Abstract
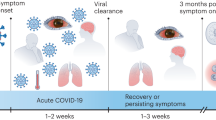
Up to 25% of individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exhibit postacute cognitive sequelae. Although millions of cases of coronavirus disease 2019 (COVID-19)-mediated memory dysfunction are accumulating worldwide, the underlying mechanisms and how vaccination lowers risk are unknown. Interleukin-1 (IL-1), a key component of innate immune defense against SARS-CoV-2 infection, is elevated in the hippocampi of individuals with COVID-19. Here we show that intranasal infection of C57BL/6J mice with SARS-CoV-2 Beta variant leads to central nervous system infiltration of Ly6Chi monocytes and microglial activation. Accordingly, SARS-CoV-2, but not H1N1 influenza virus, increases levels of brain IL-1β and induces persistent IL-1R1-mediated loss of hippocampal neurogenesis, which promotes postacute cognitive deficits. Vaccination with a low dose of adenoviral-vectored spike protein prevents hippocampal production of IL-1β during breakthrough SARS-CoV-2 infection, loss of neurogenesis and subsequent memory deficits. Our study identifies IL-1β as one potential mechanism driving SARS-CoV-2-induced cognitive impairment in a new mouse model that is prevented by vaccination.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Source data are provided with this paper.
References
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
O’Mahoney, L. L. et al. The prevalence and long-term health effects of long COVID among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine 55, 101762 (2023).
Han, Q., Zheng, B., Daines, L. & Sheikh, A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens 11, 269 (2022).
Centers for Disease Control and Prevention, National Center for Health Statistics. Long COVID—Household Pulse Survey. https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm (2023).
Hua, M. J. et al. Prevalence and characteristics of long COVID 7–12 months after hospitalization among patients from an urban safety-net hospital: a pilot study. AJPM Focus 2, 100091 (2023).
Perlis, R. H. et al. Prevalence and correlates of long COVID symptoms among US adults. JAMA Netw. Open 5, e2238804 (2022).
Taquet, M. et al. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 18, e1003773 (2021).
Xu, E., Xie, Y. & Al-Aly, Z. Long-term neurologic outcomes of COVID-19. Nat. Med. 28, 2406–2415 (2022).
Mehandru, S. & Merad, M. Pathological sequelae of long-haul COVID. Nat. Immunol. 23, 194–202 (2022).
Méndez, R. et al. Long-term neuropsychiatric outcomes in COVID-19 survivors: a 1-year longitudinal study. J. Intern. Med. 291, 247–251 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022).
Hampshire, A. et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine 39, 101044 (2021).
Guo, P. et al. COVCOG 2: cognitive and memory deficits in long COVID: a second publication from the COVID and cognition study. Front. Aging Neurosci. 14, 804937 (2022).
Graham, E. L. et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized COVID-19 ‘long haulers’. Ann. Clin. Transl. Neurol. 8, 1073–1085 (2021).
Monje, M. & Iwasaki, A. The neurobiology of long COVID. Neuron 110, 3484–3496 (2022).
Klein, R. S. Mechanisms of coronavirus infectious disease 2019-related neurologic diseases. Curr. Opin. Neurol. 35, 392–398 (2022).
Soung, A. L. et al. COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis. Brain 145, 4193–4201 (2022).
Grant, R. A. et al. Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia. Nature 590, 635–641 (2021).
Schwabenland, M. et al. Deep spatial profiling of human COVID-19 brains reveals neuroinflammation with distinct microanatomical microglia–T-cell interactions. Immunity 54, 1594–1610 (2021).
Jensen, M. P. et al. Neuropathological findings in two patients with fatal COVID-19. Neuropathol. Appl. Neurobiol. 47, 17–25 (2021).
Matschke, J. et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19, 919–929 (2020).
Thakur, K. T. et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 144, 2696–2708 (2021).
Bird, C. M. & Burgess, N. The hippocampus and memory: insights from spatial processing. Nat. Rev. Neurosci. 9, 182–194 (2008).
Zemla, R. & Basu, J. Hippocampal function in rodents. Curr. Opin. Neurobiol. 43, 187–197 (2017).
Basu, J. & Siegelbaum, S. A. The corticohippocampal circuit, synaptic plasticity, and memory. Cold Spring Harb. Perspect. Biol. 7, a021733 (2015).
Toda, T., Parylak, S. L., Linker, S. B. & Gage, F. H. The role of adult hippocampal neurogenesis in brain health and disease. Mol. Psychiatry 24, 67–87 (2019).
