Abstract
Natural products and herbal medicine have been widely used in drug discovery for treating infectious diseases. Recent outbreak of COVID-19 requires various therapeutic strategies. Here, we used YSK-A, a mixture of three herbal components Boswellia serrata, Commiphora myrrha, and propolis, to evaluate potential antiviral activity against SARS-CoV-2. We showed that YSK-A inhibited SARS-CoV-2 propagation with an IC50 values of 12.5 µg/ml and 15.42 µg/ml in Vero E6 and Calu-3 cells, respectively. Using transcriptome analysis, we further demonstrated that YSK-A modulated various host gene expressions in Calu-3 cells. Among these, we selected 9 antiviral- or immune-related host genes for further study. By siRNA-mediated knockdown experiment, we verified that MUC5AC, LIF, CEACAM1, and GDF15 host genes were involved in antiviral activity of YSK-A. Therefore, silencing of these genes nullified YSK-A-mediated inhibition of SARS-CoV-2 propagation. These data indicate that YSK-A displays an anti-SARS-CoV-2 activity by targeting multiple antiviral genes. Although the exact antiviral mechanism of each constituent has not been verified yet, our data indicate that YSK-A has an immunomodulatory effect on SARS-CoV-2 and thus it may represent a novel natural product-derived therapeutic agent for treating COVID-19.
Similar content being viewed by others
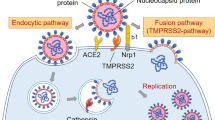
Natural products and herbal extracts have been used as traditional and complementary medicine, especially in Asian countries, including India, China, Japan, and Korea as well as in several African countries1. Since herbal medicine has an immunomodulatory effect, it could be used as a preventive measure and as a therapeutic agent for coronavirus disease 2019 (COVID-19) patients. Furthermore, natural products are less toxic, inexpensive, and easily accessible sources of phytochemicals for therapeutic agents. Therefore, complementary and substitute treatments using plant-based phytochemicals could be an alternative strategy for controlling severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic2. Indeed, National Health Commission of China has delivered therapy regulations for the use of herbal medicine as an alternative remedy for COVID-19 in combination with modern western medicine3. Accumulating evidence suggests that natural products derived from plants exert inhibitory effects on SARS-CoV-2 propagation. Herbal drug extracts from Polygala Root, Areca, and Quercus Bark and natural compounds derived from herbal drugs such as baicalin and glabridin display antiviral activity against SARS-CoV-2 infection4. In addition, PHELA, an herbal combination of four exotic African medicinal plants (Clerodendrum glabrum E. Mey. Lamiaceae, Gladiolus dalenii van Geel, Rotheca myricoides (Hochst.) Steane & Mabb, and Senna occidentalis (L.) Link), effectively inhibits both SARS-CoV and SARS-CoV-2 infections5.
The SARS-CoV-2 pandemic, a global outbreak of coronavirus, has had a devastating impact on the global economy and health of people across the world. To date, this virus has infected more than 770 million people worldwide and caused nearly 7 million deaths6. SARS-CoV-2 not only devastates the respiratory tract system7 but also affects other organs, and consequently leads to multiple organ failure and death8,9. Therefore, tremendous research efforts have been made to develop prevention and treatment strategies against SARS-CoV-2. So far, a few antiviral drugs (paxlovid, remdesivir, and molnupiravir) and more than 10 monoclonal antibodies have been marketed for COVID-19 treatment. However, the treatment window of antiviral agents is probably limited to the viral phase of SARS-CoV-2 infection. Apart from a few oral antivirals, current marketed antiviral agents are delivered by injection, further limiting practical administration in resource-limited settings lacking developed healthcare infrastructure10.
Natural products have been considered as sources of new anti-SARS-CoV-2 drugs. YSK-A is a mixture of three different herbal extracts consisting of Boswelliaserrata, Commiphoramyrrha, and propolis. Recently, we have reported that YSK-A exerts an antiviral activity by reducing lesions of respiratory tracts in SARS-CoV-2 infected hamsters11. To further investigate how YSK-A displays an anti-SARS-CoV-2 activity, we performed RNASeq analysis using Calu-3 cells and identified four host genes mainly involved in antiviral and immune responses. Importantly, we showed that YSK-A inhibited SARS-CoV-2 propagation by targeting MUC5AC, LIF, CEACAM1, and GDF15 genes. All these data suggest that YSK-A may represent a potential alternative natural product-derived antiviral agent against SARS-CoV-2. This is an important finding that natural products and herbal extracts could be utilized as resources for novel antiviral agents against SARS-CoV-2.
Results
YSK-A inhibits SARS-CoV-2 propagation
We have recently reported that YSK-A displayed potential antiviral activity against SARS-CoV-211. To further evaluate whether YSK-A exerted anti-SARS-CoV-2 activity, we first evaluated cellular toxicity of YSK-A in Vero E6 and Calu-3 cells, which were known to be highly susceptible to SARS-CoV-2 infection12. We showed that as high as 100 µg/ml YSK-A displayed no cytotoxic effect on both cell lines (Fig. 1A). To determine whether YSK-A inhibits SARS-CoV-2 replication, Vero E6 cells were either mock infected or infected with either wild-type (MOI = 0.01) or Delta variant (MOI = 0.1) of SARS-CoV-2 and treated with either vehicle or 100 µg/ml YSK-A for 24 h and then SARS-CoV-2 replication was determined by staining cells with double-stranded RNA-specific J2 antibody. By using immunofluorescence assay, YSK-A profoundly decreased SARS-CoV-2 RNA in both wild-type and Delta variant (Fig. 1B). These data verified that YSK-A had anti-SARS-CoV-2 activity. To further confirm the anti-SARS-CoV-2 activity of YSK-A, either Vero E6 or Calu-3 cells were pretreated with various concentrations of YSK-A for 24 h and then infected with wild-type (MOI = 0.01 in Vero E6; MOI = 0.1 in Calu-3) or Delta variant (MOI = 0.1 in Vero E6; MOI = 1 in Calu-3) of SARS-CoV-2. At 24 h postinfection (Vero E6 cells) or 48 h postinfection (Calu-3 cells), supernatant was collected to determine the infectious virus titer by TCID50 assay. Simultaneously, RNA and protein levels of SARS-CoV-2 were analyzed either by quantitative real-time PCR (qRT-PCR) or immunoblot analysis. YSK-A significantly decreased infectious titer (Fig. 1C) and RNA levels (Fig. 1D) of SARS-CoV-2. We further showed that YSK-A markedly decreased protein levels of SARS-CoV-2 in a dose-dependent manner (Fig. 1E). Since remdesivir targets viral RNA-dependent RNA polymerase and widely used in SARS-CoV-2 research, we used remdesivir as a positive control. We demonstrated that 5 μM remdesivir completely abolished SARS-CoV-2 protein levels. Interestingly, we observed multiple bands of nucleoprotein (N) in Vero E6 cells. It has been previously reported that N of SARS-CoV undergoes posttranslational modifications13. The authors found both full-length N and additional bands, indicating the N-specific proteolytical cleavage with the help of Caspase-6. They further demonstrate that caspase-6-mediated cleavage of N depends on the cell lines and correlates with the replication cycle of SARS-CoV. N processing is only observed in Vero E6 and A549 cells but not in Caco-2 and N2a cells. We therefore postulate that SARS-CoV-2 N protein may also undergo similar posttranslational modifications. In fact, we previously observed multiple bands of N protein in Vero E6 cells14. Of note, YSK-A efficiently blocked virus titer with an IC50 value of 12.5 µg/ml in Vero E6 and 15.42 µg/ml in Calu-3 for wild-type, and IC50 value of 7.07 µg/ml in Vero E6 and 54.35 µg/ml in Calu-3 for Delta variant of SARS-CoV-2. Collectively, YSK-A displayed broad-spectrum antiviral activity, suggesting that it may represent a novel plant-derived therapeutic agent for COVID-19.
