Abstract
Objective
The 2019 Coronavirus (COVID-19) results in a wide range of clinical severity and there remains a need for prognostic tools which identify patients at risk of rapid deterioration and who require critical care. Chest radiography (CXR) is routinely obtained at admission of COVID-19 patients. However, little is known regarding correlates between CXR severity and time to intubation. We hypothesize that the degree of opacification on CXR at time of admission independently predicts need and time to intubation.
Methods
In this retrospective cohort study, we reviewed COVID-19 patients who were admitted to an urban medical center during March 2020 that had a CXR performed on the day of admission. CXRs were divided into 12 lung zones and were assessed by two blinded thoracic radiologists. A COVID-19 opacification rating score (CORS) was generated by assigning one point for each lung zone in which an opacity was observed. Underlying comorbidities were abstracted and assessed for association.
Results
One hundred forty patients were included in this study and 47 (34%) patients required intubation during the admission. Patients with CORS ≥ 6 demonstrated significantly higher rates of early intubation within 48 h of admission and during the hospital stay (ORs 24 h, 19.8, p < 0.001; 48 h, 28.1, p < 0.001; intubation during hospital stay, 6.1, p < 0.0001). There was no significant correlation between CORS ≥ 6 and age, sex, BMI, or any underlying cardiac or pulmonary comorbidities.
Conclusions
CORS ≥ 6 at the time of admission predicts need for intubation, with significant increases in intubation at 24 and 48 h, independent of comorbidities.
Key Points
• Chest radiography at the time of admission independently predicts time to intubation within 48 h and during the hospital stay in COVID-19 patients.
• More opacities on chest radiography are associated with several fold increases in early mechanical ventilation among COVID-19 patients.
• Chest radiography is useful in identifying COVID-19 patients whom may rapidly deteriorate and help inform clinical management as well as hospital bed and ventilation allocation.
Similar content being viewed by others
Introduction
The 2019 novel coronavirus disease (COVID-19) pandemic is responsible for more than 100,000 deaths worldwide [1, 2]. Many centers routinely obtain chest radiography (CXR) at the time of initial triage to assess for disease severity. While previous Cochrane reviews evaluating the utility of CXR in acute lower respiratory tract infections have found no improvement of clinical outcomes, it is unclear whether CXR may affect management for COVID-19 patients [3]. Emerging studies have found that severity of CXRs may predict intubation and hospital admission in young and middle-aged adults (21–50 years old); however, little is known regarding the predictive power of CXR for the rate of clinical deterioration. This knowledge gap is especially important for older patients or those with underlying comorbidities who have been shown to be at higher risk of critical illness and rapid decompensation [4, 5].
COVID-19 has a wide range of clinical presentation, from asymptomatic to critically ill [5, 6]. Identification of markers at initial presentation which may be predictive of disease progression and specifically time to intubation is of critical importance, as resource (such as inpatient beds) and ventilation allocation are major considerations in the COVID-19 pandemic [7, 8]. Indeed, many have raised concerns regarding the ethical and appropriate management of ventilators in the setting of overwhelming numbers of rapidly and unpredictably deteriorating COVID-19 patients [9]. A priori knowledge of which patients may require intubation and in what time frame would be invaluable to clinicians and would allow for improved decision-making regarding resource allocation, planning, and in identifying those who may require additional clinical vigilance.
Accurate interpretation of chest radiograph may be confounded by comorbidities, such as underlying pulmonary or cardiac disease. As these disease processes have also been shown to be associated with increased morbidity and mortality among COVID-19 patients, elucidating possible confounders between CXR severity and these comorbidities is essential in understanding the independent utility of a CXR severity score in this cohort which is at highest risk of rapid clinical decline [10, 11].
This study aims to use a CXR severity index for objective assessment of COVID-19 radiographs at the time of admission to assess for associations with time to intubation and identify any confounders of CXR severity with known underlying risk factors for critical illness in COVID-19.
Materials and methods
From March 01 to March 31, 2020, an IRB-approved (STU: #00212323), HIPAA compliant, retrospective review of all patients with positive SARS-CoV-2 RT-PCR at a large urban academic hospital was performed, with a waiver of informed consent due to the retrospective nature of the study. Patients were included for analysis in this study if they were admitted into the hospital for further management and received a chest radiograph on the day of admission (Fig. 1).
