Abstract
In this study, we evaluated the quality of life (QoL) and associated factors of community health workers (CHWs) in different urban settings as a contributor to the preparedness of Brazilian primary care for future sanitary emergencies. The sample included 1935 CHWs from 4 state capitals and 4 inland municipalities in northeastern Brazil. Information was collected on QoL (WHOQOL-BREF), work routines, sociodemographics, direct and indirect exposure to violence, general self-efficacy, social support (MSPSS), mental health (SRQ-20) and coronavirus anxiety. The data were subjected to multiple linear regression analysis (α = 5%). In the state capitals, the factors associated with loss of QoL were poor mental health, lack of training, uncertainty about occupational biosafety, and lack of adaptation of services to tend to patients diagnosed with COVID-19. Among the inland municipalities, the main factors were coronavirus anxiety, poor mental health, lack of adaptation of services, lack of training, and lack of personal protective equipment (PPE). A high MSPSS (family and friends) score and self-efficacy had positive impacts on QoL in both urban settings. Our results highlight the need for investment in permanent education, PPE, social support, and mental health care for CHWs.
Similar content being viewed by others
Introduction
The Brazilian Unified National Health System (SUS) represents a significant public health policy, structured on the primary health care (PHC) model and implemented, at the local level, by the Family Health Strategy (FHS), which provides multiprofessional care1. PHC played an important role in the Brazilian response to COVID-19, which required timely readjustments to the care provided by public health care teams (ESFs), including changes in protocols, patient flow and work routines2.
FHS is the primary strategy for consolidating and expanding PHC within Brazil. It includes the implementation of democratic and participatory health care and management practices through multidisciplinary teams covering defined populations and territories. In addition, the FHS considers each human being according to their singularity and socio-cultural context in a quest for comprehensive care3. The FHS multiprofessional team is comprised of a doctor, a nurse, a dentist, health auxiliaries and community health workers (CHWs), who are trained community members that reside and work within the territory served by the FHS, so they are familiar with the context of people's lives, which greatly strengthens the bonds between the community and the Primary Health Care (PHC) teams. CHWs primarily engage in providing guidance and support for their team’s health professionals and conducting health promotion activities and home visits to assist and collect information on the health and living standards of families. Their community presence facilitates residents’ access to health services and strengthens the bond between families and the FHS4.
The incidence of urban violence has increased markedly in various regions of the world, including Northeast Brazil. Among the 50 most violent cities in the world in 2023, there are ten Brazilian northeast municipalities, including six of the nine state capitals5, three of which were researched in the present article. The high level of community violence and low social indicators (e.g., high illiteracy, low urban development index and high percentage of the population living in poverty) in the Northeast denote the vulnerable daily reality of this region6. Furthermore, this vulnerability scenario was worsened by COVID-19. In the first year of the Covid-19 pandemic, this region, which accounts for 27% of the Brazilian population, recorded a third of the cases (34%) and deaths (32%) of COVID-19, demonstrating the great impact of the pandemic in the Brazilian northeast7.
It has been demonstrated that violence, the Covid-19 pandemic, and other stressors are associated with the process of CHW work and mental health4,8,9,10,11. Nevertheless, not much is known on the CHWs quality of life on this stressed context.
The work setting of CHWs has changed drastically as long-standing social, environmental and cultural dynamics have been reshaped by new circumstances associated with lockdown restrictions, a lack of information about the manifestations of the disease, increased mortality, and a loss of quality of life (QoL) for the population at large and for health professionals in particular12,13.
The changes in work routines brought about by sanitary emergencies affected CHWs’ personal and professional lives and quality of life due to a complex constellation of sociodemographic, economic, environmental, cultural and health factors, with all their subjectivities and intersubjectivities. Quality of life may be defined in many ways. According to the World Health Organization (WHO), 'Quality of Life' refers to an individual's perception of their position in life, considering their socioeconomic context, habits, customs, values, goals, expectations, and concerns14.
