Abstract
Purpose
This study aims to identify the contributions of individual and community social determinants of health (SDOH), demographic, and clinical factors in COVID-19 disease severity through a model-based analysis.
Methods
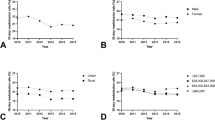
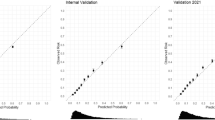
This national cross-sectional study focused on hospitalization among those tested for COVID-19 and use of intensive care, analyzing data on 220,848 Veterans tested between February 20, 2020 and October 20, 2021. Multiple logistic regression models were constructed using backwards elimination. The predictive value of each model was assessed with a c-statistic.
Results
Those hospitalized were older, more likely to be male, of Black or Asian race, have an income less than $39,999, live in an urban residence, and have medical comorbidities. The strongest predictors for hospitalization included Gini inequality index, race, income, heart failure, chronic kidney disease (CKD), and chronic obstructive pulmonary disease (COPD). For intensive care, Asian race, rural residence, COPD, and CKD were the strongest predictors. C-statistics were c = 0.749 for hospitalization and c = 0.582 for ICU admission.
Conclusions
A combination of clinical, demographic, individual and community SDOH factors predict COVID-19 hospitalization with good predictive ability and can inform risk stratification, discharge planning, and public health interventions. Racial disparities were not explained by social or clinical factors. Intensive care models had low discriminative power and may be better explained by other characteristics.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data Availability
The United States Department of Veterans Affairs (VA) places legal restrictions on access to veteran’s health care data. The data that support the findings for this study are not permitted to leave the VA firewall without a Data Use Agreement. VA data are made freely available to researchers behind the VA firewall with an approved VA study protocol. For more information, please visit https://www.virec.research.va.gov.
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- CDW:
-
Corporate Data Warehouse
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus disease 2019
- FPL:
-
Federal poverty level
- HIV:
-
Human immunodeficiency virus
- ICD-10:
-
International Classification of Diseases-10
- ICU:
-
Intensive care unit
- Sars-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SDOH:
-
Social Determinants of Health
- VHA:
-
Veterans Health Administration
- VA:
-
Veterans Affairs
- VINCI:
-
VA Informatics and Computing Infrastructure
- US:
-
United States
- USVETS:
-
United States Veterans Eligibility Trends and Statistics
References
CDC Covid Data tracker. Accessed February 4, 2023, from Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
COVID-19 Risks and Vaccine Information for Older Adults. Accessed January 24, 2022, from Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/aging/covid19/covid19-older-adults.html.
Griffith DM, Sharma G, Holliday CS, Enyia OK, Valliere M, Semlow AR, et al. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev Chronic Dis. 2020;17:e63. https://doi.org/10.5888/pcd17.200247.
Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021;4(6):e2111182. https://doi.org/10.1001/jamanetworkopen.2021.11182.
Evidence for Conditions that Increase Risk of Severe Illness. Accessed January 24, 2022, from Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/underlying-evidence-table.html.
Callender LA, Curran M, Bates SM, Mairesse M, Weigandt J, Betts CJ. The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front Immunol. 2020;11. https://doi.org/10.3389/fimmu.2020.01991.
Covid-19 Racial and Ethnic Health Disparities. Accessed January 24, 2022, from Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html.
Sze S, Pan D, Nevill CR, Gray LJ, Martin CA, Nazareth J, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. https://doi.org/10.1016/j.eclinm.2020.100630.
Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT Jr, Skanderson M, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17(9):e1003379. https://doi.org/10.1371/journal.pmed.1003379.
Raine S, Liu A, Mintz J, Wahood W, Huntley K, Haffizulla F. Racial and ethnic disparities in COVID-19 outcomes: social determination of health. Int J Environ Res Public Health. 2020;17(21):8115. Retrieved from https://www.mdpi.com/1660-4601/17/21/8115. Accessed 24 Jan 2022.
Chang MH, Moonesinghe R, Truman BI. COVID-19 hospitalization by race and ethnicity: association with chronic conditions among medicare beneficiaries, January 1-September 30, 2020. J Racial Ethn Health Disparities. 2021. https://doi.org/10.1007/s40615-020-00960-y.
Hsu HE, Ashe EM, Silverstein M, Hofman M, Lange SJ, Razzaghi H, et al. Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an Urban Safety-Net Medical Center - Boston, Massachusetts, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):864–9. https://doi.org/10.15585/mmwr.mm6927a3.
Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–43. https://doi.org/10.1056/NEJMsa2011686.
Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–62. https://doi.org/10.1377/hlthaff.2020.00598.
Lassale C, Gaye B, Hamer M, Gale CR, Batty GD. Ethnic disparities in hospitalisation for COVID-19 in England: the role of socioeconomic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav Immunol. 2020;88:44–9. https://doi.org/10.1016/j.bbi.2020.05.074.
Acosta AM, Garg S, Pham H, Whitaker M, Anglin O, O’Halloran A, et al. Racial and ethnic disparities in rates of COVID-19-associated hospitalization, intensive care unit admission, and in-hospital death in the United States From March 2020 to February 2021. JAMA Netw Open. 2021;4(10):e2130479. https://doi.org/10.1001/jamanetworkopen.2021.30479.