Chest radiography and COVID-19 opacification rating score
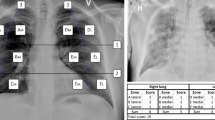
Selection of patients assessed with CXR was up to the discretion and clinical evaluation of the attending emergency physician. Portable CXRs were obtained with Carestream DRX Revolution (Carestream Health) and PA/lateral radiographs with Carestream Evolution (Carestream Health). Image interpretation was performed by two board-certified, cardiothoracic fellowship-trained radiologists (N.P. and B.A.) who were blinded to the patient’s clinical status. Chest radiographs were assessed for opacities in twelve lung zones. Lung zones were defined as apical (cranial to the azygous vein contour), mid (between azygous vein contour and superior cavoatrial junction), and basal (below superior cavoatrial junction), and were further divided into medial and lateral segments using the mid-clavicular line as a landmark (Fig. 2). A COVID-19 opacification rating score (CORS) was generated by assigning one point for each lung zone in which an opacity was observed. Patients with discordant scores were assigned the more severe score for the purpose of analysis. Involvement of at least 6 lung zones was used as a cutoff for analysis. The Cohen’s kappa coefficient was used to assess interobserver agreement.
Chest radiography and opacification severity zones. a A 34-year-old man presented to the emergency department with shortness of breath was found to have COVID-19. b The lungs are divided into twelve lung zones. Lung zones were defined as apical (cranial to the azygous vein contour), mid (between azygous vein contour and superior cavoatrial junction), and basal (below superior cavoatrial junction), and were further divided into medial and lateral segments using the mid-clavicular line as landmark. Opacities were identified in the right mid medial, right basal medial, and left mid medial lung zones. A CORS of 3 was assigned. c A 48-year-old woman presented to the emergency department with cough, chest pain, and shortness of breath was diagnosed with COVID-19. Multiple opacities are identified in the bilateral lungs. This patient rapidly decompensated and was intubated within 24 h from acquisition of this radiograph. d Opacities are defined in all twelve defined lung zones; a CORS of 12 was assigned
COVID-19 RT-PCR and clinical data abstraction
The COVID-19 assay utilized primer, probes and reagents, and the procedure designated by the CDC and the Institutional Diagnostic Molecular Biology Laboratory using real-time PCR method.
Other abstracted data included age, sex, date of presentation, duration of symptoms, presence of fever, D-dimer, need for supplementary oxygen at the time of imaging, necessity and time of intubation, BMI, and underlying pulmonary or cardiac comorbidities. A patient was considered to have a pre-existing pulmonary comorbidity if they had a history of any of the following: chronic obstructive pulmonary disease (COPD), asthma, or obstructive sleep apnea (OSA). A patient was considered to have a pre-existing cardiac comorbidity if they had a history of myocardial infarction (MI), coronary artery disease (CAD), or heart failure (HF).
Intubation and admission criteria
During the study period, the clinical protocol in the hospital required that patients be admitted to the ICU with consideration of intubation if supplemental nasal cannula oxygen requirements exceeded 5 l. Higher levels of oxygen support were not allowed on the medical floors and no non-invasive positive pressure ventilation was used in this time period. Admission and imaging criteria were per the discretion of the emergency department and inpatient medicine physician.
Statistical analysis
Continuous variables assessed included age and BMI. Categorical variables assessed included sex, age by category (under and over 50 years old), BMI (by WHO obesity classifications), and any pulmonary or cardiac comorbidities, as previously defined. The primary outcome assessed was intubation during admission, and at 24 h and at 48 h. When examining the association between independent variables and outcomes, a feedforward stepwise approach was used given the propensity for independent variables to be correlated to each other.
Univariable linear and logistic regressions or Fisher exact tests were performed to assess for correlation between independent variables and intubation, as well as with CORS ≥ 6 and reader disagreement.
Kaplan-Meier (KM) curves were generated with intubation as the end point. All patients were followed until discharge or death. Censorship for intubation was performed at 7 days (168 h). Independent variables assessed for KM analysis included CORS ≥ 6, age, sex, BMI class, and the presence of any pulmonary comorbidities or cardiac comorbidities. Log-rank tests were used to assess for significant differences in intubation at 7 days.
Significance for statistical analysis was set at α < 0.01 and a Bonferroni correction for multiple hypotheses was applied. For associations with intubation at 7 days, eight independent variables were assessed and the threshold for significance was set at p < 0.0013 (0.01/8). For CORS associations with patient characteristics, seven independent variables were assessed, and therefore, the threshold for significance was accepted at p < 0.0014 (0.01/7). For associations with the need for intubation at 24 h, 48 h, and during admission, the threshold for significance was set at p < 0.01, as these were considered independent analyses.