YSK-A impedes SARS-CoV-2 propagation. (A) Either Vero E6 or Calu-3 cells were treated with 12.5, 25, 50, 100 μg/ml of YSK-A. At 24 h (Vero E6) or 48 h (Calu-3) after treatment, cell viability was measured by WST assay as described in Material and Method. (B) Vero E6 cells were either mock-infected or infected with wild-type (MOI = 0.01) or Delta variant (MOI = 0.1) of SARS-CoV-2 for 1 h in the absence or presence of 100 μg/ml YSK-A. Cells were further cultured in media containing YSK-A. At 24 h postinfection, cells were fixed in 4% paraformaldehyde, and immunofluorescence staining was performed by using J2 antibody and FITC-conjugated goat anti-mouse IgG to detect double-stranded RNA (green). Cells were counterstained with DAPI to label nuclei (blue). Scale bar = 50 µm. (C–E) Cells were pretreated with 12.5, 25, 50, 100 μg/ml of YSK-A. At 24 h after treatment, cells were infected with wild-type (MOI = 0.01 in Vero E6; MOI = 0.1 in Calu-3) or Delta variant (MOI = 0.1 in Vero E6; MOI = 1 in Calu-3) of SARS-CoV-2 for 1 h in the absence or presence of the indicated concentrations of YSK-A. Cells were further cultured in media containing YSK-A and then harvested at 24 h postinfection for Vero E6 (C–E, left panels) and 48 h postinfection for Calu-3 (C–E, right panels). (C) Supernatant was collected to determine the infectious virus titer by TCID50 assay. For the “% inhibition” calculation, the normalized relative inhibition values were calculated according to the formula % inhibition = 100 x [1—(X—mock infected) / (infected untreated—mock infected)], where X is each given treatment condition. Dose–response curves for IC50 values were determined by nonlinear regression analysis using the GraphPad Prism v9 (GraphPad Software, San Diego, CA, USA). (D) SARS-CoV-2 RNA levels were determined by qRT-PCR. One-way ANOVA was used for comparing multiple YSK-A concentrations treatment with virus infection only. (E) Protein levels of SARS-CoV-2 were determined by an immunoblot assay using the indicated antibodies. Remdesivir (Rem) was used as a positive control. Data represent averages from triplicate experiments. *P < 0.05.
YSK-A displays antiviral activity by regulating various host gene expressions
To investigate the antiviral mechanism of YSK-A, we performed transcriptome sequencing (RNA-Seq) analysis using Calu-3 cells treated with 100 µg/ml YSK-A as we reported previously15. We identified ~ 100 host genes that were differentially expressed in YSK-A-treated cells. Of these, 39 genes were down-regulated with 1.5-fold reduction (Log2FC < -0.5) (Table 1A) and 65 genes were up-regulated with 1.5-fold increase (Log2FC > 0.5) in YSK-A treated cells (Table 1B). Of these differentially regulated host genes, we randomly selected 28 genes which are known to be involved in either antiviral activity or immune response. To further verify whether these selected genes were involved in YSK-A-mediated antiviral activity, Calu-3 cells were treated with increasing amounts of YSK-A. At 24 h posttreatment, RNA was isolated and then mRNA levels of these genes were measured by qRT-PCR. Figure 2A shows that mRNA levels of 8 genes were decreased by YSK-A in a dose dependent manner. Of note, YSK-A significantly decreased mRNA levels of CCN1, CCN2, DKK1, GPRC5B, ITGB6 and VIM with nearly twofold, which is consistent with transcriptomic data. Conversely, we further demonstrated that mRNA levels of 20 genes were increased by YSK-A in a dose dependent manner (Fig. 2B). The mRNA levels of 19 genes were similarly increased by YSK-A as seen in transcriptome data. However, the mRNA level of HMSD was increased only 1.5-fold as compared to sevenfold in transcriptomic analysis. This difference may be due to either the low copy number of HMSD in Calu-3 cells or the sensitivity level between these two methods. After literature search about these genes, we finally selected 1 down-regulated gene (VIM) and 8 up-regulated genes (MUC5AC, ISG20, LIF, OAS1, TIPARP, CEACAM1, CXCL2 and GDF15) to further investigate the potential roles of these in SARS-CoV-2 propagation.
YSK-A modulates mRNA levels of numerous host genes. (A) Calu-3 cells were either mock treated or treated with 0, 25, 50, 100 μg/ml YSK-A. At 24 h after treatment, total cellular RNA was isolated and then cDNA was synthesized. mRNA levels of 8 host genes down-regulated by YSK-A were measured by qRT-PCR. (B) Calu-3 cells were treated as described in A and then mRNA levels of 20 host genes up-regulated by YSK-A were measured by qRT-PCR. Data represent averages from triplicate experiments. One-way ANOVA was used for comparing multiple YSK-A concentrations treatment with DMSO treatment (*P < 0.05; **P < 0.01).