QoL can be assessed in different ways and with different tools, one of which is the WHOQOL-BREF15, developed and recommended by the World Health Organization (WHO). Frontline health professionals are particularly prone to a decrease in QoL due to anxiety, depression and burnout, aggravated by factors of social unrest and violence in the territory4,16.
The availability of social support for health workers in terms of instrumental and emotional factors and social interaction has been shown to preserve QoL in both the occupational setting and the family setting17,18,19, which has become increasingly evident during recent pandemics20,21. Studies published before the pandemic identified sex, age, schooling, workplace, family income, smoking, psychological aspects and satisfaction as determinants of QoL22.
Despite a number of similar actions and measures taken in the early days of the pandemic, the response to health emergencies varied among municipalities according to local socioeconomic, demographic, epidemiological, social and political factors and the capacity and resilience of the public health care infrastructure7,23,24.
It is important to investigate to what extent the CHWs’ QoL was affected during this period, taking into account the context of violence in the territories and the sociodemographic and economic situation of each municipality. A discussion on this issue can contribute new knowledge and help create interventions for the promotion of QoL among CHWs, identify vulnerable groups, design health care policies and plan actions. In addition, the research conducted during the pandemic and the questions raised are important aids in preparing CHWs for future health emergencies.
The purpose of this study was to assess the QoL of CHWs from Northeast Brazilian state capitals and inland municipalities, as well as factors related to mental health, socioeconomic variables and the primary care setting.
Methods
This was a cross-sectional, multicenter study based on information collected in four Brazilian state capitals (Fortaleza/Ceará, João Pessoa/Paraíba, Recife/Pernambuco, Teresina/Piauí) and four inland municipalities in the state of Ceará (Crato, Juazeiro do Norte, Barbalha, Sobral) between April and August 2021. The sampling locations were chosen to obtain a representative picture of the factors associated with CHW QoL in both central and inland urban settings. The Northeast is a region with high social vulnerability and political, economic, territorial inequalities and has been one of the worst affected by the pandemic7. Primary health care coverage in the municipalities studied ranges from 58.12% (Recife) to 100% (Sobral)25; the population from 59 thousand (Barbalha) to 2.4 million (Fortaleza)26 and the HDI of 0.683 (Barbalha) to 0.772 (Recife)27.
In 2020, according to the Health Ministry’s e-management system, the eight sampled cities employed a total of 7909 CHWs28. Using a simple sample calculation based on the number of CHWs in each municipality, a sample error of 5%, a 95% confidence level, and a homogeneous distribution (80/20) of the sampled population, we arrived at a minimum sample size of 1879 CHWs. However, the actual number of CHWs interviewed for the study (n = 1935) exceeded this number.
To be eligible, CHWs had to be active members of ESF teams during the study period and have at least one year of experience as CHWs. Participation was spontaneous upon invitation. CHWs on leave or vacation were excluded.
To standardize the data collection procedure, the collectors were trained using a manual prepared for the purpose. The training started with the theoretical aspects of each stage. Due to the sanitary conditions under which the study was conducted, we employed the biosafety protocols established in the GVIMS/GGTES/ANVISA directive 04/2020 in addition to complying with the standard ethical requirements of research involving human subjects.
The self-reporting questionnaire (SRQ-20) collected information on sociodemographics, work, psycho-emotional symptoms, experience with COVID-19, general self-efficacy (GSE), multidimensional perceived social support (MSPSS), coronavirus anxiety, exposure to violence in territories, work issues in territories, and the WHOQOL-BREF (dependent variable).
The WHOQOL-BREF is widely used to assess QoL and contains 26 items covering 4 domains: physical health, psychological health, social relationships, and the environment. Each item is scored on a Likert scale, with higher scores indicating a better QoL29,30.
Focusing on psychoemotional symptoms, the SRQ-20 has been extensively used in Brazilian studies to measure indicators of common mental disorders (CMDs), especially in occupational settings, and is an important mental health screening tool that uses ≥ 7 as the cutoff31. Ranging from 0 to 20, the SRQ score corresponds to the number of affirmative answers to 20 dichotomous questions. The instrument has been validated for Brazil32.
