Mucormycosis: a post covid-19 enigma
Varsha Agarwal, Ambika Gupta*, Virendra Singh, Neha Jajodia
MDS Student, Department of oral medicine and radiology, post graduate institute of dental sciences, India
2Senior Professor and Head, Department of oral medicine and radiology, post graduate institute of dental sciences, India
3Senior Professor and Head, Department of oral and maxillofacial surgery, post graduate institute of dental sciences, India
4Senior Resident, Department of oral and maxillofacial surgery, post graduate institute of dental sciences, India
Received Date: 29/05/2021; Published Date: 15/06/2021
*Corresponding author: Dr. Ambika Gupta, Senior professor and head, Department of oral medicine and radiology, post graduate institute of dental sciences, Rohtak, India. Email: drambika79@rediffmail.com
Abstract
Respiratory distress is commonly seen with COVID-19. But in many cases, the virus affects a person’s overall well-being and aggravates other systemic diseases. One such observation of grave concern is a rapid increase in the number of mucormycosis cases in patients recovering from COVID-19. This manuscript discusses a few hypotheses that may explain the pathogenesis of mucormycosis in post COVID-19 phase.
Keywords: COVID-19; Invasive fungal infections; Mucormycosis; Mucormycetes; Mycoses; SARS-CoV-2
Introduction
SARS-CoV-2, the causative agent of COVID-19 was first reported in Wuhan, China, in December 2019 and has spread across the globe to become a worldwide pandemic. Patients infected with COVID-19 are at increased risk of pulmonary embolism, acute cardiac injury, arrhythmias and secondary infections [1]. These systemic manifestations lead to long term hospitalization and use of multiple drugs. Probably, this is the major reason for increased recognition of secondary infections like Mucormycosis by the dentists in the post-COVID-19 phase [2].
Mucormycosis is a rare, opportunistic fungal infection observed primarily in immunocompromised individuals such as patients with diabetes, systemic use of corticosteroid, neutropenia, hematologic malignancies and stem cell transplant [1]. Recently, there has been a spike in the number of mucormycosis cases in post-COVID-19 infection cases.
Pathogenesis of Mucormycosis in Post Covid-19 Recovery Phase
A complex interaction of factors, including pre-existing diseases, medical therapy for management of COVID-19 induced complications, the risk of hospital-acquired infectionsand systemic immune alterations due to COVID-19 infection itself, may have been some of the predisposing factors for mucormycosis [2]. A few hypotheses may be proposed as under:
COVID-19 patients have immune dysregulation, with a decrease in number of T-lymphocytes i.e., CD4-Positive and CD8-Positive T-cells, thereby altering the innate immunity of an individual and enhancing the risk of invasive mycosis [2].
SARS-CoV and SARS-CoV-2 belong to the same species; have similar prevalence, clinical and biological characteristics. An increased incidence of fungal infection in SARS patients was noticed (14.8–27%), which was the major cause of death in those patients [3]. Similarly, an incidence of invasive fungal infections of 26.7% was reported by White et al in 135 screened adults with COVID-19 infection. Cases with invasive fungal diseases had an increased mortality (53% vs 31%) [2]. So, it may be hypothesised that due to similar biological behaviour as SARS-CoV, SARS-CoV-2 also predisposes to invasive fungal diseases.
The route of entry of SARS-CoV-2 is mediated through binding with angiotensin-converting enzyme 2 (ACE2) receptors. Nasal and oral mucosal epithelium have shown high expression of these receptors, that may have led to the increased affinity & attachment to these cells [4]. This may explain the symptoms of anosmia, ageusia, oral mucosal ulcerations and necrosis. Tissue necrosis of oro-nasal mucosa may promote mucormycetes, that is a normal commensal and saprophyte, to cause the invasive disease.
SARS-CoV-2 like other coronaviruses including SARS-CoV causes blocking or neutralisation of ACE2 receptors which increases the expression of pro-thrombotic CX3CL1, thus sparking off an increase in local inflammatory mediators, thromboembolic events and tissue necrosis. This in turn may predispose to fulminant fungal infections [5].