YSK-A modulates mRNA levels of target genes at different time points
To determine an optimum condition for treating cells with YSK-A, Calu-3 cells were treated with 100 µg/ml YSK-A. At the indicated time points after YSK-A treatment, RNA was extracted and then mRNA levels were analyzed by qRT-PCR. As shown in Fig. 3A, YSK-A significantly decreased mRNA level of VIM in Calu-3 cells at 12 h after treatment as compared with vehicle. Conversely, YSK-A significantly increased mRNA levels of other eight remaining genes (Fig. 3B). Interestingly, modulatory effects of YSK-A on target gene expressions varied at different time points. Therefore, mRNA levels were significantly upregulated at 12 h posttreatment in MUC5AC and OAS1, whereas at 3 h posttreatment in ISG20 and TIPARP. We further showed that YSK-A upregulated mRNA levels of LIF, CEACAM1, CXCL2, and GDF15 at 24 h posttreatment. For unknown reason, CXCL2 mRNA level in mock-treated cells was markedly decreased at 24 h posttreatment. Of note, modulatory effects of YSK-A on target genes were particularly significant at 24 h after treatment.
YSK-A regulates mRNA levels of target genes at various time points. (A) Calu-3 cells were either mock treated or treated with 100 µg/ml YSK-A. At the indicated time points, total cellular RNA was isolated and then cDNA was synthesized. mRNA level of VIM gene was measured by qRT-PCR. (B) Calu-3 cells were treated as described in A and then mRNA levels of 8 host genes were measured by qRT-PCR. Data represent averages from triplicate experiments. Student’s t test was used for comparing the differences between YSK-A treatments and mock-treatment at the indicated time points (*P < 0.05; **P < 0.01). One-way ANOVA was calculated to compare the differences between the indicated time points and mock-treatment at 3 h (#P < 0.05, ##P < 0.01).
Confirmation of the host target genes of YSK-A by siRNA-mediated silencing
To further analyze the modulatory effect of YSK-A on selected host genes, Calu-3 cells were transfected with either negative siRNA or siRNA targeting each of 9 selected genes, followed by treatment with 100 µg/ml YSK-A. At 24 h after treatment, mRNA expression levels of YSK-A target genes were analyzed. As shown in Fig. 4, siRNA-mediated knockdown impaired mRNA expressions of all target genes. We further showed that YSK-A decreased mRNA levels of VIM nearly twofold (Fig. 4A), whereas YSK-A increased twofold in mRNA levels of MUC5AC, ISG20, LIF, OAS1, TIPARP, CEACAM1, CXCL2, and GDF15 (Fig. 4B). Therefore, modulatory role of YSK-A on mRNA expressions and knockdown efficiency of siRNAs were highly effective on target genes. Collectively, these data verified that siRNAs targeting nine genes properly decreased mRNA levels and these genes proved to be the real target of YSK-A.
Confirmation of YSK-A target genes by siRNA-mediated silencing. (A) Calu-3 cells were transfected with either 20 nM negative siRNA or 20 nM VIM-specific siRNA. At 24 h after siRNA treatment, cells were treated with either DMSO or 100 µg/ml YSK-A. At 24 h after treatment, Calu-3 cells were harvested, RNA was extracted, and then mRNA expression level of VIM was determined by qRT-PCR. (B) Calu-3 cells were transfected with either 20 nM negative siRNA or 20 nM siRNAs targeting genes, including MUC5AC, ISG20, LIF, OAS1, TIPARP, CEACAM1, CXCL2 and GDF15. Cells were further treated as described in A, and then mRNA expression levels of 8 genes were determined by qRT-PCR. Data represent averages from triplicate experiments. One-way ANOVA was calculated to compare the difference between gene-specific siRNA and negative siRNA in the presence or absence of YSK-A. *P < 0.05; **P < 0.01, ***P < 0.001; ns, not significant; #P < 0.05; ##P < 0.01; ns not significant.
YSK-A displays anti-SARS-CoV-2 activity by targeting multiple host genes
Lastly, we interrogated whether YSK-A target genes are involved in SARS-CoV-2 propagation. For this purpose, Calu-3 cells were transfected with either negative siRNA or siRNA targeting the indicated host target genes. At 24 h after siRNA transfection, cells were further treated with either vehicle (DMSO) or 100 µg/ml YSK-A. One day after treatment, cells were infected with SARS-CoV-2 (MOI = 0.2) for 1 h in the absence or presence of YSK-A. At 48 h postinfection, SARS-CoV-2 propagation was analyzed by TCID50, qRT-PCR, and immunoblot analysis. As expected, YSK-A decreased virus titer, RNA, and nucleoprotein levels of SARS-CoV-2 as compared to DMSO treated cells. Since YSK-A downregulated the expression of VIM gene and VIM is considered to be a coreceptor of SARS-CoV-216,17, we expected that knockdown of VIM might decrease SARS-CoV-2 propagation. However, silencing of VIM increased virus titer, RNA and protein levels of SARS-CoV-2 as compared to negative siRNA-treated cells (Fig. 5 A). These data suggest that VIM may not be involved in SARS-CoV-2 propagation. We next evaluated antiviral activities of the remaining 8 genes that were upregulated by YSK-A. We expected that if these gene expressions were impaired, YSK-A might no longer suppress the propagation of SARS-CoV-2. Indeed, YSK-A was unable to impede SARS-CoV-2 propagation in MUC5AC-, LIF-, CEACAM1- and GDF15-knockdown cells (Fig. 5B,C). Instead, knockdown of these four genes significantly increased viral propagation as compared to virus infection only. These data indicate that MUC5AC, LIF, CEACAM1, and GDF15 have intrinsic anti-SARS-CoV-2 activity and thus we propose that YSK-A may upregulate these four multiple genes to inhibit SARS-CoV-2 propagation. On the other hand, YSK-A marginally increased SARS-CoV-2 propagation in ISG20, OAS1, CXCL2 silencing cells. These data indicate that ISG20, OAS1, CXCL2 may not be involved in YSK-A-mediated SARS-CoV-2 antiviral activity. Of note, knockdown of TIPARP completely inhibited SARS-CoV-2 propagation in the presence of YSK-A, further suggesting that TIPRAP might not be involved in YSK-A-mediated SARS-CoV-2 regulation. Taken together, these data indicate that YSK-A inhibits SARS-CoV-2 propagation by upregulating antiviral- and immune-related multiple host target genes, including MUC5AC, LIF, CEACAM1, and GDF15.
