Abstract
Objectives
The disproportionate impact of coronavirus (COVID-19) on African Americans along with associated inequities in social determinants of health (SDOH) and racism increase their vulnerability to the psychosocial impact of COVID-19. This qualitative study applied the socio-ecological model (SEM) to explore psychosocial stressors, coping styles, and needs to improve psychosocial health among unique subgroups of African Americans in early pandemic stages.
Methods
Sixty-two African Americans (16 parents, 15 young adults, 16 essential workers, and 15 individuals with underlying medical conditions) participated in qualitative, semi-structured interviews between May and September 2020. Interview data were analyzed based on the SEM using thematic analysis.
Results
The majority (84%) reported being stressed with parents having the highest level. Four themes emerged : (1) our COVID-19 pandemic state of mind, (2) top stressors in the early stages of the COVID-19 pandemic, (3) coping strategies during COVID-19, and (4) needs during the COVID-19 pandemic to reduce stress. While there were similarities, different stressors were experienced among subgroups, which yielded different coping styles and needs from stakeholders across multi-levels to improve their psychosocial health.
Conclusions
Findings suggest current and future pandemic response plans need targeted strategies across multiple levels of influence to address the psychosocial impact of the COVID-19 pandemic on African Americans.
Similar content being viewed by others
Introduction
As of December 2021, COVID-19 cases were the highest in the USA, having over 50.3 million confirmed cases, including over 800,000 deaths [9]. The rapid spread of COVID-19 has negatively impacted the mental health of Americans. According to the Kaiser Family Foundation (KFF) Health Tracking Poll, approximately 53% of Americans reported experiencing worry and stress from the pandemic in July 2020 and 47% in March 2021. Women, parents, young adults, essential workers, and individuals with underlying medical conditions bear the greatest mental health impacts [26]. Early in the pandemic, the mental health status largely reflected the significant disruption in economics, healthcare systems, childcare, food systems, and social exchange [43]. Furthermore, the transmission dynamics of SARS-CoV-2 and the disparate COVID-19 outcomes in morbidity and mortality further sparked impromptu stay-at-home orders by the governments and the implementation of preventive mandates (e.g., face masks and social distancing) [31, 56]. Everchanging updates, lack of information, and even the circulation of mis- and/or disinformation continues to impact the mental health of Americans [39, 43]. Increasing evidence has shown long-term biological consequences of stress [29, 47]. Therefore, how one copes is significantly related to how these psychological stressors are handled in the COVID-19 pandemic and ultimately influences health outcomes [50].
Many racial and ethnic minorities experience inequities in social determinants of health (SDOH) (e.g., lack of or limited access to quality care, crowded housing, jobs as essential workers or job loss, and experience discrimination) often caused by structural racism. These inequities in SDOHs place them at greater risk for psychosocial distress and have negatively impacted their ability to cope [3, 37, 45]. The COVID-19 pandemic highlighted these many inequities, fueling this global public health crisis [27]. Unsurprisingly, African Americans have and continue to be disproportionately impacted by COVID-19. While comprising only 13% of the US population, COVID-19 hospitalizations and death rates among African Americans are almost three and two times higher compared to Whites [9]. Due to the link between economic and physical health [18], disproportionate COVID-19 outcomes partially reflect African Americans (57%) being more likely to worry about themselves or their families getting COVID-19 compared to Whites (43%) [26]. Furthermore, compared to Whites, African Americans are about 1.7 times more likely to say they had trouble covering usual household expenses, 2.5 times more likely to report not having enough to eat, and 3 times more likely to self-report not being caught up on rent [11]. They are also more likely to be threatened by reductions in pay or hours, temporary furloughs, or permanent layoffs [35]. Collectively, this syndemic—COVID-19 pandemic, racism, and “structural inequity”—contributes to psychosocial distress in marginalized communities and has prompted the opportunity for a transformational change [52].
Pandemic response plans often lack or have a limited response in the area of psychosocial stress [1]. For example, during the SARS epidemic of 2002–2003, there lacked little expert guidance on how to address these demands [6]. Similarly, the world’s leading experts have placed the majority of their attention on managing COVID-19 and associated complications, preventive behaviors, and vaccine and treatment developments. In addition, individuals lack access to mental health services especially those already facing psychosocial distress prior to the pandemic. This warrants great concern as (1) past research has highlighted the long-lasting cognitive and mental health effects of a pandemic on a population [55]; and (2) we are experiencing a syndemic. Recently, there has been a shift to focus on the psychosocial impact of the pandemic on the public. So, there is a need to identify the root cause and strategies to mitigate the psychosocial stress among African American communities during and post-COVID-19 pandemic.
The purpose of this qualitative study was to explore the mental health status and stressors of uniquely vulnerable subgroups of African Americans during the initial stages of the COVID-19 pandemic through the framework of the Socio-Ecological Model. We further explored the coping strategies and perceived needs from stakeholders across multilevels to reduce the psychosocial stress of African Americans bearing the greatest mental health impact.