Kumar, A., Pareek, V., Faiq, M. A., Ghosh, S. K. & Kumari, C. Adult neurogenesis in humans: a review of basic concepts, history, current research, and clinical implications. Innov. Clin. Neurosci. 16, 30–37 (2019).
Hein, A. M. et al. Sustained hippocampal IL-1β overexpression impairs contextual and spatial memory in transgenic mice. Brain Behav. Immun. 24, 243–253 (2010).
Wu, M. D. et al. Adult murine hippocampal neurogenesis is inhibited by sustained IL-1β and not rescued by voluntary running. Brain Behav. Immun. 26, 292–300 (2012).
Soung, A. L. et al. IL-1 reprogramming of adult neural stem cells limits neurocognitive recovery after viral encephalitis by maintaining a proinflammatory state. Brain Behav. Immun. 99, 383–396 (2022).
Garber, C. et al. Astrocytes decrease adult neurogenesis during virus-induced memory dysfunction via IL-1. Nat. Immunol. 19, 151–161 (2018).
Schultheiß, C. et al. The IL-1β, IL-6, and TNF cytokine triad is associated with post-acute sequelae of COVID-19. Cell Rep. Med. 3, 100663 (2022).
Català, M. et al. The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia. Lancet Respir. Med. 12, 225–236 (2024).
Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 28, 1461–1467 (2022).
Huapaya, J. A. et al. Vaccination ameliorates cellular inflammatory responses in SARS-CoV-2 breakthrough infections. J. Infect. Dis. 228, 46–58 (2023).
Zhu, X. et al. Dynamics of inflammatory responses after SARS-CoV-2 infection by vaccination status in the USA: a prospective cohort study. Lancet Microbe 4, e692–e703 (2023).
Fan, Q. et al. Clinical characteristics and immune profile alterations in vaccinated individuals with breakthrough Delta SARS-CoV-2 infections. Nat. Commun. 13, 3979 (2022).
Vanderheiden, A. et al. CCR2 signaling restricts SARS-CoV-2 infection. mBio 12, e0274921 (2021).
Shuai, H. et al. Emerging SARS-CoV-2 variants expand species tropism to murines. EBioMedicine 73, 103643 (2021).
Pan, T. et al. Infection of wild-type mice by SARS-CoV-2 B.1.351 variant indicates a possible novel cross-species transmission route. Signal Transduct. Target. Ther. 6, 420 (2021).
Leger, M. et al. Object recognition test in mice. Nat. Protoc. 8, 2531–2537 (2013).
Vasek, M. J. et al. A complement–microglial axis drives synapse loss during virus-induced memory impairment. Nature 534, 538–543 (2016).
Rosen, S. F. et al. Single-cell RNA transcriptome analysis of CNS immune cells reveals CXCL16/CXCR6 as maintenance factors for tissue-resident T cells that drive synapse elimination. Genome Med. 14, 108 (2022).
Brannock, M. D. et al. Long COVID risk and pre-COVID vaccination in an EHR-based cohort study from the RECOVER program. Nat. Commun. 14, 2914 (2023).
Notarte, K. I. et al. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: a systematic review. EClinicalMedicine 53, 101624 (2022).
Bricker, T. L. et al. A single intranasal or intramuscular immunization with chimpanzee adenovirus-vectored SARS-CoV-2 vaccine protects against pneumonia in hamsters. Cell Rep. 36, 109400 (2021).
Antunes, M. & Biala, G. The novel object recognition memory: neurobiology, test procedure, and its modifications. Cogn. Process. 13, 93–110 (2012).
Yang, A. C. et al. Dysregulation of brain and choroid plexus cell types in severe COVID-19. Nature 595, 565–571 (2021).
Fullard, J. F. et al. Single-nucleus transcriptome analysis of human brain immune response in patients with severe COVID-19. Genome Med. 13, 118 (2021).
Lee, M. H. et al. Neurovascular injury with complement activation and inflammation in COVID-19. Brain 145, 2555–2568 (2022).
Lage, S. L. et al. Persistent oxidative stress and inflammasome activation in CD14highCD16– monocytes from COVID-19 patients. Front. Immunol. 12, 799558 (2021).
Junqueira, C. et al. FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation. Nature 606, 576–584 (2022).
Fernández-Castañeda, A. et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell 185, 2452–2468 (2022).
Reagin, K. L. & Funk, K. E. The role of antiviral CD8+ T cells in cognitive impairment. Curr. Opin. Neurobiol. 76, 102603 (2022).