Ioannou GN, Locke E, Green P, Berry K, O’Hare AM, Shah JA, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-CoV-2 infection. JAMA Network Open. 2020;3(9):2022310-e2022310. https://doi.org/10.1001/jamanetworkopen.2020.22310.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6. https://doi.org/10.1038/s41586-020-2521-4.
Aldridge RW, Lewer D, Katikireddi SV, Mathur R, Pathak N, Burns R, et al. Black, Asian and Minority Ethnic groups in England are at increased risk of death from COVID-19: indirect standardisation of NHS mortality data. Wellcome Open Res. 2020;5:88. https://doi.org/10.12688/wellcomeopenres.15922.2.
Khanijahani A, Iezadi S, Gholipour K, Azami-Aghdash S, Naghibi D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20(1):248. https://doi.org/10.1186/s12939-021-01582-4.
About VHA. Accessed January 31, 2022, from US Department of Veterans Affairs. 2022. https://www.va.gov/health/aboutvha.asp#:~:text=The%20Veterans%20Health%20Administration%20(VHA,Veterans%20enrolled%20in%20the%20VA.
Razjouyan J, Helmer DA, Li A, Naik AD, Amos CI, Bandi V, Sharafkhaneh A. Differences in COVID-19-related testing and healthcare utilization by race and ethnicity in the Veterans Health Administration. J Rac Ethn Health Disparities. 2021;1–8. https://doi.org/10.1007/s40615-021-00982-0.
Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT, Skanderson M et al. Covid-19 testing, hospital admission, and intensive care among 2,026,227 United States Veterans aged 54–75 years. medRxiv : the preprint server for health sciences. 2020. 2020.2004.2009.20059964. https://doi.org/10.1101/2020.04.09.20059964.
Luo J, Rosales M, Wei G, Stoddard GJ, Kwok AC, Jeyapalina S, Agarwal JP. Hospitalization, mechanical ventilation, and case-fatality outcomes in US veterans with COVID-19 disease between years 2020–2021. Ann Epidemiol. 2022;70:37–44. https://doi.org/10.1016/j.annepidem.2022.04.003.
NCHHSTP Social Determinants of Health. Accessed January 24, 2022, from Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/nchhstp/socialdeterminants/index.html.
Singu S, Acharya A, Challagundla K, Byrareddy SN. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front Public Health. 2020;8:406–406. https://doi.org/10.3389/fpubh.2020.00406.
Hawkins D. Social determinants of COVID-19 in Massachusetts, United States: an ecological study. J Prev Med Public Health Yebang Uihakhoechi. 2020;53(4):220–7. https://doi.org/10.3961/jpmph.20.256.
KC M, Oral E, Straif-Bourgeois S, Rung AL, Peters ES. The effect of area deprivation on COVID-19 risk in Louisiana. PLoS One. 2020;15(12):e0243028. https://doi.org/10.1371/journal.pone.0243028.
Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: us county versus zip code analyses. J Public Health Manag Pract. 2021;27(Suppl 1):COVID-19 and Public Health: Looking Back, Moving Forward, S43-s56. https://doi.org/10.1097/phh.0000000000001263.
Rural-Urban Commuting Area Codes. Accessed February 22, 2022 from Economic Research Service U.S. Department of Agriculture. 2020. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx.
Gini Index. United States Census Bureau. Accessed March 28, 2022 from United States Census Bureau. n.d. https://www.census.gov/topics/income-poverty/incomeinequality/about/metrics/gini-index.html.
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–70. https://doi.org/10.1053/jhep.2001.22172.
Caetano SJ, Sonpavde G, Pond GR. C-statistic: a brief explanation of its construction, interpretation and limitations. Eur J Cancer. 2018;90:130–2. https://doi.org/10.1016/j.ejca.2017.10.027.
Asch DA, Islam MN, Sheils NE, Chen Y, Doshi JA, Buresh J, et al. Patient and hospital factors associated with differences in mortality rates among Black and White US Medicare beneficiaries hospitalized with COVID-19 infection. JAMA Netw Open. 2021;4(6):e2112842. https://doi.org/10.1001/jamanetworkopen.2021.12842.
Eibner C, Krull H, Brown KM, Cefalu M, Mulcahy AW, Pollard M, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q. 2016;5(4):13.
Acknowledgements
This work was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health [award number UL1TR002378]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors contributed to the study conception and design.
Funding
This work was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health [award number UL1TR002378]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Alyssa Greenhouse, Daniel Richard, and Anjali Khakharia. Methodologic guidance was provided by Michael Goodman, Lawrence Phillips, and Julia Gazmararian. The first draft of the manuscript was written by Alyssa Greenhouse and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the institutional review boards of the Atlanta VA Research and Development Committee and Emory University. It was granted a waiver of informed consent and is Health Insurance Portability and Accountability Act compliant.
Competing Interests
The authors report no declarations of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Greenhouse, A.R., Richard, D., Khakharia, A. et al. The Social, Demographic, and Clinical Predictors of COVID-19 Severity: a Model-based Analysis of United States Veterans. J. Racial and Ethnic Health Disparities 11, 3172–3181 (2024). https://doi.org/10.1007/s40615-023-01773-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01773-5