Analyses and graph design were conducted using StataSE, version 14.2 (StataCorp), GraphPad Prism version 6.01 (GraphPad Software) and Python version 3.5.2 (statsmodels v0.6.1, SciPy 0.18.1, SciKit Learn v0.18.1) (Python Software Foundation).
Results
Patient cohort
Patient inclusion criteria are detailed in Fig. 1. A summary of patient demographic information and clinical history at presentation is presented in Table 1. A total of 140 COVID-19-positive patients were included in the study (median age 58.5, SD = 16.2; 44.2% female) with a median symptom duration of 7 days at the time of presentation. Forty (40) patients reported a history of cardiovascular disease and 22 reported a history of chronic pulmonary disease. Average BMI for the patient population was 31.1 of which 15 patients (10.7%) were characterized as having class III obesity.
Chest radiography
A total of 134 patients received AP portable radiographs of the chest; 6 received PA and lateral radiographs. Two of 134 AP portable radiographs were imaged in the supine position and 5 in the semi-erect position; the remaining 127 were imaged upright. The CORS system is described in Fig. 2. The Cohen’s kappa for agreement on CORS ≥ 6 was 0.65. Seventy-three (52%) patients presented with CORS < 6 and 67 patients presented with CORS ≥ 6 at the time of admission. A distribution of scores is presented in Fig. 3.
Distribution of COVID-19 opacification rating score (CORS) among 140 admitted patients. CORS for the overall cohort is presented in panel a. Lung zones were demarcated as described in Fig. 2 and a point assigned for opacity in each zone. The CORS is the summation of total opacity points on chest radiograph. The red line demarcates the cutoff of CORS ≥ 6 which was used for analysis in this study. Frequencies and distribution of lung zone opacities on the admission CXR are presented in panel b. The CORS of patients stratified by need for intubation at 7 days is presented in panel c and d
Association of CORS with intubation
A total of 47 (34%) patients were intubated in this cohort, 40 (29%) of which were intubated within 7 days after admission and 3 (6%) within the first 2 h. No patients were intubated at the time of CXR acquisition. Mean time from symptom onset to intubation was 10.2 days (SD 6.5). CORS ≥ 6 was predictive of higher rates of intubation during the hospital stay (OR 6.1 [99% CI 2.1–18.1], p < 0.001). Log-rank testing demonstrated that a CORS ≥ 6 was predictive of higher rates of intubation within 7 days of admission (Fig. 4, CORS ≥ 6, 46% intubated; CORS < 6 , 14.3% intubated, p < 0.0001). CORS ≥ 6 was also associated with significantly higher rates of early intubation at 24 h and 48 h after admission compared with CORS < 6 (Table 2, 24 h intubation OR 19.8, [99% CI 1.3–298], p < 0.001; 48 h intubation OR 28.1 [99% CI 1.9–416], p < 0.001).
a Chest radiograph severity score predicts early intubation after admission. Kaplan-Meier curves demonstrate a statistically significant difference in time to intubation after admission in patients with CORS ≥ 6 (****p < 0.0001, log-rank test). The number of patients at risk in each 24-h period is displayed below the Kaplan-Meier curves. A Kaplan-Meier curve illustrating the proportion of patients intubated in the early admission period (0–48 h) is shown in panel b
Patient comorbidities, clinical variables, and association with CORS and intubation
No significant correlation was found between CORS ≥ 6 and patient age category (p = 0.77), sex (p = 0.23), BMI category (p = 0.08), or underlying pulmonary (p = 0.09) or cardiac (p = 0.09) comorbidities (Table 1).
Kaplan-Meier analysis of time to intubation with age categories (below and above 50 years old) (p = 0.05), sex (p = 0.23), BMI (by WHO categories, p = 0.14), underlying pulmonary disease (p = 0.01), and underlying cardiac comorbidities (p = 0.09) did not show significantly higher rates of intubation (supplemental Figure 1).
Twenty-one patients whom did not require supplemental oxygen at the time of radiograph acquisition demonstrated CORS ≥ 6 and eventually required intubation. Seventy-seven patients underwent D-dimer laboratory evaluation and the mean D-dimer was 462 (SE 99.5). The mean D-dimer of those with CORS > 6 was 629.5 (SE 176.5) versus 262.3 (SE 37.9) in those with CORS < 6 (p = 0.07).
Chest radiography among discharged patients
Chest radiography was available for 39 of 85 patients whom were discharged from the ED. The median CORS from this cohort was 1 (IQR 2, range 0–8). Two patients from this cohort had CORS ≥ 6. One discharged patient with an initial CORS of 0 was admitted to an outside hospital 4 days later and quickly recovered without need for ventilatory support.