Methods
Socio-Ecological Model (SEM) and COVID-19
According to the SEM, there are five levels of influence on health behavior, which are interactive and reinforcing [34, 46, 54]. The intrapersonal level includes the knowledge, attitudes, and motivations of an individual around COVID-19 that affect mental health. Interpersonal level refers to the influence received from family, friends, and peers during the COVID-19 pandemic. The organizational level involves the practices and policies of the organizations around COVID-19. The community refers to the collaboration of organizations to create change during COVID-19. Last, the societal level refers to local, state, and national laws that are developed and/or activated to influence change. For this study, we explore how factors on each of these levels influence mental well-being and strategies perceived by uniquely vulnerable African American subgroups to improve or mitigate the psychosocial impact of the COVID-19 pandemic.
Study Design, Sample, and Recruitment
Semi-structured interviews were conducted between May and September 2020 amid the COVID-19 pandemic. A phenomenological approach was chosen to explore the mental status of vulnerable African American subgroups and gain an in-depth understanding of coping strategies and needs from multilevel stakeholders to help improve their mental health. Interviews via Zoom, an online teleconferencing software program, were chosen due to the nature of the pandemic (e.g., need to physically distance). In addition, they have several advantages including improved access to interviewees, reduced costs, and increased convenience for interviewees [16, 36, 57].
To recruit participants, a purposive sampling method was used [42]. Inclusion criteria were aged 18 and older and a member of one of the following categories—essential worker (i.e., “one who conducts a range of operations and services in industries that are essential to ensure the continuity of critical functions in the United States” [10]), parent, young adult aged 18 to 35 years, or individual with an underlying medical condition. We chose these categories to gain diverse perspectives on the impact of COVID-19 on mental health among subgroups bearing the greatest health impact. We used our existing database, community partners, and flyers as recruitment mechanisms. We assigned participants upon recruitment to the subgroups and informed participants they would address questions from this perspective.
Measures
Socio-demographics were collected to provide a description of the sample only. Stress was measured as a categorical variable (yes/no). This was confirmed in qualitative responses identifying participant stressors during the early pandemic stages. Age was a continuous variable measured in years. Participants self-identified as African American and indicated membership in the following categories: essential worker, UMC, young adult, or parent. Education categories were some high school, GED or high school diploma, associate’s degree, some college, bachelor’s degree, master’s degree, and doctoral/professional degree. Categories were collapsed to create a dichotomous variable (some college or less and associate’s degree or higher). Income categories were less than $20,000, $20,001–$40,000, $40,001–$60,000, $60,001–$80,000, over $80,000, and prefer not to answer. Categories were combined to form less than $40,000, $40,001–$80,000, over $80,000, and do not want to answer.
Data Collection Procedures
Three medical students and two researchers conducted interviews. The research team had extensive experience in qualitative research and provided training to the medical students prior to study initiation. Interested individuals received a survey link to a REDCAP survey (i.e., a secure online platform for organizing and storing surveys and data) to screen for study eligibility [22]. During the interview, participants were read a study information sheet and informed consent documentation. After providing verbal consent, interviewers used the protocol based on the SEM to elicit views toward the impact of COVID-19 on African Americans’ mental health. The SEM was also used to guide the discussion related to stressors (i.e., coping strategies and needs from multilevel stakeholders) to help address psychosocial stressors associated with the syndemic from the perspective of their assigned subgroup. Interviews lasted 45–90 min and were audio-recorded. One team member conducted the interviews, while another team member took notes.
Data Analysis
Prior to analysis, all interviews were transcribed via Zoom. Members of the research team reviewed each transcript for accuracy. SPSS (version 26) was used to conduct a descriptive analysis (i.e., frequencies, percentages, cross-tabulations, and ANOVA) for socio-demographics among those who stated they were stressed compared to those who stated they were not stressed. To guide the coding process, a hierarchical coding system was developed using the questions and preliminary review of five transcripts per group. To establish reliability in the coding system, each researcher independently coded five transcripts, compared the codes, and added or removed codes. Then, the coding of the remaining transcripts was completed by the two researchers. When no new codes emerged, saturation was met. Codes were then placed into categories based on the overall group, the subgroups, and then by constructs of the SEM, a process known as axial coding [20]. We then conducted thematic analyses, a qualitative approach, which involved (1) a constant comparison of codes to explore patterns in responses; and (2) identification of themes within and across subgroups by the degree of stress. Verification procedures were intercoder reliability, investigator triangulation, and thick, rich descriptions [30].
Results
Interviews were conducted with 62 African Americans belonging to uniquely vulnerable populations to gain diverse viewpoints on the mental health impact of the COVID-19 pandemic: 16 parents, 16 essential workers, 15 individuals with underlying medical conditions (UMCs) (e.g., autoimmune disorders, sickle cell disease, diabetes), and 15 young adults (ages 18–35). In the overall sample, the majority were female (n = 43; 69.4%) with a mean age of 40.29 years. For essential workers, the majority were female (n = 10; 62.5%) with a mean age of 38.81 years. Individuals with underlying medical conditions were primarily female (n = 12; 80%) with a mean age of 55.47 years. Young adults were primarily female (n = 10; 66.7%) with a mean age of 27.60 years. For parents, the majority were female (n = 11; 68.8%) with a mean age of 39.44 years. Approximately 84% stated they were stressed during early pandemic stages. See Table 1 for socio-demographics by subgroup. There were no significant differences in socio-demographics within each subgroup (results not shown). We also explored stress levels by socio-demographics (see Table 2). Gender by stress was marginally significant (p = 0.055) with females having higher levels of stress.