Countries like India have a high prevalence rate of type 2 diabetes mellitus (8.9% of adults), which is a well-known risk factor for the disease [2]. COVID-19 may also predispose infected individuals to hyperglycaemia and subsequent fulminant mycosis as described in Figure-1 & Figure-2 [6,7,8].
Corticosteroid therapy is associated with an increased risk of invasive fungal disease. Present guidelines in India recommend intravenous methylprednisolone 0.5-1 mg/kg/day for 3 days in moderate cases and 1-2 mg/kg/day in severe cases of COVID-19. The National Institute of Health recommends the use of dexamethasone (6 mg/day for a maximum of 10 days) in patients who are ventilated or require supplemental oxygen. These guidelines specifically mention the risk of developing a secondary infection [2].
Rawson et al reported the widespread use of broad-spectrum antibiotics, with as many as 72% of patients receiving these drugs, despite any evidence of infection [2]. Use of broad-spectrum antibiotics, may have led to an increase in the number of invasive mycosis super infections.
Luksamijarulkul P et al isolated fungal contaminants from the inside surface of used surgical masks mainly, Aspergillus spp. (37%) & Penicillium spp. (31%) [9]. This suggests that unhygienic practices like continued use of masks/ unwashed cloth masks may be another predisposing factor for fungal as well as bacterial infections.
Antinori S. et al. observed a high incidence of candidemia in patients treated with tocilizumab, which is used to manage cytokine storm in COVID-19 patients [10]. Despite much evidence in the literature, it may be considered as an additional precipitating factor in the pathogenesis of invasive fungal diseases.
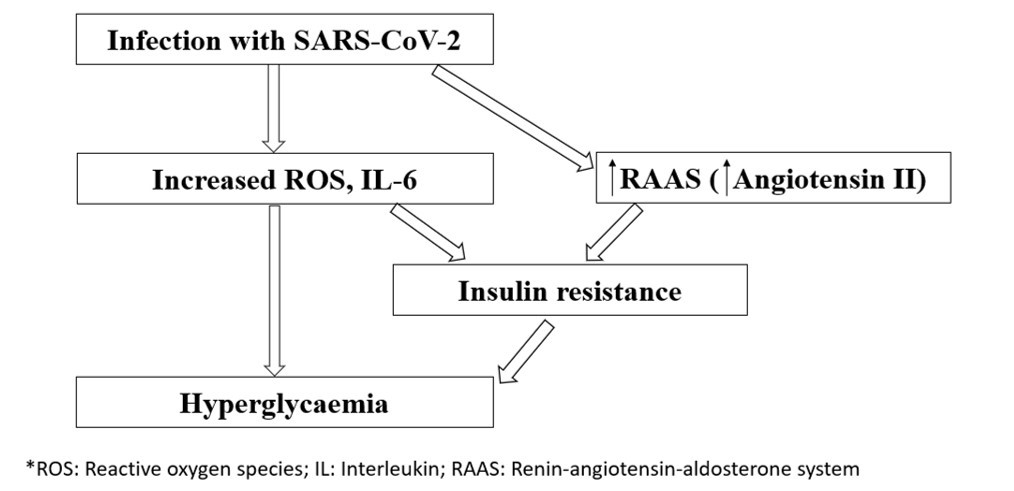
Figure-1: Flowchart showing hyperglycaemia induced by infection with SARS-CoV-2 (*ROS: Reactive oxygen species; IL-6: Interleukin-6; RAAS: Renin-angiotensin-aldosterone system)
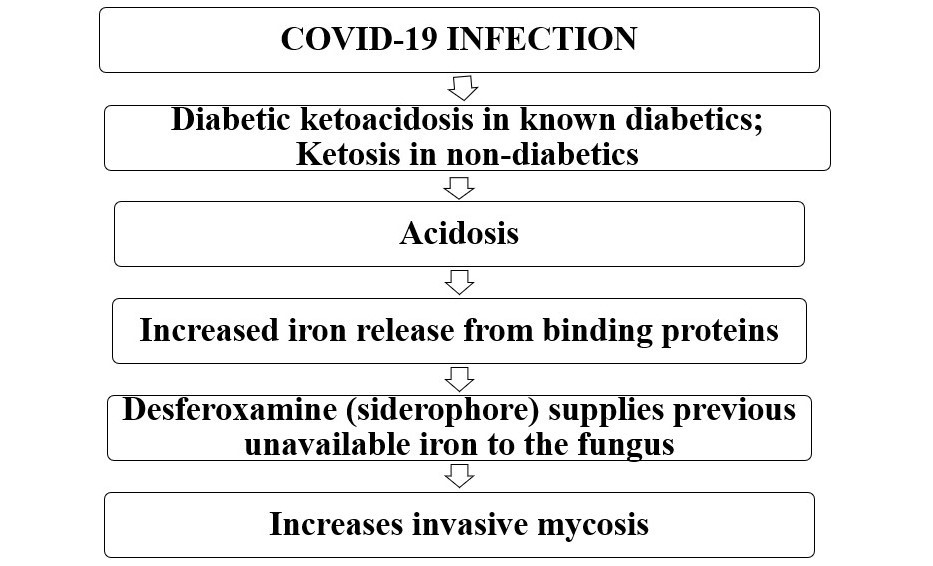
Figure-2: Pathogenesis of mucormycosis secondary to COVID-19 infection.
Conclusion
COVID-19 is significantly associated with an increased incidence of fungal secondary infections, probably due to its diabetogenic action, immune dysregulation and widespread use of steroids and broad-spectrum antibiotics. Hence, the dentists should be well aware of the possibility of secondary invasive mycosis post COVID-19 infection, for the early diagnosis and prompt treatment, in order to reduce the associated morbidity and mortality.
