Opportunities to reduce the radiation exposure during computed tomography to assess the changes in the lungs in patients with COVID-19: use of adaptive statistical iterative reconstruction
- Authors: Filatova D.A.1, Sinitsin V.E.1, Mershina E.A.1
-
Affiliations:
- Lomonosov Moscow State University
- Issue: Vol 2, No 2 (2021)
- Pages: 94-104
- Section: Original Study Articles
- URL: https://jdigitaldiagnostics.com/DD/article/view/62477
- DOI: https://doi.org/10.17816/DD62477
- ID: 62477
Cite item
Abstract
BACKGROUND: Several COVID-19 patients are subjected to multiple imaging examinations during hospitalization, the cumulative effect of which can significantly increase the total dose of radiation received. The effective radiation dose can be reduced by lowering the current and voltage of the X-ray tube, but this reduces image quality. One possible solution is to use adaptive statistical iterative reconstruction technology on the «raw» CT data. Recently, data on the efficacy of low-dose CT (LDCT) in the diagnosis of COVID-19 have appeared in the literature.
AIM: To analyze the quality and diagnostic value of LDCT images of the lungs after applying an iterative processing algorithm and to assess the possibility of reducing the radiation load on the patient when diagnosing COVID-19.
MATERIALS AND METHODS: Patients from the Infectious Diseases Department of the Moscow State University Hospital participated in the prospective study. CT examinations were performed at the time of patient admission and discharge and were repeated as needed during hospitalization. In the first study, a standard CT protocol with a tube voltage of 120 kV and automatic current modulation in the range of 200–400 mA was used; in repeated CT scans, the LDCT protocol was used with reduced tube voltage parameters (100 or 110 kV) and automatic current modulation in the range of 40–120 mA. To assess the diagnostic value of LDCT in comparison with standard CT, a survey was conducted among doctors from the Department of Radiation Diagnostics at Moscow State University Hospital. The questionnaire included a comparison of the two methods for identifying the following pathological processes: «ground-glass» opacities, compaction of the lung tissue with reticular changes, areas of lung tissue consolidation, and lymphadenopathy.
RESULTS: The study included 151 patients. The average age was 58±14.2 years, with men accounting for 53.6% of the population. During LDCT the radiation load was reduced by 2.96 times on average, CTDI by 2.6 times, DLP by 3.1 times, the current on the tube by 1.83 times, and the voltage on the tube by 1.2 times. The results indicate that the effectiveness of detecting the main signs of viral pneumonia and assessing the dynamics of the patient’s condition does not differ significantly from CT performed according to the standard protocol.
CONCLUSIONS: The results of a comparison of standard and low-dose CT show that there is no significant loss of diagnostic information and image quality as the radiation load is reduced. Thus, chest LDCT can be used to successfully diagnose COVID-19 in routine practice.
Keywords
Full Text
BACKGROUND
During the coronavirus disease 2019 (COVID-19) pandemic, computed tomography (CT) studies are used to diagnose coronavirus pneumonia in both outpatient and inpatient settings and are recommended to be performed in patients suspected or verified with COVID-19 on the day of hospitalization for an initial examination, then repeatedly after 2–3 days if the required therapeutic effect is not achieved and then after 5–7 days in the absence or improvement of symptoms dynamics [1–5].
A number of patients with COVID-19 undergo multiple imaging studies during hospitalization, whose cumulative effect can significantly increase the total dose of radiation received. The principle “as low as reasonably achievable” (ALARA) states that whenever radiation is required, the impact should be ALARA. Bearing in mind this important principle, it is extremely important to remember that any CT scan must be accompanied by a justification of examination and optimization of radiation dose [6]. CT scans are significant aid in diagnosing COVID-19; however, the potential to increase radiation exposure of large numbers of patients across the country cannot be ignored. Maintaining the balance between the need for efficient imaging for rapid diagnostics and efforts to minimize radiation exposure is important.
Effective dose of radiation during CT studies can be decreased by reducing the current and voltage of X-ray tube; however, this leads to image quality distortion due to an increase in the amount of noise and artifacts. A possible solution to this problem is the introduction of technology adaptive to statistical iterative reconstruction of CT “raw data,” for example, using the Adaptive Statistical Iterative Reconstruction (ASIR) technology and numerous similar methods [7–9].