YSK-A displays anti-SARS-CoV-2 activity by targeting various host genes. (A) (Left panel) Calu-3 cells were transfected with either 20 nM negative siRNA or 20 nM VIM-specific siRNA. At 24 h after siRNA treatment, cells were treated with either DMSO or 100 µg/ml YSK-A. At 24 h after treatment, cells were either mock-infected or infected with wild-type SARS-CoV-2 (MOI = 0.2) in the absence or presence of 100 µg/ml YSK-A for 1 h. The cells were then washed with PBS and the culture medium was replaced with fresh medium containing either vehicle or 100 µg/ml YSK-A. At 48 h postinfection, TCID50 value was determined from the SARS-CoV-2-containing supernatant. (Middle panel) Total cellular RNA was extracted from the virus infected cells and then SARS-CoV-2 RNA levels were measured by qRT-PCR. (Right panel) Viral protein expression levels were determined by immunoblot assay using the indicated antibodies. (B) (Top panel) Calu-3 cells were transfected with either 20 nM negative siRNA or 20 nM siRNA targeting MUC5AC, ISG20, LIF, OAS1, and TIPARP, respectively. Cells were treated with YSK-A and further infected with SARS-CoV-2 as described in A. At 48 h postinfection, TCID50 value was determined from the SARS-CoV-2-containing supernatant. (Middle panel) Total cellular RNA was extracted from the virus infected cells and then SARS-CoV-2 RNA levels were measured by qRT-PCR. (Bottom panel) Viral protein expression levels were determined by immunoblot assay using the indicated antibodies. (C) (Top panel) Calu-3 cells were transfected with either 20 nM negative siRNA or 20 nM siRNA targeting CEACAM1, CXCL2, and GDF15, respectively. Cells were treated with YSK-A and further infected with SARS-CoV-2 as described in A. At 48 h postinfection, TCID50 value was determined from the SARS-CoV-2-containing supernatant. (Middle panel) Total cellular RNA was extracted from the virus infected cells and then SARS-CoV-2 RNA levels were measured by qRT-PCR. (Bottom panel) Viral protein expression levels were determined by immunoblot assay using the indicated antibodies. Data represent averages from triplicate experiments. Student’s t test was used for comparing the significant difference between gene-specific siRNA and negative siRNA in the presence of YSK-A (#P < 0.05). One-way ANOVA was calculated to compare the multiple treatments gene-specific siRNA and negative siRNA (*P < 0.05; **P < 0.01, ***P < 0.001).
Discussion
Natural products and herbal medicine have been widely used to treat human diseases and disorders. We previously reported that Mori Cortex Radicis18, Triterpenoid saponins19, and saponin20 inhibit HCV propagation. It has been also reported that various natural products and their derivatives display antiviral activity against SARS-CoV-24,5,21. We previously show that YSK-A exerts antiviral activity in SARS-CoV-2 infected cells11. In the current study, we showed that YSK-A displayed no cytotoxic effect on Vero E6 and Calu-3 cells. To further investigate how YSK-A displays an anti-SARS-CoV-2 activity, we performed RNASeq analysis and identified four host genes which have proved to be involved in antiviral and immune responses in YSK-A-treated Calu-3 cells. We demonstrated that YSK-A-regulated four host genes, including MUC5AC, LIF, CEACAM1 and GDF15, exhibited the antiviral activity against various variants of concern of SARS-CoV-2 in two different cell lines.
Boswellia serrata is known to have substantial anti-inflammatory activities22,23,24 and has been used to treat many inflammatory diseases such as rheumatoid arthritis25, ulcerative colitis26 and chronic colitis27. Commiphora myrrha has been demonstrated to have anti-inflammatory28 and analgesic activity28,29. It also has anti-microbia30 and anti-infective activity against acute respiratory viral infections31. In silico studies further suggest that Boswellia serrata ligands and a Commiphora myrrha product (Tiryaq-E-Wabai) may interact with viral proteins to interrupt SARS-CoV-2 propagation32,33,34. Propolis has been well known to have anti-microbial35, anti-inflammatory and immunomodulatory activities36,37 and it shows broad-spectrum antiviral activity against a diverse panel of viruses38. It has been previously reported that propolis exerts an antiviral effect on COVID-1939,40. In our previous study, Commiphora myrrha and propolis also displayed antiviral activity against SARS-CoV-2 in Vero E6 cells11.
To further investigate whether any of these host genes were involved in YSK-A-mediated antiviral activity, we performed RNA-Seq analysis in Calu-3 cells. We identified that ~ 100 host genes were differentially expressed in YSK-A-treated cells as compared with mock-infected cells (Table. 1). Of these, we selected 28 antiviral and immune-related genes, and investigated the effect of YSK-A on mRNA replication of target genes. Among these, we finally selected 1 down-regulated gene (VIM) and 8 up-regulated genes (MUC5AC, ISG20, LIF, OAS1, TIPARP, CEACAM1, CXCL2, GDF15) for further study. We showed that the modulatory effect of YSK-A on host genes has reached the maximum at 24 h after treatment. Based on this finding, we further analyzed antiviral activity of SARS-CoV-2 of MUC5AC, LIF, TIPARP, CEACAM1 and GDF15. Mucin 5AC (MUC-5AC) is a large gel-forming glycoprotein that forms a major airway mucin41. Recent study shows that SARS-CoV-2 spike induces MUC5AC/5B in human nasal epithelial cells42 and SARS-CoV-2 infection increases the MUC5AC secretion in primary human airway epithelial cells43. We showed that knockdown of MUC5AC nullified the inhibitory effect of YSK-A and thus enhanced SARS-CoV-2 infection. However, it has been previously reported that MUC5AC is riched in asthma44, and patients with asthma are vulnerable to get severe COVID-1945. Although mucus hyperproduction provides a physical barrier, IL-13 treated cells still maintain a low degree of infection despite the removal of mucus43. All these data suggest that MUC5AC acts as an antiviral factor and YSK-A regulates MUC5AC to inhibit SARS-CoV-2 propagation. Leukemia inhibitory factor (LIF) belongs to the IL-6 cytokine family. There is no direct evidence indicating that LIF exerts an anti-SARS-CoV-2 activity. It has been previously reported that LIF plays an important role in protecting lung from viral infection46,47. LIF is also required to maintain stable function of the blood-air barrier during infection48. In addition, our data showed that silencing of LIF increased SARS-CoV-2 propagation and thus LIF may be considered as an antiviral gene. The analysis of RNA-seq data from MERS-CoV infected Calu-3 cells detected the up-regulation of AHR and related genes including TCDD-inducible poly-ADP-ribose polymerase (TIPARP)49. TIPARP is a viral RNA-sensing pattern recognition receptor that mediates antiviral responses triggered by BAX- and BAK1-dependent mitochondrial damage50. However, TIPARP inhibits IFN production by ADP-ribosylation of TBK-1, leading to enhanced replication of several viruses51. In our study, YSK-A virtually abolished SARS-CoV-2 propagation in TIPARP-silenced cells. This result suggests that other mechanism may be involved in the YSK-A-regulated TIPARP function of the SARS-CoV-2 propagation. Carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1) is involved in IFN-γ-mediated induction of inflammatory responses, cellular growth, and proliferation in airway epithelial cells52. CEACAM1 expression level is the highest during SARS-CoV-2 infection, followed by SARS-CoV, IAV, and RSV53. Moreover, CEACAM1 suppresses both HCMV and influenza viruses in an SHP2-dependent process by suppressing mTOR-mediated protein biosynthesis54. Overall, CEACAM1 functions as an antiviral factor and YSK-A may exert an anti-SARS-CoV-2 activity by increasing CEACAM1 expression level. Growth and differentiation factor 15 (GDF15) belongs to the transforming growth factor β superfamily and is also named macrophage inhibitory cytokine-1. Overexpression of GDF15 inhibits H5N1 infection55. GDF15 is known to be a biomarker of cardiovascular and inflammatory COVID-19 patients in many clinical studies56. Overexpression of GDF15 in COVID-19 might be a compensatory mechanism to counteract dysregulated inflammatory reactions57. Here we postulate that YSK-A may display an antiviral activity by modulating GDF15 expression level in SARS-CoV-2 infection settings. However, overexpression of GDF15 increases the infectivity of HCV58. Since the role of GDF15 is still controversial in various viral infections, more studies are needed to elucidate the molecular mechanism of GDF15 in YSK-A-treated SARS-CoV-2 infection.