Garber, C. et al. T cells promote microglia-mediated synaptic elimination and cognitive dysfunction during recovery from neuropathogenic flaviviruses. Nat. Neurosci. 22, 1276–1288 (2019).
Sun, Y., Koyama, Y. & Shimada, S. Inflammation from peripheral organs to the brain: how does systemic inflammation cause neuroinflammation? Front. Aging Neurosci. 14, 903455 (2022).
Lee, J. S. et al. Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19. Sci. Immunol. 5, eabd1554 (2020).
Frere, J. J. et al. SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations after recovery. Sci. Transl. Med. 14, eabq3059 (2022).
Grønkjær, C. S., Christensen, R. H. B., Kondziella, D. & Benros, M. E. Long-term neurological outcome after COVID-19 using all SARS-CoV-2 test results and hospitalisations in Denmark with 22-month follow-up. Nat. Commun. 14, 4235 (2023).
Zarifkar, P., Peinkhofer, C., Benros, M. E. & Kondziella, D. Frequency of neurological diseases after COVID-19, influenza A/B and bacterial pneumonia. Front. Neurol. 13, 904796 (2022).
Dinarello, C. A. Immunological and inflammatory functions of the interleukin-1 family. Annu Rev. Immunol. 27, 519–550 (2009).
Trevino, T. N. et al. Engineered Wnt7a ligands rescue blood–brain barrier and cognitive deficits in a COVID-19 mouse model. Brain 147, 1636–1643 (2024).
Wenzel, J. et al. The SARS-CoV-2 main protease Mpro causes microvascular brain pathology by cleaving NEMO in brain endothelial cells. Nat. Neurosci. 24, 1522–1533 (2021).
Bowe, B., Xie, Y. & Al-Aly, Z. Post acute sequelae of COVID-19 at 2 years. Nat. Med. 29, 2347–2357 (2023).
Chen, R. E. et al. Resistance of SARS-CoV-2 variants to neutralization by monoclonal and serum-derived polyclonal antibodies. Nat. Med. 27, 717–726 (2021).
Zang, R. et al. TMPRSS2 and TMPRSS4 promote SARS-CoV-2 infection of human small intestinal enterocytes. Sci. Immunol. 5, eabc3582 (2020).
Szretter, K. J. et al. 2′-O-Methylation of the viral mRNA cap by West Nile virus evades IFIT1-dependent and -independent mechanisms of host restriction in vivo. PLoS Pathog. 8, e1002698 (2012).
Williams, G. D. et al. Nucleotide resolution mapping of influenza A virus nucleoprotein–RNA interactions reveals RNA features required for replication. Nat. Commun. 9, 465 (2018).
Case, J. B., Bailey, A. L., Kim, A. S., Chen, R. E. & Diamond, M. S. Growth, detection, quantification, and inactivation of SARS-CoV-2. Virology 548, 39–48 (2020).
Hassan, A. O. et al. A single-dose intranasal ChAd vaccine protects upper and lower respiratory tracts against SARS-CoV-2. Cell 183, 169–184 (2020).
Vanderheiden, A. et al. Development of a rapid focus reduction neutralization test assay for measuring SARS-CoV-2 neutralizing antibodies. Curr. Protoc. Immunol. 131, e116 (2020).
Acknowledgements
We thank M. S. Diamond (Washington University in St. Louis) for the ChAd-S vaccine, WNV stock and Vero cells. We thank M. S. Suthar for the B.1.351 variant of SARS-CoV-2. We thank W. Beatty from the Washington University in St. Louis Microscopy Core Facility for her assistance and technical expertise. Imaging and Imaris analyses were performed, in part, through the use of Washington University Center for Cellular Imaging supported by Washington University School of Medicine, The Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital (CDI-CORE-2015-505 and CDI-CORE-2019-813) and the Foundation for Barnes-Jewish Hospital (3770 and 4642). Flow cytometry analysis was supported, in part, by the Bursky Center for Human Immunology and Immunotherapy Programs at Washington University, Immunomonitoring Laboratory. This work was supported by F32NS128065 (to A.V.), R01NS104471, R35 NS122310 and R01 AI160188 (all to R.S.K.) and R01-AI139251 (to A.C.M.B.).
Author information
Authors and Affiliations
Contributions
A.V. and R.S.K. conceived and designed the study and wrote the paper. A.V., J.H., X.J., B.D., G.B., N.S., A.J. and M.D.C. contributed to the acquisition of data. A.V., J.H., M.D.C., A.C.M.B. and R.S.K. contributed to data analysis and interpretation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Immunology thanks Changyoun Kim and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: L. A. Dempsey, in collaboration with the Nature Immunology team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Sex does not impact B.1.351 infection.