Statements and declarations
Author Contributions: All authors contributed to accomplishment of this manuscript. Dr Varsha Agarwal searched the literature, analysed and interpreted the collected data and drafted the article. Dr Ambika Gupta conceptualised and designed the article, analysed and interpreted the collected data and contributed for the critical revision. Dr Virendra Singh conceptualised and designed the manuscript and was responsible for the critical revision. Dr Neha Jajodia searched the literature and helped in the data collection. The manuscript has been approved by all the authors.
Funding: The author(s) received no specific funding for this work.
Compliance with Ethical Standards/ Conflict of interest: The authors declare that they have no conflict of interest pertaining to this work.
Ethical Approval: Not applicable.
References
- Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. The American Journal of Emergency Medicine. 2020.
- Mehta S, Pandey A. Rhino-Orbital Mucormycosis Associated With COVID-19. Cureus. 2020.
- Song G, Liang G, Liu W. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia. 2020. p. 1-8.
- Salamanna F, Maglio M, Landini MP, Fini M. Body Localization of ACE-2: On the Trail of the Keyhole of SARS-CoV-2. Frontiers in medicine. 2020; 7: 935.
- Rivas-Fuentes S, Valdés VJ, Espinosa B, Gorocica-Rosete P, Salgado-Aguayo A. Could SARS-CoV-2 blocking of ACE2 in endothelial cells result in upregulation of CX3CL1, promoting thrombosis in COVID-19 patients? Medical Hypotheses. 2021; 151: 110570.
- Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nature Reviews Endocrinology. 2020. p.1-20.
- Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID‐19 infection may cause ketosis and ketoacidosis. Diabetes, Obesity and Metabolism. 2020.
- Rapidis AD. Orbitomaxillary mucormycosis (zygomycosis) and the surgical approach to treatment: perspectives from a maxillofacial surgeon. Clinical Microbiology and Infection. 2009; 15: 98-102.
- Luksamijarulkul P, Aiempradit N, Vatanasomboon P. Microbial contamination on used surgical masks among hospital personnel and microbial air quality in their working wards: A hospital in Bangkok. Oman Medical Journal. 2014; 29(5): 346.
- Antinori S, Bonazzetti C, Gubertini G, Capetti A, Pagani C, Morena V et al. Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia: an increased risk for candidemia? Autoimmunity reviews. 2020;19(7):102564.