Recently, data on the efficiency of low-dose CT (LDCT) in diagnostics of COVID-19 compared with standard one were presented in literature. It should be noted that CT with a radiation dose of 0.2 mSv or less is considered low dose. In a retrospective study, LDCT with iterative reconstruction in the diagnostics of COVID-19 demonstrated sensitivity, specificity, and predictive value of approximately 90%. Values of these parameters increased to 96% if patients had symptoms for >48 hours. Disease probability increased from 43.2% (before the test) to 91.1% or 91.4% (after the test) in patients with a positive CT scan, whereas the probability of disease decreased from 43.2% (before the test) to 9.6% or 3.7% (after the test) in patients with negative CT result. Additionally, LDCT revealed an additive diagnostic advantage in patients with concomitant bacterial pneumonia or an alternative diagnosis other than COVID-19 [10]. Research in this promising field is actively performed.
This study aimed to analyze the quality and diagnostic value of LDCT images of the lungs after applying the ASIR processing algorithm and to assess the possibility of reducing radiation exposure of patients diagnosed with COVID-19.
METHODS
Study design
Patients undergoing inpatient treatment at the infectious diseases department of the M.V. Lomonosov Moscow State University Medical Research and Education Center took part in a prospective, single-center, uncontrolled study. CT examinations were performed upon patient admission and discharge, then were repeated as clinically required during the period of hospitalization, but at least once every 5 days. Study 1 was conducted in all patients in the standard CT mode, subsequent ones were conducted in LDCT mode.
The primary endpoint of the study was the absence of a significant loss of diagnostic information during LDCT compared to standard CT.
Inclusion criteria
Inclusion criteria included infection with COVID-19 verified by molecular genetic studies (polymerase chain reaction method, PCR), and undergoing inpatient treatment.
Conducting conditions
The study was conducted in the infectious diseases department of the Moscow State University Medical Research and Education Center with the involvement of patients who were hospitalized with COVID-19.
Study duration
The study was conducted from April 21 to May 11, 2020.
Medical intervention description
CT of the lungs and chest organs was performed on a 32-row Somatom Scope CT manufactured by Siemens (Germany). Studies were conducted with a slice thickness of 1 mm. The first study used a standard CT protocol with a tube voltage of 120 kV, with an automatic modulation current of 200–400 mA; with repeated CT, the LDCT protocol was used with reduced parameters of tube voltage (100 or 110 kV) and automatic modulation of tube current of 40–120 mA; the ASIR algorithm was used to reduce radiation exposure. All images obtained in DICOM format were stored in the Radiological Information Network of the Moscow State Scientific and Educational Center of Moscow State University. Syngo.via workstations (Siemens, Germany) were used for CT processing and analysis.
A questionnaire survey was conducted among the doctors of the Department of Radiation Diagnostics of the Medical Research and Education Center of the M.V. Lomonosov Moscow State University to assess the diagnostic value of LDCT in comparison with standard CT. The questionnaire included a comparative description of two methods in identifying pathological processes, namely ground glass opacity induration of the lung tissue, ground glass opacity induration with reticular changes (thickened interlobular septa; “patchwork” presentation, crazy paving), areas of consolidation of lung tissues, and lymphadenopathy. Medical specialists evaluated each of the two methods on a five-point scale, where the worst detectability of a particular pathological process corresponded to 1 point, the best detectability corresponded to 5 points, and then the arithmetic mean was calculated for each item. In conclusion, it was proposed to assess the efficiency of LDCT diagnostics of COVID-19. Each study was assessed by two medical specialists, and decision was independently made in each case.
Primary study outcome
The primary outcome of the study was comparable diagnostic value of CT performed according to the standard protocol and LDCT.
Ethical considerations
The subject of this article was approved at a meeting of the Local Ethics Committee of the Medical Research and Education Center of the M.V. Lomonosov Moscow State University, dated May 25, 2020 (within the research project on diagnostics and treatment of COVID-19 at the Medical Research and Education Center of the M.V. Lomonosov Moscow State University).
Statistical analysis
Statistical analysis was performed using MS Office Excel software.