To further determine which host genes might be involved in YSK-A-mediated antiviral activity, we also selected interferon stimulated exonuclease gene 20 (ISG20), 2′,5′-oligoadenylate synthetase 1 (OAS1), and C-X-C motif chemokine ligand 2 (CXCL2) because these genes are known to have intrinsic antiviral activity. ISG20 has been shown to inhibit multiple viruses, including hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), Influenza A virus (IAV), and SARS-CoV-259,60,61,62,63. Thus, targeting ISG20 may be a potential therapeutic strategy for treating COVID-19. OAS1 is an interferon-stimulated gene that plays a key role in the cellular innate immune response. A recent study shows that OAS1 binds to dsRNA structures in the SARS-CoV-2 5′-UTR and blocks SARS-CoV-2 replication64. Using inducible CRISPR activation screen, OAS1 is identified as a SARS-CoV-2 restriction factor65 and decreased OAS1 expression contributes to COVID-19 severity66. CXCL2 is involved in inflammatory response. CXCL2 can clear SARS-CoV in mice depleted with CD4 + cells67. Although ISG20, OAS1 and CXCL2 have intrinsic antiviral activity, these genes are not involved in inhibitory activity of YSK-A in SARS-CoV-2 propagation. VIM, a type III intermediate filament protein, has been considered as coreceptors for various viruses68. It has been reported that VIM plays a crucial role in SARS-CoV infection69. VIM may bind to SARS-CoV-2 S protein and facilitate SARS-CoV-2 entry in human endothelial cells16,17. However, our study showed that silencing of VIM increased SARS-CoV-2 propagation. Further study is needed to determine whether VIM is involved in YSK-A-regulated SARS-CoV-2 propagation.
Collectively, we demonstrated that YSK-A inhibited SARS-CoV-2 propagation through multiple host genes which have widely been involved in antiviral activity and immune response. The mode of inhibitory action of YSK-A in SARS-CoV-2 propagation may be a complicated process because YSK-A consists of 3 different natural products which exhibit their own antiviral activity and immunomodulatory response. Nevertheless, using SARS-CoV-2-infected cells as a model system, we verified that YSK-A blocked viral propagation by modulating antiviral and immune-related host genes. Most importantly, we provided crucial evidence that natural products derived from plants could be an alternative therapeutic option for the treatment of COVID-19. In conclusion, YSK-A displays an anti-SARS-CoV-2 activity and thus potential of our findings are profound. However, further clinical studies are necessary to evaluate the efficacy of YSK-A as therapeutic agents for COVID-19.
Methods
Cell culture
Vero E6 cells derived from the kidney of an African green monkey and Calu-3 cells derived from human lung cancer were grown in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum, 1% penicillin–streptomycin, and 1% nonessential amino acids with 5% CO2 at 37 °C. Cells were used in experiments from 3 to 10 passages and viral infection was performed when the cell density was ~ 90%. Calu-3 cells were provided by Korean Cell Line Bank (Seoul, Korea) and Vero E6 cells were obtained from ATCC.
Preparation of infectious SARS-CoV-2
Wild-type Wuhan (NCCP-43331) and Delta (NCCP-43405) of SARS-CoV-2 were provided by the National Culture Collection for Pathogens, South Korea. Viruses were cultured in Vero E6 cells grown in DMEM supplemented with 2% FBS, 1% penicillin–streptomycin, and HEPES (Invitrogen, USA). Viral titers were determined by the 50% tissue culture infectious dose (TCID50) assay. All experiments were conducted in a biosafety level 3 (BSL-3) facility, the Korea Zoonosis Research Institute, Jeonbuk National University.
YSK-A preparation
A powder mixture (1:1:1) of Boswellia serrata, Commiphora myrrha, and propolis (designated as YSK-A) used in this study was provided by Yeskin (Korea). Boswellia serrata ethyl alcohol (EtOH) extract powder (UMALAXM ORGANICS Pvt. Ltd, June 2020) and propolis extract powder (AC biotech Pty. Ltd, October 2020) are commercially available products. Commiphora myrrha extract powder was obtained as follows. Commiphora myrrha (SAMIN pharma. INC., December 2021) was extracted with 50% EtOH at 90 °C for 8 h. The extract was concentrated and prepared as a freeze-dried powder. Standard compounds cinnamic acid, galangin, 11-keto-β boswellic acid (KBA), acetyl-11-keto-β-boswellic acid (AKBA), and furanoeudesma 1,3-diene were purchased from Coresciences. Then the YSK-A quantity was tested and the purity of all components were more than 95%11.
Water-soluble tetrazolium salt (WST) assay
Vero E6 or Calu-3 cells seeded on a 24-well plate were treated with various concentrations of YSK-A. At the indicated time points, cell viability was measured using 30 µl of WST (Dail Lab, Korea) as reported previously70.
TCID50 assay
A 50% tissue culture infectious dose (TCID50) assay was performed to determine the infectious titer of cell culture-produced SARS-CoV-2 as described previously71 with few modifications. Vero E6 cells seeded on 96-well plates overnight were infected with ten-fold serial dilutions of the virus-containing supernatants. At 5 days postinfection, virus-infected cells were counted by the presence of CPE in each well under a light microscope.
Transcriptome analysis
RNA purification
Calu-3 cells were treated with 100 µg/ml YSK-A. At 24 h post-treatment, cells were harvest and then total RNA was extracted using NucleoZol (Macherey–Nagel, Germany) according to the manufacturer's method.