Mice were intranasally infected with B.1.351 (5 ×105 pfu). a) Weight loss curves for mice infected at 8, 10, or 20 weeks of age (all male, n = 5-6). b) Weight loss curves for 16-week-old male or female mice infected with B.1.351 (n = 6-8). c) Viral titer in the Nasal turbinates and lung from 2 (n = 9), 4 (n = 8), 6 (n = 9), 8 (n = 12), 12 (n = 6) dpi measured via plaque assay. d) RNA transcript levels of Ifnb, Ifng, Il1b, Tnf at 4 and 6 dpi represented as fold change over mock (6 dpi) in the lung (n = 4). e) Representative image of Spike RNA in situ hybridization for an entire sagittal section of the brain from 4 dpi counterstained with hematoxylin. f) Indicated Open field measurement for combined sexes at 30 dpi (n = 19). g) Representative image of Novel Object apparatus set-up. On the right the percentage of investigations of each object during a preference test (n = 4). h) Selected open field measurements for male vs female mice at 30 dpi (n = 9). i) The discrimination index for the NOR test for B.1.351 infected male (n = 18) vs female mice (n = 20) is displayed on the left at 30 dpi. On the right, the discrimination index plotted vs the maximum weight lost during infection. Linear regression was used to calculate the R-squared and p-value are displayed on chart (n = 19). Data is represented as mean with SEM and was pooled (F-I) or representative (A-E) of 2-4 independent experiments. Statistical significance was determined using an unpaired, two-tailed, student’s t-test (F, I) or Welch’s one-way ANOVA with Dunnett’s multiple comparisons test (F), ordinary two-way ANOVA with Sidak’s multiple correction test (A, H), or simple linear regression (I).
Extended Data Fig. 2 T cells are increased in the cortex after SARS-CoV-2 infection.
Mice were intranasally infected with B.1.351 and euthanized at the indicated timepoint. a) Representative plots of the cortex at 30 dpi showing gating strategy for blood, cortex, and hippocampus. b) Frequency of the indicated population as a percentage of the total CD45+ cells in the blood at 6 dpi and c) 30 dpi d) Frequency of Ly6CLo or Hi cells in the total CD45HiCD11b+ population at 6 and 30 dpi in the blood. e) The count per gram of tissue for the indicated cell population in the cortex (top) or hippocampus (bottom) at 6 dpi or f) 30 dpi. 6 dpi: Mock n = 9, B.1.351 n = 8, 30 dpi: mock n = 8, B.1.351 n = 9. Data is represented as mean with SEM and was pooled from 2 independent experiments. Statistical significance was determined using an unpaired, two-tailed, student’s t-test (A-F).
Extended Data Fig. 3 Microglia are activated in the hippocampus after B.1.351 infection.
a) Representative pseudocolor flow plots showing expression of P2RY12 or Ly6C on CD45MidCD11b+ cells from the cortex at 6 dpi from B.1.351 infected mice. b) Representative images of IBA-1 expression in the DG after B.1.351 infection or mock at 6 and 30 dpi (40X magnification). Below is the percentage of IBA-1+ area in the indicated hippocampal region at mock (n = 6), 2 (n = 3), 4 (n = 3), 6 (n = 6), 8 (n = 4) dpi and 30 dpi (n = 10). c) Morphological measurements of IBA-1 or total IBA-1 count in the DG from mock and B.1.351 infected animals at the indicated timepoint (6 dpi n = 8, 30 dpi n = 6). All image analysis and acquisition were performed blinded and quantification was averaged from 2-4 slices for each mouse. Scale bar is 20 μM. Data is represented as mean with SEM and was representative of 2 independent experiments. Statistical significance was determined using an unpaired, two-tailed, student’s t-test (C) or Welch’s one-way ANOVA with Dunnett’s multiple comparisons test (B).
Extended Data Fig. 4 B.1.351 does not induce higher serum cytokine levels compared to PR8 infection.