RESULTS
Study participants
A total of 151 patients who underwent inpatient treatment at the infectious diseases department of the Medical Research and Education Center of the M.V. Lomonosov Moscow State University participated in the study. The average age of patients was 58 ± 14.2 years; wherein 70 were women (46.4%) and 81 were men (53.6%). COVID-19 diagnosis was confirmed by PCR results.
Main research results
Characteristics of study 1 (standard CT) included average radiation exposure of 3.76 ± 1.28 mSv; average computed tomography dose index (CTDI) of 6.69 ± 2.18 mGy; average dose length product (DLP) of 222.28 ± 76.33 mGy/cm; average tube current of 2165.97 ± 682.83 mA/s; and average tube voltage of 129.43 ± 3.21 mV. Characteristics of subsequent studies (LDCT) included radiation exposure of 1.27 ± 0.47 mSv; CTDI of 1.57 ± 1.40 mGy; DLP of 73.01 ± 19.94 mGy/cm; tube current of 1182.55 ± 366.55 mA/s; and tube voltage of 111.79 ± 5.73 mV. If a patient underwent several LDCT studies, the arithmetic mean between them was considered when calculating statistical indicators.
The following results were obtained from standard and low-dose CT comparison. During LDCT, radiation exposure decreased on average by 2.96 times, CTDI reduced by 2.6 times, DLP reduced by 3.1 times, tube current reduced by 1.83 times, and tube voltage reduced by 1.2 times. These values are presented in Table 1.
Table 1. Comparative characteristics of standard and low-dose computed tomography
Indicator | Standard CT | Low-dose CT | Difference, times |
Average radiation exposure, mSv | 3.76±1.28 | 1.27±0.47 | 2.96 |
CTDI, mGy | 6.69±2.18 | 1.57±1.40 | 2.6 |
DLP, mGy/cm | 222.28±76.33 | 73.01±19.94 | 3.1 |
Average tube current, mA/s | 2165.97±682.83 | 1182.55±366.55 | 1.83 |
Tube voltage, mV | 129.43±3.21 | 111.79±5.73 | 1.2 |
Note. CT, computed tomography; CTDI (Computed Tomography Dose Index), average computed tomography dose index; DLP, dose length product.
Table 2 presents the results of the survey questionnaire of doctors of the Department of Radiation Diagnostics of the Medical Research and Education Center of the M.V. Lomonosov Moscow State University for assessing the diagnostic accuracy of LDCT in comparison with standard CT.
Table 2. Results of the survey questionnaire of doctors of the Department of Radiation Diagnostics of the Medical Research and Education
Center of the M.V. Lomonosov Moscow State University
Characteristics | Standard CT | LDCT |
Identification of the lung tissue induration by the type of ground glass opacity | 5 | 5 |
Identification of induration areas by the type of ground glass opacity with reticular changes (thickened interlobular septa)―presentation of patchwork, crazy paving | 5 | 4,43 |
Identification of lung tissue consolidation areas | 5 | 5 |
Detection of lymphadenopathy | 5 | 4 |
Note. The average values of points given for each item are indicated: the minimum point is 1, the maximum is 5. CT, computed tomography; LDCT, low-dose computed tomography.
Table 2 demonstrates that with LDCT, the efficiency of detecting the main signs of viral pneumonia, and assessment of the patient’s condition dynamics does not significantly change compared to that of standard CT. It should also be noted that, according to survey results, 7 doctors (100% of those surveyed) believe that LDCT is effective for COVID-19 diagnostics.