RNA sequencing library construction
For the RNA sequencing assay, cDNA libraries were constructed, and single-end libraries were sequenced using the MGI-T7 platform (MGI Tech Co) using MGIEasy RNA Directional Library Prep Set.
Sequence alignment
We removed adapter sequence using Cutadapt version 2.9 and using the quality filtering of Trimmomatic version 0.39 which scans through reads from the 5’end and removes reads that length under 36 bases. After Trimming, reads were aligned to the human reference genome consisting of hg38 and Ensembl v.102 used STAR version 2.7.3a. RSEM version 1.3.1. was used in combination with STAR program. STAR and RSEM were set default parameters72,73,74,75.
Gene expression analysis
We normalized gene count data used DEseq2 normalized method into coding genes. We performed gene expression pattern to heatmap and PCA plot using R packages. Differential expression of gene analysis was performed using DEseq276.
Difference expression of genes
We used DESeq2 for DEG identification from RNA-seq data that normalized expect counts at fold change > 1.5. We then classified the gene expression into 2 groups: down-regulated group with 1.5-fold reduction (Log2FC < − 0.5) and up-regulated group with 1.5-fold increase (Log2FC > 0.5).
Quantification of RNA
Total RNA was isolated using NucleoZol (Macherey–Nagel, Germany). cDNA was synthesized by using a cDNA synthesis kit (Toyobo) according to the manufacturer’s instructions. Quantitative real-time PCR (qRT-PCR) experiments were performed using the CFX Connect real-time system (Bio-Rad Laboratories, Hercules, CA). Primer sequences to detect YSK-A-stimulated genes, β-actin and SARS-CoV-2 polymerase are listed in Table 2.
RNA interference
siRNAs targeting YSK-A-stimulated genes and the universal negative control siRNA were purchased from Bioneer (South Korea). Target sequences for siRNAs are listed in Table 3. siRNA transfection was performed using a Lipofectamine RNAiMax reagent (Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions.
Immunoblot analysis
Cells were harvested and lysed in a buffer containing 50 mM Tris HCl (pH 7.5), 150 mM NaCl, 1% NP-40, 1 mM EDTA, 0.25% sodium deoxycholate, 1 mM Na3VO4, 1 mM sodium fluoride, 1 mM phenylmethylsulfonyl fluoride, 1 mM β-glycerophosphate, and protease inhibitor cocktail (Roche) for 30 min on ice, and centrifuged at 12,000 rpm for 10 min at 4 °C. The supernatant was collected and equal amounts of protein were subjected to SDS-PAGE and then electrotransferred to a nitrocellulose membrane. The membrane was blocked in TBST buffer (20 mM Tris–HCl (pH 7.6), 150 mM NaCl, and 0.2% Tween 20) containing 5% non-fat dry milk for 1 h and then incubated overnight at 4 °C with the indicated antibodies in TBST buffer containing 1% BSA. The SARS-CoV-2 nucleoprotein was detected using a primary anti-nucleoprotein antibody (1/4000 dilution) (Sino Biological, China), and the secondary goat anti-rabbit antibody (1/5000 dilution) (Jackson ImmunoResearch Laboratories, West Grove, PA, USA). Actin was detected by the monoclonal anti-actin primary antibody (1/3000 dilution) (Sigma- Alrdrich, USA) and the secondary goat anti-mouse antibody (1/5000 dilution) (Jackson ImmunoResearch Laboratories, West Grove, PA, USA). Proteins were detected using an ECL kit (Amersham Biosciences).
Immunofluorescence assay
Vero E6 cells seeded on cover glass were infected with SARS-CoV-2 at an MOI of 0.01 in the absence or presence of 100 µg/ml YSK-A for 24 h. Cells were rinsed in PBS and fixed with 4% paraformaldehyde for 10 min. After two washes in PBS, fixed cells were permeabilized with 0.1% Triton X-100 in PBS for 15 min. Cells were then blocked in 0.5% BSA in PBS for 1 h and incubated overnight with mouse monoclonal anti-dsRNA J2 antibody (1/1000 dilution) (English & Scientific Consulting, J21003). After three washes in PBS, cells were incubated with FITC-conjugated goat anti-mouse (1/1000 dilution) (Jackson ImmunoResearch Laboratories, West Grove, PA, USA). Cells were also counterstained with 4′,6′-diamidino-2-phenylindole (DAPI) for 10 min to label nuclei. Fluorescence was analyzed by using the Zeiss LSM 700 laser 397 confocal microscopy system (Carl Zeiss, Inc., Thornwood, NY) and CELENA® S Digital Imaging System 398 (Logos Biosystems, Inc.).
Statistical analysis
Data are presented as the means ± standard deviations (SDs). Statistical analysis was performed by Student’s t test for two treatments and one-way analysis of variance (ANOVA) for multiple treatments. Dunnett’s test was used as a post hoc test. All statistical analyses were performed using IBM® SPSS® statistic v22 (IBM). Half-maximal effective (IC50) concentrations of YSK-A were estimated by nonlinear regression analysis using the GraphPad Prism v9 (GraphPad Software, San Diego, CA, USA). All graphs were drawn using GraphPad Prism and Excel 2016 (Microsoft). The asterisks or sharp in the figures indicate significant differences (*P < 0.05; **P < 0.01; ***P < 0.001; ns, not significant).
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
References
Hoareau, L. & DaSilva, E. J. Medicinal plants: A re-emerging health aid. Electron. J. Biotechnol. 2, 3–4 (1999).
Jahan, I. & Ahmet, O. Potentials of plant-based substance to inhabit and probable cure for the COVID-19. Turk. J. Biol. 44, 228 (2020).
Ang, L., Lee, H. W., Choi, J. Y., Zhang, J. & Lee, M. S. Herbal medicine and pattern identification for treating COVID-19: A rapid review of guidelines. Integr. Med. Res. 9, 100407 (2020).
Ngwe Tun, M. M. et al. The discovery of herbal drugs and natural compounds as inhibitors of SARS-CoV-2 infection in vitro. J. Nat. Med. 76, 402–409 (2022).
Matsabisa, M. et al. In vitro study on efficacy of PHELA, an African traditional drug against SARS-CoV-2. Sci. Rep. 12, 10305 (2022).
WHO. WHO Coronavirus Disease (COVID-19) Dashboard. Accessed September 2023 (2023).
Zou, L. et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 382, 1177–1179 (2020).
Ding, Q., Lu, P., Fan, Y., Xia, Y. & Liu, M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan. China. J. Med. Virol. 92, 1549–1555 (2020).
Karki, R. et al. Synergism of TNF-α and IFN-γ triggers inflammatory cell death, tissue damage, and mortality in SARS-CoV-2 infection and cytokine shock syndromes. Cell 184, 149–168 (2021).