Four major themes emerged in this study: (1) our COVID-19 pandemic state of mind, (2) top stressors in early stages of COVID-19 pandemic, (3) coping strategies during COVID-19, and (4) needs during the COVID-19 pandemic to reduce stress. See brief descriptions below and Table 3 for sample quotes.
Theme 1: Our COVID-19 Pandemic State of Mind
Most participants across subgroups expressed they were experiencing heightened stress, anxiety, and/or depression due to the COVID-19 pandemic. Many feared getting infected with SARS-CoV-2 along with potential sequelae and outcomes such as hospitalization and even death. Some further described how their relationships (e.g., marriages, parent-child, extended family, friendships) were feeling less connected or too connected due to physical distancing, living in multi-generational homes, and lack of distancing in their work environment. Some further stated how they felt “vulnerable” due to the politically motivated government not providing equitable resource allocation along with poor access to physical and mental healthcare services or COVID testing. Hence, they feared an emerging syndemic, the interaction of a “racial pandemic,” public health pandemic, and health inequities. This syndemic was perceived to magnify the existing mental health issues within the African American community that are exacerbated due to structural racism. Therefore, many anticipated a lasting effect of this pandemic on mental health throughout the entire population.
Within the subgroups, many parents stated how their children had limited understanding of the COVID-19 pandemic and were not prepared socially and emotionally for the changes (e.g., virtual or lack of learning, physical distancing, face-mask wearing). Many with UMCs discussed withdrawal, being a “zombie,” or feeling as if “walls were closing in” since they had to isolate themselves. Specifically, they mentioned the toll of relying on others to perform tasks (e.g., grocery shopping) and not being able to help loved ones who contracted the virus. Some also expressed feelings of uselessness and depression. Essential workers often described their high COVID-risk jobs, the varying labor protections, and the need to engage in preventive behaviors to protect themselves and those in their home environment. Despite this, many participants attempted to maintain a positive outlook, and some stated they were adapting to the current state of the pandemic.
Few individuals in each subgroup expressed that their mental state had been unaffected by the pandemic. One young adult shared that the pandemic was just the next chaotic thing to happen in the USA, so she was not stressing about it. A few individuals with UMCs shared this was not anything new to them since they were already living life as a “sick person,” and incorporating preventative behaviors (i.e., social distancing, wearing masks) did not add extra stress. Last, a few parents indicated the social distancing mandates and stay-at-home orders allowed them to spend more time with family.
Theme 2: Top Stressors in Early Stages of the COVID-19 Pandemic
We describe the stressors using the SEM at the intrapersonal, interpersonal, community/organizational, and societal levels and highlight similarities and emerging differences by subgroup within those levels.
Intrapersonal
One major effect of this global pandemic was the loss of jobs/income and subsequent financial instability described within all subgroups. Along with the loss of income came the loss of health insurance coverage, preventing people from obtaining essential healthcare. While the government provided stimulus checks, many young adults and parents shared sentiments that the amount was insufficient and the overall economic plan was not equitable. Young adults were already living “paycheck to paycheck,” and some lost their jobs during the pandemic. A few were claimed as dependents on their parents’ income taxes and could not receive the funds. Participants with UMCs and even some essential workers mentioned the difficulty of obtaining necessities, accessing healthcare, and adhering to public safety measures, particularly their avoidance of large crowds. Gaining weight due to being more sedentary, closed gyms, and less healthy eating was also identified as a stressor. Participants also reflected on the fear and anxiety of exposure to the virus especially due to their current health conditions and financial situations. Furthermore, a small number of participants mentioned the stigma of a COVID diagnosis adding another layer of anxiety and even hesitancy when deciding to get tested. A few participants also shared that being Black and a male heightened the trauma that might be experienced from situations like the pandemic. Particularly, the anxiety of all mothers of Black males and young adult men heightened in light of racial violence and the need to engage in face mask wearing during the COVID-19 pandemic. Last, many essential workers stressed about the possibility of losing their job or getting COVID-19 especially due to lack of personal protective equipment (PPE) based on the political stance on masks.
Interpersonal
Many participants expressed the need for emotional support from family and friends, yet many lacked this physical connection and intimacy. Particularly, young adults feared visiting family due to their inability or refusal to physical distance. Most individuals with UMCs preferred to physically distance themselves to protect their health. In contrast, some participants especially essential workers feared exposing loved ones to SARS-CoV-2. In both instances, a few individuals lived in multigenerational homes, which exacerbated these fears. Parents also shared the distress of trying to balance working from home while simultaneously caring for children, facilitating playtime, and maintaining virtual schooling. Another layer of stress was the parent’s inability to teach the lessons provided by their children’s schools due to their own educational background. A minute number of parents mentioned the emotional burden of explaining the pandemic to their children. Lastly, some individuals were exhausted from hearing about or not talking enough about COVID-19 with their family, friends, and peers.