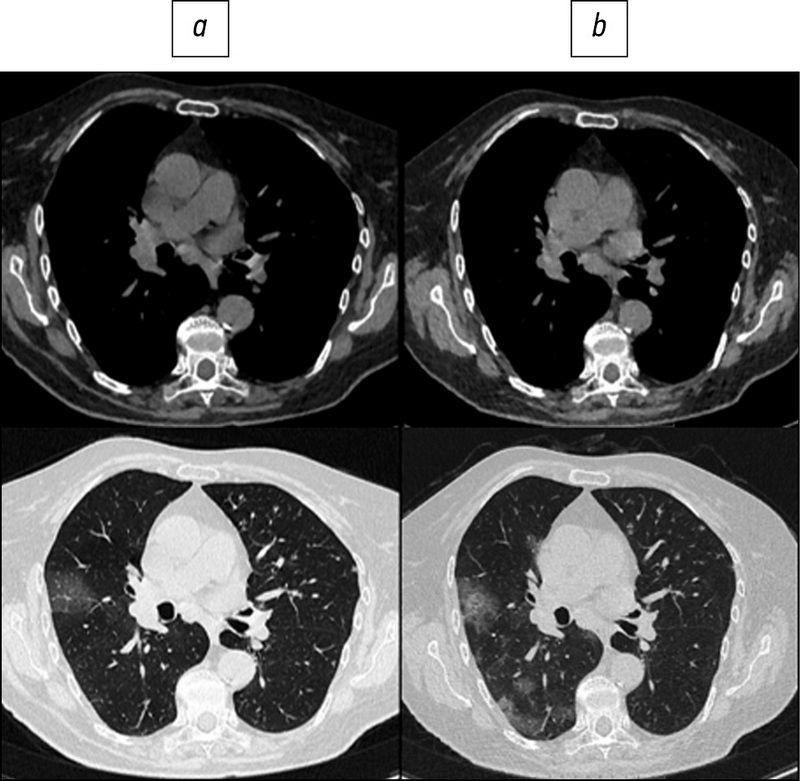
Fig. 1. Patient, 78 years old: standard computed tomography at admission was performed with a radiation load of 2.5 mSv (a), low-dose computed tomography - 1.0 mSv (b).
Fig. 2. Patient, 72 years old: standard computed tomography at admission was performed with radiation exposure of 2.1 mSv (a), low-dose computed tomography - 0.87 mSv (b).
Fig. 3. Patient, 60 years old: standard computed tomography at admission was performed with a radiation load of 3.3 mSv (a), low-dose computed tomography - 1.1 mSv (b).
Fig. 4. Patient, 46 years old: standard computed tomography at admission was performed with a radiation dose of 5.6 mSv (a), low-dose computed tomography - 1.7 mSv (b).
Fig. 5. Patient, 40 years old: standard computed tomography at admission was performed with radiation exposure of 6.8 mSv (a), low-dose computed tomography - 2.0 mSv (b).
Fig. 6. Patient, 56 years old: standard computed tomography at admission was performed with a radiation load of 1.6 mSv (a), low-dose computed tomography - 0.87 mSv (b).
Here are illustrative examples of clinical cases (Figs. 1–6), demonstrating the similarity of diagnostic value of two aforementioned research methods. Columns on the left (a) show images of a standard CT scan performed upon admission of the patient to the hospital, and columns on the right (b) present LDCT over time. The top line of images indicates the pulmonary window mode, whereas the bottom line indicates the mediastinal window mode. For comparison, values of radiation exposure in each case are presented. Time intervals between standard CT and LDCT were 2–7 days; thus, the primary endpoint was reached in all patients enrolled in the study.
Adverse events
During the study, no adverse events were recorded because of CT according to the standard protocol and LDCT.
DISCUSSION
Main research result summary
Study results confirm the absence of significant loss of diagnostic information in chest LDCT in patients with COVID-19; thus, chest LDCT can be routinely used for successful diagnostics of this disease.
