendous variability in caseloads over short periods of time at individual sites, so that by the time protocols became approved the number of infections in the community dropped below the number expected and required for timely recruitment. On the flip side, when caseloads are exploding, and institutions require all hands on deck, with redeployment to active patient care roles of every person who can contribute to this mission, assigning personnel to support clinical trial recruitment and conduct is likely to be viewed as a “luxury” that the institution cannot afford to support. There is also the tension between making novel therapies generally available through FDA Expanded Access programs based on strong theoretical grounds, such as the use of convalescent plasma, and wanting to conduct rigorous randomized controlled clinical trials to unequivocally assess the value of the therapy. These challenges are not new, being clearly delineated by Upton Sinclair in his 1925 novel Arrowsmith, which was informed by the 1918 influenza pandemic [Reference Eisenman16].
These challenges cry out for immediate design and implementation of nation-wide multisite trials to answer as many questions as possible to optimize medical management as rapidly as possible. As we are writing, NIH is undertaking such an effort in its ACTIV [17] and CONNECTS [18] programs, with the CTSA TIN participating in the ACTIV-1 trial [19]. A full review of the effectiveness of these programs relative to actions taken in other countries, in particular the U.K. RECOVERY trial [Reference Horby, Lim and Emberson20] and the ACCORD program [21], will provide valuable data for future planning. There is a need for national prioritization of the key scientific issues, and mechanisms to ensure adequate enrollment into the major studies by avoiding having multiple trials with overlapping enrolment criteria at many sites, and to prevent competition between NIH trials for sites and resources. Such an effort needs to extend beyond academic health centers to practice-based research networks if the largest number of people are to be enrolled in the shortest period of time and if the data are likely to be most generalizable. Now is the time to consider putting in place all of the necessary infrastructure, including the regulatory and legal documents and master protocols, as well as the organizational structure, that will allow for a true “turn-key” operation that can start enrollment within weeks of a major new public health emergency.
As an example, the lessons learned from the convalescent plasma therapy experience in the early phase of the COVID-19 pandemic indicate that the CTSA program as a consortium is ideally suited to rapidly develop a convalescent plasma program for future infectious disease challenges. By pooling resources and knowledge, it could rapidly in parallel: 1. Develop a high-throughput assay to measure antibody titers in convalescent plasma that correlate with viral neutralization. 2. Create a collection of validated biobank samples that could be used to analyze the sensitivity and specificity of the antibody assays. 3. Set up convalescent donor plasma collection centers in hub blood banks, regional blood collection facilities, and potentially in partnership with commercial plasma collection companies to obtain convalescent plasma anywhere in the country where the first convalescent patients reside, with distribution to sites around the country where it is needed most. Since it is crucial to obtain data from randomized studies to assess the potential benefits and risks of convalescent plasma, the CTSAs in collaboration with the TIN could create a master protocol, coupled with model subcontracts and a regulatory pathway, for rapid implementation in a future pandemic. Based on the currently available data from the COVID-19 experience, such a trial might best be limited to early institution of therapy with plasma containing high titers of antibody in an attempt to maximize the anticipated treatment effect. Such an effort would, however, also require funding, a secure supply chain, and the availability of staff who are not directly engaged in providing medical care to the patients. If such a mechanism was in place for the current pandemic, it is possible that high-quality data would have been available to assess the likely benefits and risks of convalescent plasma therapy within less than 5–6 months of the rapid expansion of the disease into the community. Thus, by combining the national reach of the CTSA program and its remarkable depth of full spectrum translational expertise, the consortium’s unique synergy could be put to maximal use in improving the health of the nation and the world.
Discussion
The COVID-19 pandemic has rapidly emerged as one of the greatest translational research challenges in the last 100 years. It has changed nearly everything, from our ability to conduct in-person research visits to an unprecedented race for effective therapies and vaccines. In those areas of the country most severely affected by the virus, it has also required bravery, dedication, and courage on the part of countless medical professionals and other first responders as they put their own health at risk to save others, as well as the bravery of the research participants themselves. Despite the terrible toll that the pandemic has taken on both institutions and individuals, we believe that CTSA hubs have shown enormous creativity and perseverance to solve a myriad of new translational challenges, as well as team science on a scale that we could only imagine just a year ago. This response fits well the framework of Pandemic-Driven Post-traumatic Growth for Organizations and Individuals proposed by Olson et al. [Reference Olson, Shanafelt and Southwick22], defined as “positive psychological change experienced as a result of a struggle with highly challenging life circumstances,” providing an opportunity to view the pandemic not only as an unimaginable destructive force but also as a potential force for improvement. Among the key elements of the framework are, at the personal level, development of deeper relationships, openness to new possibilities, greater sense of personal strength, and greater appreciation of life. For success, it requires deliberative reflection, leading to action characterized by awareness, transparency, motivation, creativity, and dedication to improvement. Institutional parallels include transforming communication and delegation of authority and actively supporting caregivers.
Crisis management is often focused on restoring organizational function to its pre-crisis level, but perhaps a more appropriate goal is to achieve a higher level of function as a result of learning from the traumatic event. Reflective assessment, identification of extraordinary role models, identifying opportunities for reinvention of processes, contemplating how the experience connects the institution to the broader community and humanity, and reappraising priorities with regard to what is truly most important are some of the ways to achieve the goals of post-traumatic growth. There is no way to ignore the trauma we have all experienced individually and as members of great institutions. We hope that this theme issue detailing the activities of the CTSA program in response to the COVID-19 pandemic will help contribute to the goal before all of us, to make the trauma just the first chapter in the story of post-traumatic growth that will make all of our institutions and the CTSA program stronger, more resilient, and more effective.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cts.2021.10.
Acknowledgments
The authors thank all who participated in the CTSA survey on responses to the COVID-19 pandemic and offer special thanks to all who participated in, and led, the writing groups for the other papers in this special edition of The Journal of Clinical and Translational Science. Their commitment in the face of many competing demands under enormous time pressure reflects the high dedication of CTSA hubs and members to the goal of speeding effective therapies to improve human health. The authors also would like to thank Samantha Jonson, CTSA Program Steering Committee Executive Secretary, and the Center for Leading Innovation and Collaboration (CLIC) survey team (Scott McIntosh, Jackie Attia, Kathryn Buettner) and staff members (Rebecca Laird, Julie Schwan, Judy Giordano, Laura Hassinger, and Tracie Norman) for their rapid and excellent operational support. We want to thank Suzanne Rivera for outstanding administrative assistance.
This work was funded in part by the University of Rochester Center for Leading Innovation and Collaboration (CLIC), under Grant U24TR002260. CLIC is the coordinating center for the Clinical and Translational Science Awards (CTSA) Program, funded by the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH). This work is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors also acknowledge funding to their individual CTSA Hubs by NCATS: UL1TR002489 (JBB), UL1TR001866 (BC), UL1TR003096 (RK), UL1TR002345 (WGP), UL1TR002001 (MSZ).
Disclosures
The authors have no conflicts of interest to declare.