Community/Organizational
Across all subgroups, participants shared that the lack of communication and cohesiveness from local government and institutions contributed to their mental distress. The amount of uncertainty surrounding the pandemic origins, contradicting information on preventive behaviors, and poor adherence to public safety protocols among employees and public places contributed to their stress. Multiple parents shared that the lack of communication from their children’s schools along with the lack of attention to the inequities in access to remote learning and resources was a stressor for many in marginalized communities. Many essential workers and individuals with UMCs shared their frustration with people not being considerate of others and not following prevention mandates. While a few essential workers mentioned their employers were prepared in terms of providing PPE and ensuring labor protection laws were enforced, others shared that theirs were not concerned and/or lacked access to PPE for their employees. Multiple essential workers mentioned being overworked and undercompensated or lacked leave due to a COVID-19 diagnosis further exacerbating stress levels. Last, many participants also perceived the health system was not prepared for a pandemic (e.g., lack of medicines to treat COVID-19, telemedicine to increase access, or pandemic response plans) to engage with the community, which stressed them further.
Societal
Across all subgroups, the uncertainty and the fear surrounding the COVID-19 perpetuated by the media was a top stressor. Participants highlighted the barrage of information that came from many different sources, including the national government, and how the information did not align or was untimely. This heightened anxiety in being unaware of how to protect themselves and their loved ones. Many participants also shared that the current sociopolitical landscape, racial violence, and discrimination against the Black community exacerbated the stress of the pandemic itself. A young adult participant shared the COVID-19 pandemic revealed how the government was not working for the people through structural racialization. Most participants discussed the lack of or poor measures to ensure access to healthcare or mental healthcare along with poor issuance or demanding compliance of policies for workplace safety. A few parents highlighted the inequitable distribution of school funding, emphasizing the digital divide and the negative impact on their child’s education. Last, participants highlighted the inequities in the COVID-19 response and resources, which further complicated the lived Black experience.
Theme 3: Coping Strategies During COVID-19
Participants were asked about strategies used to cope with their stressors. The answers were grouped into six categories: (1) meaning-making, (2) health promotion, (3) cognitive, (4) interests, (5) structure/organization, and (6) maladaptive coping strategies.
Multiple participants coped by reframing their stress as opportunities for growth and development (i.e., meaning-making). Some perceived this pandemic as a sign from God to slow down and focus on aspects of their lives that were previously neglected while others mentioned this experience strengthened their spiritual connection. This was common among many essential workers and individuals with UMCs.
Many mentioned the shutdown allowed time to cook healthier meals or be more mindful about their diet. Others shared that the increased time spent at home caused them to adopt a more sedentary lifestyle. Therefore, they increased engagement in healthier behaviors—exercise, meditation, and yoga—all serving as “stress relievers.” The individuals with UMCs set boundaries and guidelines for interacting with family and peers (e.g., Zoom meetings). Participants also utilized cognitive coping strategies (e.g., positive thinking, limited interaction with media or social media platforms, and even formal therapy) to deal with their stressors. However, a few parents stated they connected with other parents to discuss strategies to engage children during the COVID-19 pandemic.
Many participants developed new hobbies and interests such as reading, journaling, music, and gardening as a means of coping. Multiple individuals also shared that they were coping with and managing their stress by looking to provide more structure and organization, which includes some parents getting assistance from family, to establish routines and a sense of normalcy in their home/family life.
Although most participants shared somewhat healthy coping strategies, a handful of individuals reported the use of maladaptive methods. A few participants, particularly essential workers and young adults, stated their increased drug and alcohol use during the COVID-19 pandemic. Others highlighted the loss of sleep. With the increased time spent at home, often alone, many people especially those with UMCs shared that they were often overindulging in unhealthy food habits or eating more takeout/fast food. This led to increased weight gain and more stress. A few young adults also highlighted online shopping and hanging with friends as coping strategies.
Theme 4: Needs During the COVID-19 Pandemic to Reduce Stress
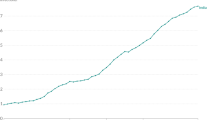
Participants described their needs to reduce stress during the COVID-19 pandemic, which aligned with the SEM. We described each of their needs by level and subgroups (see Fig. 1 for a summary).
Intrapersonal
Multiple participants in each group mentioned they either did not need anything or they did not know how to define what they needed. To manage emotional stressors, many participants also stated they did not feel the burden should be on anybody to support them, and that their happiness was solely their responsibility. Many participants who were essential workers and individuals with UMCs stated they needed to lean deeper into their spirituality. A few participants especially young adults and parents indicated a need to identify multiple income strategies to reduce financial stressors.
Interpersonal
Many of the participants’ needs fell into the interpersonal category, where people were emotionally drawn to the need for physical contact with others and support with tasks around the house. A few participants, particularly young adults and parents, mentioned the need for consistent check-ins, phone or in-person, from their friends and family. Last, participants, especially those with UMCs, wanted their friends to take COVID more seriously and support them in engaging in preventive practices consistently.
Community/Organizational
Across groups, participants needed better effort from businesses, schools, and community institutions to “keep things sanitized and just try to be as safe as possible” as it relates to COVID-19. Improved and cohesive communication from local government and community institutions was identified as a need. Participants also shared they definitely need “the health care providers and to have the researchers to present the factual data about this thing.” Last, many participants across subgroups, especially essential workers, wanted their employers to enforce labor protections, provide PPE, and protect their benefits if affected by COVID-19.