The Coronavirus Anxiety Scale (COVID-19) is used to assess anxiety induced by concerns about COVID-1933, with higher scores indicating greater anxiety. The instrument features five questions scored on a scale from 0 to 4, ranging from 0 to 20.
The MSPSS was introduced by Zimet et al.34 and has been validated for Brazilian Portuguese35. It is based on the perception that people in one’s social sphere provide affective and material resources, a sense of belonging, and a supportive network36,37. Social support can alleviate distress during times of uncertainty, crisis, anxiety and tension38. The instrument features 12 items, covering three factors (family, friends and significant others which look at the presence of a special person in time of need as a source of comfort, to share joys and sorrows, and care about feelings)39, and is scored using a Likert scale36.
The collected data were analyzed using the statistical software R, with the level of significance set at 5% (p < 0.05). The outcome variable was QoL, expressed as the total WHOQOL-BREF score. In addition, multiple linear regression analysis with backward elimination was performed using Akaike’s information criterion due to the exploratory nature of the model. As with the correlation analyses, the data from the state capitals and the inland municipalities were analyzed separately.
All the participating CHWs provided informed written consent. Filed under #4.587.955, the study protocol was approved by the Internal Review Board of Ceará State University (UECE).
Ethics approval and consent to participate
This research was approved by the Research Ethics Committee of Ceará State University (UECE) (authorization #4.587.955). Written informed consent was obtained from all the participants in the study. All procedures were performed in accordance with relevant guidelines.
Results
The total sample consisted of 1935 CHWs, with a predominance of females (82.76%). The average age was 46 years (range: 23–72). Most had children (80.98%), but no spouse or partner (58.21%) was identified as Catholic (65.85%), and most were indigenous/brown (71.84%). Nearly half (47.26%) had completed high school and earned up to 2 minimum wages (at the time of writing, 1 minimum wage was equivalent to USD ~ 260). Table 1 shows the statistical analysis of the sociodemographic variables.
On average, the respondents engaged in 4.78 ± 1.41 types of activities (range: 0–6) and made 4.77 ± 1.16 types of home visits (range: 0–6). Most (77.91%) were frontline workers during the lockdown, despite not being trained for this type of work (83.96%). Slightly more than half (54.58%) reported having insufficient access to personal protective equipment (PPE), and 66.7% of the participants reported having insufficient biosafety norms in the workplace. Almost all (96.98%) believed they were susceptible to COVID-19 in the workplace (Table 2).
According to three quarters of the respondents (75.7%), the service was adapted to patients diagnosed with COVID-19, but 62.1% reported not having increased their workload. Moreover, almost all (94.46%) considered themselves potential vectors of coronavirus, 74% had one relative diagnosed with COVID-19, and 40.41% had themselves been diagnosed. The work processes changed during the pandemic according to 79.43% of the CHWs in the state capital and 77.26% of the CHWs in inland municipalities (Table 2).
Table 3 shows the variables related to the perception of violence, coronavirus anxiety, mental health, social support and QoL. Note that social relationships and support were positively associated with QoL in both state capitals (77%) and inland municipalities (74%).
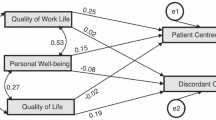
The QoL of CHWs in state capitals was negatively influenced by low SRQ-20 scores, lack of training to care for patients diagnosed with COVID-19, perception of insufficient biosafety norms, and lack of adaptation of services to care for patients diagnosed with COVID-19. On the other hand, high MSPSS (family and friends) and high GSE were positively associated with QoL (Table 4).
The QoL of CHWs in inland municipalities was negatively influenced by coronavirus anxiety, low SQR-20 scores, lack of training to care for patients diagnosed with COVID-19, lack of access to PPE, and lack of adaptation of services to care for patients diagnosed with COVID-19. On the other hand, high MSPSS (family and friends), high GSE, completed elementary school, and an income > 4 times the minimum wage were positively associated with QoL (Table 5).