Main research result discussion
In the absence of etiotropic treatment of COVID-19, it is especially important to diagnose the disease at an early stage and immediately isolate the infected person. According to clinical guidelines, COVID-19 diagnosis is established based on clinical examination, epidemiological anamnesis data, and laboratory testing results [11]. The task of etiological laboratory diagnostics comprises searching for severe acute respiratory syndrome coronavirus 2 ribonucleic acid using nucleic acid amplification methods (reverse transcription PCR, RT-PCR). Pathogen detection in a nasopharyngeal smear is possible as early as a week before the onset of clinical manifestations of the infection [12]. Nevertheless, evidence that RT-PCR can give false negative results was reported. Therefore, Ch. Long et al. [13] reported that 35 patients had CT signs of characteristic pneumonia among 36 patients diagnosed with COVID-19, whereas a positive RT-PCR result was obtained for the first time in only 30 patients. In the remaining six cases, repeated testing was performed, and the test result was positive in three of them at the second test (after 2 days) and in three more cases at the third test (after 6 days). Thus, CT sensitivity was 97.2%, and RT-PCR in study 1 was 84.6% [13]. In a study by Y. Fang et al. [14], similar results were obtained, when CT sensitivity was 98% and that of RT-PCR was 71% (in study 1, the positive result was obtained in 36 of 51 patients with symptoms of pneumonia on CT and a suitable epidemiological history; the diagnosis was further confirmed in 12 patients in study 2, 2 patients in study 3, and 1 patient in study 4). Assumed reasons that the RT-PCR sensitivity in COVID-19 diagnosis was lower than that of CT, including the imperfection of nucleic acid amplification technologies, the variability of the sensitivity threshold of tests from different manufacturers, low viral load, and wrong technique of sampling material for analysis. Additionally, the number of viral particles varies depending on the site where the material for analysis is taken, as evidence revealed that it is preferable to examine the sputum first, followed by a nasopharyngeal swab in sensitivity [15]. Thus, despite a negative RT-PCR result, CT is recommended to visualize changes in the lungs if the patient has characteristic symptoms and epidemiological history. In case of CT signs of pneumonia, it is necessary to take measures for emergency isolation of the patient, after which a repeated laboratory analysis should be performed.
In the context of an increased number of CT examinations, an issue of a significant increase in radiation exposure and associated risk arise, for example, the evidence that approximately 2% of cancers in the USA are associated with radiation doses received as CT result [16]. Despite the absence of major epidemiological studies on this subject, a large amount of data on radiation-induced cancer in survivors of atomic bombs dropped on Japan in 1945 was reported. In the subgroup of people who received radiation doses in the range from 5 to 150 mSv, a significant increase was observed in the overall risk of developing cancer, the average dose in this subgroup was 40 mSv [17], and the average effective radiation dose for standard chest CT is 5 mSv [18]. As for LDCT of the chest with radiation exposure of 0.4 mSv, no sufficient evidence of efficacy in the context of screening and diagnostics of COVID-19 is currently reported [3].
Radiation dose received by a patient during CT scan depends on tube current strength, voltage, scan time, slice thickness, scan volume, and interval. Scanning time is reduced with the use of modern models of spiral tomographs; however, radiation exposure sometimes even increases due to increased current strength and scan volume. Under these conditions, it is reasonable to resort to radiation dose reduction techniques. The dose is directly proportional to the tube current. Recently, several studies showed that chest LDCT at 10–140 mAs does not significantly reduce the image quality, and nodular structures are still observed [19–21]. In their study, X. Zhu et al. [22] demonstrated a linear correlation between the tube current and the DLP at a constant voltage and scan time, and also assessed the feasibility of optimization of radiation dose by reducing the tube current. By comparing images obtained at different CTDI values, the threshold value of this parameter was determined, which enables to obtain images without a significant loss of information content (25 mAs), and with an increase in the thickness of sections, the loss of image quality occurred more slowly. Statistical analysis revealed no significant difference between images obtained at 115, 40, and 25 mAs. Thus, 25 mAs or more is an acceptable exposure parameter to provide satisfactory image quality for chest CT, whereas CTDI at 25 mAs was reduced by 70% compared to CTDI at 115 mAs. Despite the accuracy of this parameter, clinicians should be aware that its value may vary with different CT systems; additionally, it must be adjusted considering the biological characteristics of patients (for example, the radiation dose should be increased for obese patients and when examining the upper lobe of the lung due to the false shadow caused by the scapula). Threshold values of CDTI parameter obtained in this study are consistent with the results of the study by T. Kubo et al. [23], where standard and low-dose CTs were compared to determine the main characteristics of lung lesions, which enabled us to confirm or rule out malignant nature. Parameters of 20–50 mAs were sufficient to determine the nature of the lesion without additional standard CT. Edge characteristics, calcification, and lobulation, as well as pleural response, standard and low-dose CTs showed the same efficiency to determine parameters of lesions as structure.