Discussion
The role of imaging has rapidly evolved in the COVID-19 pandemic [12,13,14]. CXR is routinely obtained at the time of admission due to its availability, low cost, and streamlined disinfection protocols compared with CT. As such, a radiograph-based severity index that predicts need for intubation and particularly early intubation is invaluable in the management and triage of COVID-19 patients and for planned allocation of hospital resources. In this study, we show that CORS ≥ 6 on CXR at the time of admission is independently associated with need for early intubation, with significantly higher rates of intubation at 24 and 48 h.
There are emerging COVID-19 clinical prediction tools using clinical signs and laboratory values; however, none include a graded severity of CXR. Compared with laboratory tests and CT, CXR is more rapidly obtained, can be immediately evaluated, and is readily available with facile device decontamination, factors which are especially advantageous in the outpatient or urgent care setting. Toussie et al utilized an alternative CXR severity scoring system to identify risk of critical illness in young and middle-aged adults (21–50 years old) [4]. However, there remained an unmet knowledge gap in the utility of CXR in the older population, who were excluded from the aforementioned study, many of whom are at the highest risk of intubation. Furthermore, most of the comorbidities that have been shown to be related to intubation are not sufficiently prevalent in the young population, precluding analysis addressing whether CXR severity is independently associated with critical illness or is confounded by other clinical risk factors [5, 6, 10]. In our study, we address this knowledge gap, as a robust statistical analysis did not find any significant associations between CXR severity and multiple cofounders, including BMI, cardiac (heart failure, prior myocardial infarction, coronary artery disease), or pulmonary (obstructive sleep apnea, asthma, COPD) comorbidities, suggesting that CXR severity is an independent risk factor which primarily drives the association with need for intubation, even among elderly patients. A second novel and important addition of this study is the association of CXR severity with a specific time to intubation (< 48 h), which is invaluable information when clinically assessing and triaging patients, as well as for planning availability of hospital resources such as ventilators. We also corroborate that initial chest radiograph is predictive of need for intubation at the index admission, with an odds ratio above 6. Together, these data argue that CXR is a useful prognostic tool at presentation for COVID-19 patients, whom may present with a wide range of clinical symptoms and degree of respiratory compromise.
Kaplan-Meier analysis of age, BMI class, pulmonary and cardiac comorbidity and sex did not independently predict time to intubation. The lack of an association for these variables may be related to sample size in this study. This finding is concordant with prior studies which have identified these factors as being associated with critical illness, and may have reached significance in a larger cohort study [5, 8, 10, 11, 15].
Censorship for analysis was performed at 7 days (168 h), as intubation in this time period was felt to reflect a reasonable clinical correlate to the index CXR. Beyond 7 days of inpatient time, additional nosocomial-acquired disorders such as superinfection or venous thromboembolism may play a role in clinical decline, and thus, the intubation event would not accurately reflect a predicted outcome from the admission CXR [16, 17]. For similar reasons, survival analysis and mortality censorship analysis were not performed, as any significant associations between the index CXR and death would likely be due to an unassessed confounder. The CORS therefore has limited value in prediction of mortality. Previous studies have only assessed associations between the index CXR and intubation anytime during the hospital admission and are likely biased by unrelated confounders and variations in treatment which occur throughout the hospital course. This bias is partially accounted for by the KM analysis and censorship at 7 days performed here.
Independent reviewers reached substantial agreement in assessing CXR for CORS ≥ 6. This suggests that the CORS grading system will be reproducible in other hospitals and practice settings, thereby providing a quick and simple tool radiologist can use to inform ordering clinicians on the severity of illness. While emerging research has shown utility in artificial intelligence and automated assessment software, these are often not readily available to all radiologists, and may require significant resources to implement compared with CORS [18].
This study intentionally included only patients from the month of March, when the criteria for intubation were consistent throughout the time period. Patients in this cohort were admitted to the intensive care unit with consideration of intubation if supplemental nasal cannula oxygen requirements exceeded 5 l. No non-invasive positive pressure ventilation was used in this time period. As the clinical management of COVID-19 changes, the timing and need for intubation and correlation with CXR severity may shift accordingly.