Societal
A few participants in each group mentioned the need for the pandemic response to be depoliticized so that the focus could actually be on helping the people. All participants emphasized the need for improved communication on the pandemic from the national and state government. Many participants in each group shared needs related to improved policies and financial support across several initiatives, which they perceived should have occurred before the pandemic. They mentioned the need for better financial support outside of the stimulus and improved unemployment benefits to ensure their families and themselves could “survive” the pandemic. Improved healthcare policies were requested to accommodate those without healthcare access and those who lost jobs due to the pandemic. Essential workers identified the need for improved or enforced labor protections at their jobs (e.g., provision of PPE, better job benefits) and allocated funding for PPE. Multiple parents mentioned the need for better federal policies and financial support for their local schools to improve sanitation procedures and lower the digital divide that is commonly faced among communities of color.
Discussion
In the USA, the COVID-19 pandemic has had a profound, yet the disproportionate impact on African Americans, especially uniquely vulnerable subgroups. Particularly, the emerging syndemic of COVID-19, health inequities, and racism has yielded poor outcomes in health, economics, and social wellness, which has exacerbated poor mental health among African Americans [51]. We found that almost all participants were experiencing stress on some level with women having higher stress levels, reflecting studies emerging in the literature [17, 33, 52, 59]. Because women naturally experience more stress and anxiety compared to men, the COVID-19 pandemic may be exacerbating this difference [12, 21]. Surprisingly, when we viewed stress levels by each subgroup, we found that there were no significant differences. These findings suggest that each subgroup has stressors that could be similar within or unique to each subgroup.
To our knowledge, this study is the first to apply the SEM to explore differences in COVID-19 stressors and needs among subgroups within the African American population. Our qualitative findings demonstrated similar and different stressors across multilevels, which impact their psychological health. Participants experienced varying degrees of loneliness and uncertainty regarding COVID-19. This was exacerbated by untimely communication, misinformation, and lack of resources (e.g., lack of access to healthcare and COVID-testing, mental healthcare, and PPE) from local and federal government along with community institutions and organizations were unsurprising. As identified in prior studies [28, 48], participants carried the weight of the sociopolitical climate, Black Lives Matter movement, and political exploitation, which underscored the structural inequities in the midst of a global pandemic. Poor pandemic responses and social injustice have been a long-standing issue especially for communities of color [14, 58]. For mental health, racial and ethnic disparities have commonly existed with few available resources, and COVID-19 has exacerbated this issue as identified in our study [19, 32]. Collectively, these findings support the need for equitable public health policies, which are inclusive of mental health services to address the psychological impact of pandemics ([38] and 4).
The unfair distribution of financial resources yielded unique stressors among our groups (i.e., parents concerned about the inequitable distribution of digital technology and trained teachers among schools; essential workers lacked or had poor compliance of safety policies and benefits; individuals with UMCs working without mask mandates and access to care, and young adults lacked access to stimulus packages or lost jobs). COVID-19 exposed the structural effects of racism through the digital divide experienced in K-12 education [49, 24), demonstrated by the increased level of stress associated with homeschooling and the increased economic spending among parents in our study. Studies suggest that individuals experiencing an increased care burden during the COVID-19 pandemic suffer from the highest levels of psychosocial distress [7]. Women, particularly, bear the brunt as they are more apt to work part-time or be unemployed in order to homeschool their children. Furthermore, there is a spillover effect on their children (Russell 2020 and others). Nearly 30% of essential workers perceive their mental health has worsened, and more than half rely on unhealthy behaviors to navigate the pandemic [4]. Our findings shed light on the lack of or poor enforcement of policies, which play a role in the current mental state of essential workers. More policy support from society and community/organization could be instrumental in combatting these COVID-19 stressors. In addition, young adults highlighted their financial anxiety in our study, which is found in other studies and may in part reflect increased unemployment and food security [8, 41]. Last, individuals with UMC’s are particularly vulnerable to COVID-19 and mental distress due to structural racism (e.g., racial bias in the healthcare system), and their health conditions increase their fear and anxiety as demonstrated in our findings [13]. Together, these further confirm that targeted approaches, including support from public policy, are necessary to address the mental health stressors within the African American population during the COVID-19 pandemic.
Many of the coping strategies within the Black community, such as familialism and spirituality, were hampered due to the safety measures and restrictions due to COVID-19 [25, 53]. A few participants in our study did revert to their prayer life and scriptures to cope as cited in past studies [25]. However, studies have found that the closure of churches may disproportionately impact the coping of the African American community during the pandemic [15]. Our findings identified exploration of new hobbies, the establishment of structure in the home, limitation of media exposure, meditation, and engagement in health promotion as key coping mechanisms among African Americans [5]. It was unsurprising that maladaptive coping strategies such as drug and alcohol use emerged. This could reflect the existing opioid crisis in the African American community in addition to fewer resources or strategies available to reduce psychosocial stress [2, 23].