For many years, the question of LDCT safety in screening for oncological diseases, for example, lung cancer, has remained controversial [24]. In their study, C. Rampinelli et al. [25] analyzed the possible risks of radiation lung cancer and leukemia in healthy people who had been regularly screened using LDCT for 10 years. It turned out that the total cumulative dose of radiation was approximately 9 mSv for men and 13 mSv for women, which is equivalent to one standard CT scan. Additionally, given that the average dose from background sources in the USA is approximately 30 mSv over 10 years, it can be concluded that LDCT screening accounts for only 1/3 of the exposure to natural background radiation over the same period. Study results revealed that after 10 years of screening with LDCT, in 5203 patients aged over 50 years old who are asymptomatic with smoking experience of more than 20 pack-years, approximately 1.5 cases of lung cancer, and 2.4 cases of other types of cancer were caused by radiation exposure. Compared to the number of cases of lung cancer detected, it can be calculated that approximately 100 cases of cancer are detected by screening per case of radiation-induced cancer. Additionally, results of a study of LDCT screening in the population of smokers aged 55–74 years showed a reduction in mortality from lung cancer by 20% [26]. All these data indicate that the LDCT method is safe and effective for multiple repetitions within screening or monitoring the dynamics of the patient’s condition in the hospital despite the possible risks associated with radiation exposure. There is no doubt about the importance of using LDCT to reduce radiation exposure and ensure greater safety of the study for the patient.
CONCLUSION
Comparative analysis of the efficacy and diagnostic value of LDCT and CT performed according to a standard protocol revealed that LDCT is not only a full-fledged alternative, but also a preferable option, since its implementation can significantly reduce the radiation exposure of the patient. Given that during inpatient COVID-19 treatment, patient undergoes several imaging studies, the issue of radiation safety becomes urgent. According to practicing doctors, the amount of information provided by LDCT is not inferior to the standard CT technique in quality and accuracy; therefore, for dynamic studies, it is advisable to prefer LDCT, which is a method that enables the radiation exposure reduction.
ADDITIONAL INFORMATION
Competing interests. The authors declare that they have no competing interests.
Funding source. This study was not supported by any external sources of funding.
Authors’ contribution. D.A. Filatova ― search for publications on the article topic, writing the text of the manuscript; V.E. Sinitsin ― the concept of research, expert evaluation of information, editing the text of the manuscript, final version approval; E.A. Mershina ― formation of a data set, expert evaluation of information, editing of the text of the manuscript, final version approval. All authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published and agree to be accountable for all aspects of the work.
About the authors
Daria A. Filatova
Lomonosov Moscow State University
Author for correspondence.
Email: dariafilatova.msu@mail.ru
ORCID iD: 0000-0002-0894-1994
SPIN-code: 2665-5973
Medical Research and Educational Center
Russian Federation, 1a Shkolnaya street, 143430 Nakhabino, Moscow regionValentin E. Sinitsin
Lomonosov Moscow State University
Email: vsini@mail.ru
ORCID iD: 0000-0002-5649-2193
SPIN-code: 8449-6590
MD, PhD, Professor, Medical Research and Educational Center
Russian Federation, MoscowElena A. Mershina
Lomonosov Moscow State University
Email: elena_mershina@mail.ru
ORCID iD: 0000-0002-1266-4926
SPIN-code: 6897-9641
MD, PhD, Associate Professor, Medical Research and Educational Center
Russian Federation, MoscowReferences
- Ministry of Health of the Russian Federation. Temporary guidelines: prevention, diagnosis and treatment of new coronavirus infection. Version 8 (03.09.2020). Moscow; 2020. (In Russ). Available from: https://base.garant.ru/74596434/
- Romanov BK. Coronavirus infection COVID-19. Safety and Risc of Farmacotherapy. 2020;8(1):3–8. (In Russ.)
- Morozov SP, Protsenko DN, Smetanina SV, et al. Radiation diagnostics of coronavirus disease (COVID-19): organization, methodology, interpretation of results: preprint No. CDT-Version 2 of 17.04.2020. Moscow; 2020. 78 р. (In Russ.)