Li, G., Hilgenfeld, R., Whitley, R. & De Clercq, E. Therapeutic strategies for COVID-19: Progress and lessons learned. Nat. Rev. Drug Discov. 22(6), 449–475 (2023).
Yang, M.-S. et al. Antiviral and therapeutic effects of a mixture of Boswellia serrata, Commiphora myrrha, and Propolis for SARS-CoV-2. Nat. Prod. Commun. 18, 1934578X231180709 (2023).
Ramirez, S. et al. Overcoming culture restriction for SARS-CoV-2 in human cells facilitates the screening of compounds inhibiting viral replication. Antimicrob. Agents Chemother. 65(7), e0009721 (2021).
Diemer, C. et al. Cell type-specific cleavage of nucleocapsid protein by effector caspases during SARS Coronavirus infection. J. Mol. Biol. 376, 23–34 (2008).
Lim, Y. S. et al. Asunaprevir, a potent hepatitis C virus protease inhibitor, blocks SARS-CoV-2 propagation. Mol. Cells. 44(9), 688–695 (2021).
Than, T. T. et al. Ankyrin repeat domain 1 is up-regulated during hepatitis C virus infection and regulates hepatitis C virus entry. Sci. Rep. 6, 20819 (2016).
Amraei, R. et al. Extracellular vimentin is an attachment factor that facilitates SARS-CoV-2 entry into human endothelial cells. Proc. Natl. Acad. Sci. U.S.A. 119, e2113874119 (2022).
Suprewicz, Ł et al. Extracellular vimentin as a target against SARS-CoV-2 host cell invasion. Small 18, 2105640 (2022).
Lee, H. Y. et al. Inhibition of HCV replicon cell growth by 2-Arylbenzofuran derivatives isolated from Mori Cortex radicis. Planta Med. 73, 1481–1485 (2007).
Kim, J. W. et al. Triterpenoid saponins isolated from Platycodon grandiflorum inhibit hepatitis C virus replication. Evid. Based Complementary Altern. Med. 2013, 560417 (2013).
Lee, J. et al. Saponin inhibits hepatitis C virus propagation by up-regulating suppressor of cytokine signaling 2. PLoS One 7, e39366 (2012).
Sayed, A. M. et al. Nature as a treasure trove of potential anti-SARS-CoV drug leads: A structural/mechanistic rationale. RSC Adv. 10, 19790–19802 (2020).
Gayathri, B., Manjula, N., Vinaykumar, K., Lakshmi, B. & Balakrishnan, A. Pure compound from Boswellia serrata extract exhibits anti-inflammatory property in human PBMCs and mouse macrophages through inhibition of TNFα, IL-1β. NO and MAP kinases. Int. Immunopharmacol. 7, 473–482 (2007).
Siddiqui, M. Z. Boswellia serrata, a potential antiinflammatory agent: An overview. Indian J. Pharm. Sci. 73, 255 (2011).
Beghelli, D. et al. Antioxidant and ex vivo immune system regulatory properties of Boswellia serrata extracts. Oxid. Med. Cell. Longev. 2017, 7468064 (2017).
Etzel, R. Special extract of Boswellia serrata (H 15) in the treatment of rheumatoid arthritis. Phytomedicine 3, 91–94 (1996).
Gupta, I. et al. Effects of Boswellia serrata gum resin in patients with ulcerative colitis. Eur. J. Med. Res. 2, 37–43 (1997).
Gupta, I. et al. Effects of gum resin of Boswellia serrata in patients with chronic colitis. Planta Med. 67, 391–395 (2001).
Su, S. et al. Anti-inflammatory and analgesic activity of different extracts of Commiphora myrrha. J. Ethnopharmacol. 134, 251–258 (2011).
Germano, A., Occhipinti, A., Barbero, F. & Maffei, M. E. A pilot study on bioactive constituents and analgesic effects of MyrLiq®, a Commiphora myrrha extract with a high furanodiene content. Biomed Res. Int. 2017, 3804356 (2017).
Mohamed, A. A., Ali, S. I., El-Baz, F. K., Hegazy, A. K. & Kord, M. A. Chemical composition of essential oil and in vitro antioxidant and antimicrobial activities of crude extracts of Commiphora myrrha resin. Ind. Crops Prod. 57, 10–16 (2014).
Ansari, S., Ahmad, I., Ali, M. & Maaz, M. “Tiryaq Arba”(a polyherbal Unani formulation) as prophylactic medicine against epidemics of acute respiratory viral infections. Middle East J. Rehabil. Health Stud. 7(3), e102965 (2020).
Ahmed, N. Z. et al. In-silico evaluation of Tiryaq-e-wabai, an Unani formulation for its potency against SARS-CoV-2 spike glycoprotein and main protease. J. Drug Deliv. Ther. 11, 86–100 (2021).
Fatima, S. W., Alam, S. & Khare, S. K. Molecular and structural insights of β-boswellic acid and glycyrrhizic acid as potent SARS-CoV-2 Envelope protein inhibitors. Phytomed. Plus 2, 100241 (2022).
Roy, A. & Menon, T. Evaluation of bioactive compounds from Boswellia serrata against SARS-CoV-2. Vegetos 35, 404–414 (2022).
Tosi, B., Donini, A., Romagnoli, C. & Bruni, A. Antimicrobial activity of some commercial extracts of propolis prepared with different solvents. Phytother. Res. 10, 335–336 (1996).
McLennan, S. V. et al. The anti-inflammatory agent Propolis improves wound healing in a rodent model of experimental diabetes. Wound Repair Regen. 16, 706–713 (2008).
Santos, L. M. et al. Propolis: Types, composition, biological activities, and veterinary product patent prospecting. J. Sci. Food Agric. 100, 1369–1382 (2020).
Scorza, C. A. et al. Propolis and coronavirus disease 2019 (COVID-19): Lessons from nature. Complement. Ther. Clin. Pract. 41, 101227 (2020).
Ali, A. M. & Kunugi, H. Propolis, bee honey, and their components protect against coronavirus disease 2019 (COVID-19): A review of in silico, in vitro, and clinical studies. Molecules 26, 1232 (2021).
Aparecida Berretta, A., Duarte Silveira, M. A., Condor Capcha, J. M. & De Jong, D. Propolis and its potential against SARS-CoV-2 infection mechanisms and COVID-19 disease. Biomed. Pharmacother. 131, 110622 (2020).
Guyonnet Duperat, V. et al. Characterization of the human mucin gene MUC5AC: A consensus cysteine-rich domain for 11p15 mucin genes?. Biochem. J. 305, 211–219 (1995).