Future Directions
When exploring needs from additional stakeholders, unsurprisingly, the needs differed across multilevels by groups. We merge the existing literature with our findings to provide the following targets to reduce psychosocial stressors among each subgroup for the current and future pandemics:
-
All participants: needs: (1) accurate, ongoing communication on the COVID-19 pandemic; (2) access to healthcare and mental healthcare; (3) coping strategies to address loneliness and grief; and (4) improved financial assistance. Targets: (1) identify and implement pandemic information using preferred sources and channels; (2) restructure the healthcare system and mental healthcare treatment system to increase access (e.g., training of staff; establishing a system to identify and treat mental health issues); (3) educate on coping strategies (e.g., open communication between family and peers); and (4) improve policies around unemployment.
-
Essential workers: needs: (1) provision of PPE; (2) improved and enforced labor protection laws; (3) determine best preventive behaviors against COVID-19; and (4) financial assistance. Targets: (1) policies to ensure all have access to PPE; (2) improve benefits package (e.g., paid sick leave, flexibility); (3) educate on best preventive behaviors; and (4) create and/or enforce work safety policies including monitoring of mental health related to COVID-19.
-
Young adults: needs: (1) financial assistance; and (2) social interaction. Targets: improve federal government financial assistance policy; and (2) educate on COVID risks and how to safely gather socially.
-
Parents: needs: (1) training on the use of technology; (2) access to technology; and (3) address parental burnout. Targets: (1) offer training on digital technology to parent, child(ren), and teachers; (2) educate on self-coping strategies for parents and children; (3) jobs that offer childcare benefits; (4) improved communication plans from schools; and (5) policies that offer financial solutions (e.g., vouchers for WiFi hotspots) to costs associated with technology and ensures equal access (e.g., ability to lay cables for access).
-
Individuals with underlying medical conditions: needs: (1) continued access to care; (2) improved communication from providers. Targets: (1) revision of healthcare infrastructure (e.g., identify strategies to prevent disruption of healthcare); (2) education for providers on how to engage and communicate with patients during pandemics.
Strengths and Limitations
This is one of the first studies to capture psychosocial stressors, coping strategies, and needs from other stakeholders to address stressors among different subgroups of African Americans. This work can inform response plans that address the psychosocial impact of the COVID-19 pandemic and future pandemics. However, these views cannot be generalized to the African American community as a whole and other groups within the population. Hence, a quantitative study is necessary to predict whether factors influencing stress and coping strategies differ across subgroups. This study was conducted in the beginning of the pandemic, and stressors and needs may have changed over time. For example, we did not find the rise in interpersonal and domestic violence reflected in our narratives [40, 44]. Researchers’ personal biases could influence data collection procedures and interpretation; however, there were several checkpoints to reduce these including investigator triangulation and establishment of researcher biases. Last, we are aware that intersectionality is at play in our findings; however, that was not the scope of this work and should be explored in future studies.
Conclusions
Insights from this study suggest the need for comprehensive yet equitable public health programs inclusive of mental health to improve the psychological health of uniquely vulnerable subgroups of African Americans during and post-pandemic. Clinicians and researchers can use these insights to better understand targeted strategies that African American communities use to cope with stressors and how best to prepare and support them in the current and future pandemics. Furthermore, policy makers, and even community institutions and organizations now have an opportunity to address many systemic issues, which contribute to mental health inequities.
Data Availability
Due to the confidentiality agreements, supporting data cannot be made openly available.
References
(WHO) World Health Organization. “Pandemic influenza risk management: a WHO guide to inform and harmonize national and international pandemic preparedness and response.” 2017. Accessed on September 28, 2021 from https://apps.who.int/iris/handle/10665/259893.
Abramson A. Substance use during the pandemic. Monit Psychol. 2021;52(2):22 http://www.apa.org/monitor/2021/03/substance-use-pandemic.
APA. (American Psychological Association). “Stress and health disparities: contexts, mechanisms, and interventions among racial/ethnic minority, and low-socioeconomic status populations.” APA Working Group on Stress and Health Disparities. 2017. Accessed on September 24, 2021 from https://www.apa.org/pi/health-disparities/resources/stress-report.
APA. (American Psychological Association). “Essential workers more likely to be diagnosed with a mental health disorder during pandemic.” 2021. Accessed on September 28, 2021 from http://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress-essential
Bhattacharjee B, Acharya T. The COVID-19 pandemic and its effect on mental health in usa - a review with some coping strategies. Psychiatric Q. 2020;91(4):1135–45. https://doi.org/10.1007/s11126-020-09836-0.
Brewin CR, DePierro J, Pirard P, Vazquez C, Williams R. Why we need to integrate mental health into pandemic planning. Perspect Public Health. 2020;140(6):309–10. https://doi.org/10.1177/1757913920957365.
Budnick A, Hering C, Eggert S, Teubner C, Suhr R, Kuhlmey A, Gellert P. Informal caregivers during the COVID-19 pandemic perceive additional burden: findings from an ad-hoc survey in Germany. BMC Health Serv Res. 2021;21(1):353. https://doi.org/10.1186/s12913-021-06359-7.
Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934.
CDC (Centers for Disease Control and Prevention). “The COVID Racial Data Tracker.”2021a. Accessed on December 12, 2021 from https://covidtracking.com/race.
CDC (Centers for Disease Control and Prevention). “Risk for COVID-19 infection, hospitalization, and death by race/ethnicity | CDC, 2021b.” Accessed on December 11, 2021 from https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html.