- Udugama B, Kadhiresan P, Kozlowski HN, et al. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020;14(4):3822–3835. doi: 10.1021/acsnano.0c02624
- Zhao W, Zhong Z, Xie X, et al. Relation between chest ct findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214(5):1072–1077. doi: 10.2214/AJR.20.22976
- Beregi JP, Greffier J. Low and ultra-low dose radiation in CT: Opportunities and limitations. Diagn Interv Imaging. 2019;100(2):63–64. doi: 10.1016/j.diii.2019.01.007
- Cheng L, Chen Y, Fang T, et al. Fast iterative adaptive reconstruction in low-dose CT imaging. In: 2006 International Conference on Image Processing. Atlanta, GA: IEEE; 2006. P. 889–892. Available from: https://ieeexplore.ieee.org/document/4106673/
- Hara AK, Paden RG, Silva AC, et al. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol. 2009;193(3):764–771. doi: 10.2214/AJR.09.2397
- Prakash P, Kalra M, Kambadakone A, et al. Reducing abdominal CT radiation dose with adaptive statistical iterative reconstruction technique. Invest Radiol. 2010;45(4):202–210. doi: 10.1097/RLI.ob013e3181dzfeec
- Chen LG, Wu PA, Sheu MH, et al. Automatic current selection with iterative reconstruction reduces effective dose to less than 1 mSv in low-dose chest computed tomography in persons with normal BMI. Medicine (Baltimore). 2019;98(28):e16350. doi: 10.1097/MD.0000000000016350
- Dangis A, Gieraerts C, De Brueker Y, et al. Accuracy and reproducibility of low-dose submillisievert chest CT for the diagnosis of COVID-19. Radiology Cardiothoracic Imaging. 2020;2(2):e200196. doi: 10.1148/ryct.2020200196
- Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020;323(22):2249–2251. doi: 10.1001/jama.2020.8259
- Long C, Xu H, Shen Q, et al. Diagnosis of the Coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961
- Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296(2):E115–E117. doi: 10/1148/radiol.2020200432
- Yang Y, Yang M, Shen C, et al. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. 2020. doi: 10.1101/2020.02.11.20021493
- Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149
- Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res. 2000;154(2):178–186. doi: 10.1667/0033-7587(2000)154[0178:rrcral]2.0.co;2
- Matkevich E, Sinitsyn V, Mershina E. Comparative analysis of radiation doses of patients with computed tomography in a Federal medical institution. Journal of Radiology and Nuclear Medicine. 2016;97(1):33–39. (In Russ). doi: 10.20862/0042-4676-2016-97-1-33-40
- Naidich DP, Marshall CH, Gribbin C, et al. Low-dose CT of the lungs: preliminary observations. Radiology. 1990;175(3):729–731. doi: 10.1148/radiology.175.3.2343122
- Prasad SR, Wittram C, Shepard JA, et al. Standard-dose and 50%-reduced-dose chest CT: comparing the effect on image quality. AJR Am J Roentgenol. 2002;179(2):461–465. doi: 10.2214/ajr.179.2.1790461
- Zwirewich CV, Mayo JR, Müller NL. Low-dose high-resolution CT of lung parenchyma. Radiology. 1991;180(2):413–417. doi: 10.1148/radiology.180.2.2068303
- Zhu X, Yu J, Huang Z. Low-dose chest CT: optimizing radiation protection for patients. AJR Am J Roentgenol. 2004;183(3):809–816. doi: 10.2214/ajr.183.3.1830809
- Kubo T, Ohno Y, Takenaka D, et al. Standard-dose vs. low-dose CT protocols in the evaluation of localized lung lesions: Capability for lesion characterization – iLEAD study. Eur J Radiol Open. 2016;3:67–73. doi: 10.1016/j.ejro.2016.03.002
- Gombolevsky VA, Chernina VY, Blokhin IA. Main achievements of low-dose computed tomography in lung cancer screening. Tuberculosis and Lung Diseases. 2021;99(1):61–70. (In Russ). doi: 10.21292/2075-1230-2021-99-1-61-7025.
- Rampinelli C, De Marco P, Origgi D, et al. Exposure to low dose computed tomography for lung cancer screening and risk of cancer: secondary analysis of trial data and risk-benefit analysis. BMJ. 2017;356:j347. doi: 10.1136/bmj.j347
- Chiles C. Lung cancer screening with low dose CT. Radiol Clin North Am. 2014;52(1):27–46. doi: 10.1016/j.rcl.2013.08.006.
Supplementary files