This study has limitations. This is a retrospective study of patients at a single institution in a major metropolitan area. However, an advantage of a single-center study is the exclusion of heterogeneity in intubation criteria as well as uniform availability of resources, such as ventilators. No patients were unable to receive ventilation or admission due to resource constraints, therefore eliminating bias from patients who likely required elevation of care but were delayed due to availability. Only patients with available CXR were analyzed for this study, and the choice of the admitting provider to obtain imaging may bias towards those with higher clinical concern. This study included only inpatients, which select for only the most ill and may portend higher rates of intubation. However, as excluded patients that were discharged (and did not return to the emergency department) are presumed never to require critical care, this study likely captures all patients that required intubation in their disease course. Nonetheless, further research identifying correlates between time to intubation among all patients would be helpful for further validation of this CXR severity score.
The severity of the chest radiograph at the time of admission predicts need and time to intubation, with significant increases in intubation at 24 and 48 h, independent of comorbidities. The use of CXR severity may help guide clinical management, triage, and allocation of hospital resources and ventilators.
Abbreviations
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CI:
-
Confidence Interval
- COPD:
-
Chronic obstructive pulmonary disease
- CORS:
-
COVID-19 opacification rating score
- COVID-19:
-
2019 Coronavirus
- CXR:
-
Chest radiograph
- HF:
-
Heart failure
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- KM:
-
Kaplan-Meier
- MI:
-
Myocardial infarction
- OR:
-
Odds ratio
- OSA:
-
Obstructive sleep apnea
- PCR:
-
Polymerase chain reaction
- SD:
-
Standard deviation
References
CDC (2020) Coronavirus disease 2019 (COVID-19). Available from: https://www.cdc.gov/media/dpk/diseases-and-conditions/coronavirus/coronavirus-2020.html
WHO (2020) Coronavirus disease 2019 (COVID-19) situation report. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200317-sitrep-57-covid-19.pdf?sfvrsn=a26922f2_4
Cao AM, Choy JP, Mohanakrishnan LN, Bain RF, van Driel ML (2013) Chest radiographs for acute lower respiratory tract infections. Cochrane Database Syst Rev 12:CD009119
Toussie D, Voutsinas N, Finkelstein M et al (2020) Clinical and chest radiography features determine patient outcomes in young and middleaged adults with COVID-19. Radiology 297(1):E197–E206
Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054-1062
Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 Hospitalized patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 323(11):1061–1069
Truog RD, Mitchell C, Daley GQ (2020) The toughest triage - allocating ventilators in a pandemic. N Engl J Med 382(21):1973–1975
Liang W, Liang H, Ou L et al (2020) Development and validation of a clinical risk score to predict the occurrence of critical illness in Hospitalized patients with COVID-19. JAMA Intern Med 180(8):1081–1089
White DB, Lo B (2020) A framework for rationing ventilators and critical care beds during the COVID-19 Pandemic. JAMA 323(18):1773–1774
Cummings MJ, Baldwin MR, Abrams D et al (2020) Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 395(10239):1763–1770
Goyal P, Choi JJ, Pinheiro LC et al (2020) Clinical characteristics of Covid-19 in New York City. N Engl J Med 382(24):2372–2374
Zu ZY, Jiang MD, Xu PP et al (2020) Coronavirus Disease 2019 (COVID-19): a perspective from China. Radiology 296(2):E15–E25
Li Y, Xia L (2020) Coronavirus Disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol 214(6):1280–1286
ACR (2020) ACR Recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. 03/25/2020]. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
Bhatraju PK, Ghassemieh BJ, Nichols M et al (2020) Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med 382(21):2012–2022
Tess BH, Glenister HM, Rodrigues LC, Wagner MB (1993) Incidence of hospital-acquired infection and length of hospital stay. Eur J Clin Microbiol Infect Dis 12(2):81–86
Heit JA, Silverstein MD, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ 3rd (2000) Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 160(6):809–815
Li MD, Arun NT, Gidwani M, et al (2020) Automated assessment of COVID-19 pulmonary disease severity on chest radiographs using convolutional Siamese neural networks. Radiology Artificial Intelligence
Acknowledgments
We would like to thank Daniel Cruz for help in acquiring a comprehensive list of COVID-19 patients included in this study.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Nicholas Xiao.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Meagan Bechel, one of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplemental eFigure 1
Kaplan-Meier curves of COVID-19 risk factors with intubation at 7 days after admission (PDF 198 kb)
Rights and permissions
About this article
Cite this article
Xiao, N., Cooper, J.G., Godbe, J.M. et al. Chest radiograph at admission predicts early intubation among inpatient COVID-19 patients. Eur Radiol 31, 2825–2832 (2021). https://doi.org/10.1007/s00330-020-07354-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07354-y