Center on Budget and Policy Priorities. “Tracking the COVID-19 recession’s effects on food, housing, and employment hardships.”2021. Accessed on September 29, 2021 from https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and.
Chaplin TM, Hong K, Bergquist K, Sinha R. Gender differences in response to emotional stress: an assessment across subjective, behavioral, and physiological domains and relations to alcohol craving. Alcohol Clin Exp Res. 2008;32(7):1242–50. https://doi.org/10.1111/j.1530-0277.2008.00679.x.
Cobb RJ, et al. Perceived COVID-19 health threat increases psychological distress among Black Americans. Ethn Racial Stud. 2021. https://doi.org/10.1080/01419870.2021.1867216.
DeBruin D, Liaschenko J, Marshall MF. Social justice in pandemic preparedness. Am J Public Health. 2012;102(4):586–91. https://doi.org/10.2105/AJPH.2011.300483.
DeSouza F, Parker CB, Spearman-McCarthy EV, Duncan GN, Black RMM. Coping with racism: a perspective of COVID-19 shurch closures on the mental health of African Americans. J Racial Ethn Health Disparities. 2021;8(1):7–11. https://doi.org/10.1007/s40615-020-00887-4.
Drabble L, Trocki KF, Salcedo B, Walker PC, Korcha RA. Conducting qualitative interviews by telephone: lessons learned from a study of alcohol use among sexual minority and heterosexual women. Qual Soc Work : Res Pract. 2016;15(1):118–33. https://doi.org/10.1177/1473325015585613.
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686.
Florant A, Noel N, Stewart S, and Wright J. “COVID-19: investing in Black lives and livelihoods.” 2020. Accessed on September 12, 2021 from https://dataspace.princeton.edu/handle/88435/dsp01xg94hs51q.
Garrusi B, Amirkafi A, Garousi S. Mental health: the forgotten aspect of the COVID-19 pandemic. East Mediterr Health J. 2020;26(10):1151–4. https://doi.org/10.26719/emhj.20.117.
Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. 2012;39(3):364–72. https://doi.org/10.1177/1090198111418634.
Hamel L and Salganicoff A. 2020. “Is there a widening gender gap in coronavirus stress?”. Accessed on September 14, 2021 from https://www.kff.org/policy-watch/is-there-widening-gender-gap-in-coronavirus-stress/.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
James K, Jordan A. The opioid crisis in Black communities. J Law Med Ethics. 2018;46(2):404–21. https://doi.org/10.1177/1073110518782949.
Jones JM. The dual pandeics of COVID-19 and systemic racism: navigating our path forward. Sch Psychol Forum. 2021;36(5):427–31. https://doi.org/10.1037/spq0000472.
June LN, June SA. Initial real time coping by African American Christians during the coronavirus pandemic (COVID-19). J Pastoral Care Counsel. 2021;75(3):179–87. https://doi.org/10.1177/15423050211027523.
Kearny A, Hamel L, and Brodie M. 2021. “Mental health impact of the COVID-19 pandemic: an update.” https://www.kff.org/coronavirus-covid-19/poll-finding/mental-health-impact-of-the-covid-19-pandemic/.
Kickbusch I, Leung GM, and Bhuuta ZA. “Covid-19: how a virus is turning the world upside down.” BMJ. 2020;369:m1336. https://doi.org/10.1136/bmj.m1336.
Laurencin CT, Walker JM. A pandemic on a pandemic: racism and COVID-19 in Blacks. Cell Syst. 2020;11(1):9–10. https://doi.org/10.1016/j.cels.2020.07.002.
Lovallo WR. “Stress and health: biological and psychological interactions”. Thousand Oaks, CA: Sage Publications; 2016
Lub V. 2015. “Validity in qualitative evaluation: linking purposes, paradigms, and perspectives.” https://doi.org/10.1177/1609406915621406.
Marroquín B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020;293:113419. https://doi.org/10.1016/j.psychres.2020.113419.
McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Affairs (Project Hope). 2008;27(2):393–403. https://doi.org/10.1377/hlthaff.27.2.393.
McKnight-Eily LR, Okoro CA, Strine TW, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic. MMWR Morb Mortal Wkly Rep. 2021;70:162–6. https://doi.org/10.15585/mmwr.mm7005a3external.icon.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. https://doi.org/10.1177/109019818801500401.
Mills CK and Battisto J. 2020. Double jeopardy: COVID-19’s concentrated health and wealth effects in Black communities. New York: Federal Reserve Bank of New York.
Musselwhite K, Cuff L, McGregor L, King KM. The telephone interview is an effective method of data collection in clinical nursing research: a discussion paper. Int J Nurs Stud. 2007;44(6):1064–70. https://doi.org/10.1016/j.ijnurstu.2006.05.014.
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Committee on Community-Based Solutions to Promote Health Equity in the United States, Alina Baciu, Yamrot Negussie, Amy Geller, and James N. Weinstein. “The root causes of health inequity.” 2017. Accessed on December 12, 2021 from https://www.ncbi.nlm.nih.gov/books/NBK425845/.