Lee, S. et al. SARS-CoV-2 induces expression of cytokine and MUC5AC/5B in human nasal epithelial cell through ACE 2 receptor. Biomed Res. Int. 2022, 2743046 (2022).
Morrison, C. B. et al. SARS-CoV-2 infection of airway cells causes intense viral and cell shedding, two spreading mechanisms affected by IL-13. Proc. Natl. Acad. Sci. 119, e2119680119 (2022).
Bonser, L. R., Zlock, L., Finkbeiner, W. & Erle, D. J. Epithelial tethering of MUC5AC-rich mucus impairs mucociliary transport in asthma. J. Clin. Investig. 126, 2367–2371 (2016).
Zhu, Z. et al. Association of asthma and its genetic predisposition with the risk of severe COVID-19. J. Allergy Clin. Immunol. 146, 327–329 (2020).
Foronjy, R. F., Dabo, A. J., Cummins, N. & Geraghty, P. Leukemia inhibitory factor protects the lung during respiratory syncytial viral infection. BMC Immunol. 15, 1–15 (2014).
Quinton, L. J. et al. Leukemia inhibitory factor signaling is required for lung protection during pneumonia. J Immunol. 188, 6300–6308 (2012).
Metcalfe, S. M. LIF and the lung’s stem cell niche: Is failure to use LIF to protect against COVID-19 a grave omission in managing the pandemic?. Future Med. 15, 659–662 (2020).
Giovannoni, F., Li, Z., Garcia, C. C. & Quintana, F. J. A potential role for AHR in SARS-CoV-2 pathology. Res. Sq. 2020, 2rs.3.rs-5639 (2020).
Kozaki, T. et al. Mitochondrial damage elicits a TCDD-inducible poly (ADP-ribose) polymerase-mediated antiviral response. Proc. Natl. Acad. Sci. 114, 2681–2686 (2017).
Yamada, T. et al. Constitutive aryl hydrocarbon receptor signaling constrains type I interferon–mediated antiviral innate defense. Nat. Immunol. 17, 687–694 (2016).
Zhu, Y., Song, D., Song, Y. & Wang, X. Interferon gamma induces inflammatory responses through the interaction of CEACAM1 and PI3K in airway epithelial cells. J. Transl. Med. 17, 1–10 (2019).
Sharif-Askari, N. S. et al. Enhanced expression of immune checkpoint receptors during SARS-CoV-2 viral infection. Mol. Ther. Methods Clin. Dev. 20, 109–121 (2021).
Vitenshtein, A. et al. CEACAM1-mediated inhibition of virus production. Cell Rep. 15, 2331–2339 (2016).
Zhao, B. et al. Negative regulators of inflammation response to the dynamic expression of cytokines in DF-1 and MDCK cells infected by avian influenza viruses. Inflamm. 45(2), 573–589 (2022).
Rochette, L. et al. GDF15: A modulator of immunity and a predictive biomarker of cardiovascular events: A strategy in COVID-19. Ann. Cardiol. Angeiol. 72(1), 41–43 (2023).
Babalghith, A. O. et al. The potential role of growth differentiation factor 15 in COVID-19: A corollary subjective effect or not?. Diagnostics 12, 2051 (2022).
Si, Y. et al. Growth differentiation factor 15 is induced by hepatitis C virus infection and regulates hepatocellular carcinoma-related genes. PloS One 6, e19967 (2011).
Cheng, J. et al. The regulation of ISG20 expression on SARS-CoV-2 infection in cancer patients and healthy individuals. Front. Immunol. 13, 958898 (2022).
Deymier, S., Louvat, C., Fiorini, F. & Cimarelli, A. ISG20: An enigmatic antiviral RNase targeting multiple viruses. FEBS Open Bio 12, 1096–1111 (2022).
Furutani, Y. et al. Establishment of a rapid detection system for ISG20-dependent SARS-CoV-2 subreplicon RNA degradation induced by interferon-α. Int. J. Mol. Sci. 22, 11641 (2021).
Qu, H. et al. Influenza A Virus-induced expression of ISG20 inhibits viral replication by interacting with nucleoprotein. Virus genes 52, 759–767 (2016).
Stadler, D. et al. Interferon-induced degradation of the persistent hepatitis B virus cccDNA form depends on ISG20. EMBO Rep. 22, e49568 (2021).
Wickenhagen, A. et al. A prenylated dsRNA sensor protects against severe COVID-19. Science 374, eabj3624 (2021).
Danziger, O., Patel, R. S., DeGrace, E. J., Rosen, M. R. & Rosenberg, B. R. Inducible CRISPR activation screen for interferon-stimulated genes identifies OAS1 as a SARS-CoV-2 restriction factor. PLoS Pathog. 18, e1010464 (2022).
Banday, A. R. et al. Genetic regulation of OAS1 nonsense-mediated decay underlies association with COVID-19 hospitalization in patients of European and African ancestries. Nat. Genet. 54, 1103–1116 (2022).
Chen, J. et al. Cellular immune responses to severe acute respiratory syndrome coronavirus (SARS-CoV) infection in senescent BALB/c mice: CD4+ T cells are important in control of SARS-CoV infection. J. Virol. 84, 1289–1301 (2010).
Zhang, Y. et al. The diverse roles and dynamic rearrangement of vimentin during viral infection. J. Cell. Sci. 134, jcs250597 (2021).
Yu, Y.T.-C. et al. Surface vimentin is critical for the cell entry of SARS-CoV. J. Biomed. Sci. 23, 1–10 (2016).
Huynh, T. T. et al. Amuvatinib blocks SARS-CoV-2 infection at the entry step of the viral life cycle. Microbiol. Spectr. 11(3), e0510522 (2023).
Reed, L. J. & Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 27, 493–497 (1938).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Dobin, A. et al. STAR: Ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Li, B. & Dewey, C. N. RSEM: Accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform. 12, 1–16 (2011).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 17, 10–12 (2011).
Robinson, M. D. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 11, 1–9 (2010).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2021R1A2C2003275 for S.B.H.). This work was also supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2022R1A2B5B01001390 for Y.S.L.). This work was partly supported by Yeskin, Korea
Author information
Authors and Affiliations
Contributions
All authors reviewed the manuscript and have given approval to the final version of the manuscript. T.X.P. and T.T.X.H. performed experiments, analyzed data, and wrote the manuscript. B.K. provided reagents and expertise. Y.S.L. and S.B.H. designed experiments and secured funding. S.B.H. supervised the study and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pham, T.X., Huynh, T.T.X., Kim, B. et al. A natural product YSK-A blocks SARS-CoV-2 propagation by targeting multiple host genes. Sci Rep 13, 21489 (2023). https://doi.org/10.1038/s41598-023-48854-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48854-3