C57Bl/6J mice at 14 weeks of age were intranasally infected with B.1.351, PR8 (2000 TCID50) or mock infected with PBS. a) The percent of original weight for mock and PR8 infected mice (n = 8). b) qRT-PCR was performed for the M gene of PR8 lung, cortex, and hippocampus. Values are represented as delta CT normalized to GAPDH. Dotted line indicates the limit of detection. c) qRT-PCR was performed for the indicated gene on mock, 3, and 6 dpi samples from the lung (n = 4). Multiplex analysis of serum cytokines was performed on mock (n = 8), B.1.351 (n = 5) and PR8 (n = 4) animals at 6 dpi. d) Cytokine levels represented as fold change over mock levels. e) concentration of the indicated cytokine in the serum at 7 dpi (IFNg). Data is represented as mean with SEM and was pooled or representative of 2 independent experiments. Statistical significance was determined using a Welch’s one-way ANOVA with Dunnett’s multiple comparisons test (B-C, E) for A this test was performed on the area under the curve.
Extended Data Fig. 5 PR8 infection does not induce hippocampal IL-1β.
C57Bl/6J mice at 14 weeks of age were intranasally infected with B.1.351, PR8 (2000 TCID50) or mock infected with PBS. a) qRT-PCR was performed for the indicated gene on mock, 3, and 6 dpi samples from the cortex and hippocampus (n = 4). b) Representative images of Isotype control for IL-1β (Goat IgG) from 6 dpi B.1.351 mice on the left. On the right, mice were intracranially infected with WNV-E218A, harvested at 7 dpi and hippocampal slices were stained for IL-1β expression. c) Representative images of IL-1β staining in the DG (40X magnification) with quantification of the total percent IL-1β + are on the right for the DG, CA3, and CA1 for mock (n = 7) and 6 dpi PR8 (n = 7) or B.1.351 (n = 4). d) Representative images of IBA-1 staining in the DG (40X magnification) with the total % IBA-1 area quantified on the right for mock (n = 7) and 6 dpi PR8 (n = 7) or B.1.351 (n = 4). All image analysis and acquisition were performed blinded and quantification was averaged from 2-4 slices for each mouse. Scale bar is 20 μM. Data is represented as mean with SEM and was pooled from 2 independent experiments. Statistical significance was determined using Welch’s one-way ANOVA with Dunnett’s multiple comparisons test (A, C-D).
Extended Data Fig. 6 Inhibition of neurogenesis begins at neuroblast stage and does not occur during PR8 infection.
C57Bl/6 mice were intranasally infected with B.1.351 or PR8. a) Quantification of the total number of DCX+ (o.p.=0.03) or Ki67+ cells per arbitrary unit (A.U.) of DG length. Samples from 2 (n = 3), 4 (n = 2), 6 (n = 7), 8 (n = 4) dpi are compared to a mock (M) from 6 dpi (n = 5) and representative of 2 independent experiments b) Representative image of TBR2 and Ki67 staining in the DG in mock (n = 4) or 6 dpi (n = 5), with quantification of cell number/ A.U. on the right (20X magnification). c) Representative images of Ki67 and DCX staining in the SGZ of the DG at 6 dpi from mock and PR8 infected animals (20X magnification). Quantified on the right is the number of DCX + , Ki67 + , and Ki67+ DCX+ (n = 8). Mice were intranasally infected with B.1.351 and harvested at the indicated timepoints. d) Number of synaptophysin+ puncta or homer+ puncta represented as the % of the number of average mock puncta in the indicated sub-region of the hippocampus at 8 (n = 7) and 15 dpi (n = 5) are compared to 8 dpi mock (n = 8). Or at e) 30 dpi (n = 9) is compared to a day 30 mock (n = 8). f) Representative images of the DG showing staining for NeuN, TUNEL, and DAPI (20X magnification). Below, quantification of the total number of TUNEL+ NeuN+ cells per mm2 for each subregion of the hippocampus (n = 5). All image analysis and acquisition were performed blinded and quantification was averaged from 2-4 slices for each mouse. Scale bar is 20 μM. Data is represented as mean with SEM and was pooled from 2 independent experiments. Statistical significance was determined using an unpaired, two-tailed, student’s t-test (B-D) or Welch’s one-way ANOVA with Dunnett’s multiple comparisons test (A, E-G).
Extended Data Fig. 7 IL-1R1 signaling on NSCs does not impact synapse formation.