Neelam K, Duddu V, Anyim N, Neelam J, Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain, Behav Immun - Health. 2021;10:100177. https://doi.org/10.1016/j.bbih.2020.100177.
Okoro J, Odionye T, Nweze B, Onuoha M, Ezeonwuka C, Owoh J, Nkire J. COVID-19 pandemic, psychological response to quarantine, and knowledge of the disease among inmates in a Nigerian custodial center. Emerald Open Res. 2020;2:26. https://doi.org/10.35241/emeraldopenres.13684.2.
Olding J, Zisman S, Olding C, Fan K. Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon. 2021;19(1):e9–e13.
Owens MR, Brito-Silva F, Kirkland T, et al. Prevalence and social determinants of food insecurity among college students during the COVID-19 pandemic. Nutrients. 2020;12(9):2515. https://doi.org/10.3390/nu12092515.
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Admin Pol Ment Health. 2015;42(5):533–44. https://doi.org/10.1007/s10488-013-0528-y.
Pfefferbaum B and North CS. 2020. “Mental health and the COVID-19 pandemic.” https://doi.org/10.1056/NEJMp2008017.
Porter C, Favara M, Sanchez A, and Scott D. 2021. “The impact of COVID-19 lockdowns on physical domestic violence: evidence from a list randomization experiment | Elsevier Enhanced Reader.” SSM-Popul Health 14. https://doi.org/10.1016/j.ssmph.2021.100792.
Prather AA. 2020. “Stress is a key to understanding many social determinants of health | Health Affairs Blog.” Health Affairs Blog. Accessed on September 14, 2021 from https://www.healthaffairs.org/do/10.1377/hblog20200220.839562/full/.
Rimer BK. Models of individual health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass; 2008. p. 41–66.
Schneiderman N, Ironson G, and Siegel SD. 2004. “Stress and health: psychological, behavioral, and biological determinants.” https://doi.org/10.1146/annurev.clinpsy.1.102803.144141.
Seedat S. Commentary on te special issue on disproportionate exposure to trauma: trauma, stress, and adversities and health disparities among disenfranchised groups globally during the COVID pandemic. J Trauma Stress. 2021;34(5):1061–7. https://doi.org/10.1002/jts.22746.
Seymour-Walsh, A. E., Bell, A., Weber, A., & Smith, T. (2020). Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural and Remote Health, 20, 6000. 10.22605/RRH6000
Shi C, Guo Z, Luo C, Lei C, Li P. The psychological impact and associated factors of COVID-19 on the general public in Hunan, China. Risk Manag Healthcare Policy. 2020;13:3187–99. https://doi.org/10.2147/RMHP.S280289.
Shim RS, Starks SM. COVID-19, structural racism, and mental health inequities: policy implications for an emerging syndemic. Psychiatr Serv. 2021;72(10):1193–8. https://doi.org/10.1176/appi.ps.202000725.
Snowden LR, Snowden JM. Coronavirus trauma and African Americans’ mental health: seizing opportunities for transformational change. Int J Environ Res Public Health. 2021;18(7):3568. https://doi.org/10.3390/ijerph18073568.
Stamps DL, Mandell L, Lucas R. Relational maintenance, collectivism, and coping strategies among Black populations during COVID-19. J Soc Pers Relat. 2021;38(8):2376–96. https://doi.org/10.1177/02654075211025093.
Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–98. https://doi.org/10.4278/0890-1171-10.4.282.
Stuijfzand S, Deforges C, Sandoz V, Sajin CT, Jaques C, Elmers J, Horsch A. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health. 2020;20(1):1230. https://doi.org/10.1186/s12889-020-09322-z.
Taylor S, Asmundson GJG. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021;16(2):e0246317. https://doi.org/10.1371/journal.pone.0246317.
Trier-Bieniek A. 2012. “Framing the telephone interview as a participant-centred tool for qualitative research: a methodological discussion:.” https://doi.org/10.1177/1468794112439005.
Vaughan E, Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health. 2009;99(Suppl 2(Suppl 2)):S324–32. https://doi.org/10.2105/AJPH.2009.162537.
Wheeler JM, Misra DP, Giurgescu C. Stress and coping among pregnant Black women during the COVID-19 pandemic. Public Health Nurs (Boston, Mass.). 2021;38(4):596–602. https://doi.org/10.1111/phn.12909.
Russell, B. S., Hutchison, M., Tambling, R., Tomkunas, A. J., & Horton, A. L. (2020). Initial Challenges of Caregiving During COVID-19: Caregiver Burden, Mental Health, and the Parent-Child Relationship. Child psychiatry and human development, 51(5), 671–682. https://doi.org/10.1007/s10578-020-01037-x
Acknowledgements
The authors would like to thank the members of the African American community for their valuable insights on their lived experiences during the COVID-19 pandemic.
Funding
This work was supported by the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) (Award Number: 5UL1TR0002243-03).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
Informed consent was obtained from all study participants.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gillyard, T., Davis, J., Parham, I. et al. Psychosocial Stressors and Coping Strategies Among African Americans During Early Stages of the COVID-19 Pandemic: a Qualitative Study. J. Racial and Ethnic Health Disparities 10, 373–386 (2023). https://doi.org/10.1007/s40615-022-01229-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01229-2