Nestin-CreERT2 x IL-1R1fl/fl littermates (Cre+ and Cre-) were intraperitoneally (I.P.) injected with Tamoxifen for 5 days. 10 days after the last tamoxifen injection, mice were intranasally infected with B.1.351. a) Weight loss curves for Mock and B.1.351 infected Nestin-Cre- and Nestin-Cre+ mice (n = 6). b) Representative z-stacks of DCX and Ki67 staining in the DG (20X) with enlarged regions below. c) Quantification of number of DCX+ or Ki67+ cells per arbitrary unit (A.U.) of DG at 6 (n = 6, Cre+ B.1.351 n = 9), or 30 dpi (mock, n = 5, B.1.351 n = 8, I.P.=n.s.). d) Representative z-stacks of Synaptophysin and Homer in the DG at 30 dpi (63X). e) Number of puncta for each marker and the number of overlapping (synapse) puncta was quantified as the total number of puncta per mm2 and represented as a percentage of the number of puncta in mock samples for each region (Mock: Cre- n = 7, Cre+ n = 4, B.1.351: n = 8, I.P.= n.s.). f) Mice were trained for the NOR test and the percentage of total investigations of identical Object 1a and 1b is shown for Mock and B.1.351 Nestin-Cre- and Nestin-Cre+ mice at 31 dpi. g) Selected open field measurements at 30 dpi (I.P.=n.s.). For F and G: Mock: Cre- n = 10, Cre+ n = 6, B.1.351: Cre- n = 11, Cre+ n = 11. h) Simple linear regressions between the discrimination index calculated from the Novel object test and the # of Ki67+DCX+ cells, the # of BrdU+ GFAP+ Cells, or the # of Synapse puncta for B.1.351 infected mice for Nestin-Cre- mice at 30 dpi (n = 11). All image analysis and acquisition was performed blinded and quantification was averaged from 3-5 slices for each mouse. Scale bar is 20 μM. Data is represented as mean with SEM and was pooled from 2 independent experiments. Statistical significance was determined via two-way ANOVA with Sidak’s multiple correction test (C, E-G) or simple linear regression (H).
Extended Data Fig. 8 Vaccination provides neutralizing antibodies in C57Bl/6 mice.
a) Experimental schematic: Mice were intranasally vaccinated with 108 ChAd-Spike (S) or empty vector ChAD-Control (CTL) at day -30 p.i. At day -7, a cheek bleed was performed. At day 0, mice were intranasally infected with 5 ×105 pfu B.1.351. Mice were harvested at the indicated timepoint. b) FRNTs were performed to measure the % of B.1.351 neutralized by serum collected at - 21 days post vaccination from ChAd-CTL or ChAd-S inoculated animals (n = 8). c). The total number of CD3+ cells (I.P.= n.s.), CD45mid CD11b+, or CD45high CD11b+ Ly6Clo cells per gram of tissue was quantified for mock and 6 dpi ChAd-CTL or ChAd-S animals via flow cytometry (n = 7). Data is represented as mean with standard error of the mean and either representative of or pooled from 2 independent experiments. Statistical significance was determined by two-way ANOVA with Sidak’s multiple correction test (C).
Extended Data Fig. 9 Vaccination does not impact open field performance after breakthrough infection.
Mice were intranasally vaccinated with 108 ChAd-S or ChAd-CTL, then challenged with B.1.351 30 days later. a) The number of DCX+ or Ki67+ cells per A.U. of DG in mock (n = 5) or 30 dpi (n = 6) in ChAd-CTL or ChAd-S mice (I.P.=n.s.). b) Selected open field test parameters measured at 30 dpi from ChAd-CTL or ChAd-S mice (n = 5-10, I.P.=n.s.). c) At 31 dpi, mice underwent training for the Novel Object test. On the left, the % of total investigations (nose pokes) spent with identical Object 1 A or 1B. On the right, the discrimination index for mock and 30 dpi ChAd-CTL and ChAd-S mice (I.P.=n.s.). For B-C: Mock: CTL n = 8, S = 9, B.1.351: CTL n = 12, S n = 14. Data is represented as mean with standard error of the mean and pooled from 2 independent experiments. Statistical significance was determined by two-way ANOVA with Sidak’s multiple correction test (A-C).
Supplementary information
Source data
Source Data Fig. 1
Source data image.
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Source data image.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Source data image.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Source data image.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Source data image.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Source data image.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 7
Source data image.
Source Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 1
Source data image.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 3
Source data image.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 5
Source data image.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 6
Source data image.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 7
Source data image.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vanderheiden, A., Hill, J.D., Jiang, X. et al. Vaccination reduces central nervous system IL-1β and memory deficits after COVID-19 in mice. Nat Immunol 25, 1158–1171 (2024). https://doi.org/10.1038/s41590-024-01868-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41590-024-01868-z
This article is cited by
-
The dichotomic role of cytokines in aging
Biogerontology (2025)
-
A novel PLpro inhibitor improves outcomes in a pre-clinical model of long COVID
Nature Communications (2025)