Discussion
In this study, we evaluated how the QoL of Brazilian CHWs was impacted by adverse working conditions during the pandemic in different contexts and territories (four northeastern state capitals and four inland municipalities). Our findings can foster debates on how to better prepare health care services and make systems more resilient to future social and sanitary challenges. In health care, resilience is defined as the ability of health workers, administrators, institutions and communities to maintain essential services while running during times of adversity and reorganize structures and services based on lessons learned during crises40.
The predominance of the female sex in the field work force matches the findings of other studies41,42. However, it should be noted that many workers also tend to have their homes and families, and the burden and stress associated with multiple functions and insufficient rest can take their toll on health43. It is important to emphasize the multiple roles culturally assumed by the female universe, as mother, daughter, partner, which, in the face of the risk of transmissibility, have aggravated the burden due to the necessary behavioral changes both in the work environment and in the family. This may be exacerbated by the prevailing culture, according to which women are assumed to be more aware/sensitive to the needs of others44 and thus under more pressure to be the source of care, which in turn may affect their quality of life. In terms of gender inequalities affecting quality of life, UN Women Brazil concluded that the pandemic has worsened living and working conditions and increased cases of gender-based violence against women and girls45.
In this study, social support (family and friends) and general self-efficacy were associated with better QoL in both scenarios (state capitals and inland municipalities). In another study, family support was found to favor self-efficacy with regard to the control and prevention of diabetes and asthma episodes46,47. Whether in crisis or not, human behavior is modulated by the meaning individuals assign to their interactions with others, themselves and the social environment15.
Family and friends had a greater positive impact than ‘significant others’, which is consistent with the findings of other researchers20,21,31,48 and indicates the potential of these networks as a source of social support for CHWs. Thus, strategies favoring and expanding social support should be implemented, among other things, by creating space for the exchange of experiences, improving working conditions, implementing occupational health actions through psychosocial support programs, and strengthening collaboration and teamwork skills49. Such initiatives are likely to mitigate the negative effects of sanitary emergencies on CHWs’ mental health and QoL.
Social support reinforces CHWs’ perceptions of belonging, acceptance, appreciation, care and love—a feeling crucial in times of increased stress, crisis and peril20,37. The restrictions imposed during the recent lockdown heavily affected family and social relationships and led to significant changes in health work routines. In such situations, social support networks contribute to preserving QoL.
The data collected from the state capitals show that a lack of adaptation of services to care for patients diagnosed with COVID-19 and lack of adequate training led to a loss of QoL in this setting. In the inland municipalities, lack of training, lack of adaptation of services, and unavailability of PPE also negatively impacted QoL.
The measures carried out to combat Covid-19 varied among the eight sampling locations due to differences in sociodemographic, economic and cultural profiles; the capacity of each local health care infrastructure; and the availability of resources and personnel. However, a set of commonalities was observed, especially with regard to the resilience of the local health care system. Professional insecurity resulting from living with urban violence implies deficits in the development of actions outside the health unit (such as home visits and educational activities) and possible suspension/termination of consultations within teams50,51,52, aggravating the relationship with the community and could have also affected professionals’ QofL.
Our results showed that the working conditions of the CHWs in both state capitals and inland municipalities were unsatisfactory during the health emergency. In the same period, the public health care sector was marred by administrative difficulties and protracted political conflicts, with potentially serious repercussions on morbidity and mortality rates7,23,53. The health work process has been greatly compromised, the responses to the challenges imposed by covid-19 have been heterogeneous, which has had repercussions on the quality of life of health professionals54,55. A study showed that in Brazil, doctors (69.5 per cent) and nursing staff (64.1 per cent) and community health workers and endemic control workers (34.1 per cent) received personal protective equipment (PPE) continuously during the pandemic56.
In Brazil, local health authorities, rather than the federal government, managed the response to the pandemic. Immediate safety measures and new processes had to be devised to address unusual disease patterns and deaths. In several studies, health professionals have reported receiving insufficient training and information7,23,56,57. In the absence of a unified national response, problems at the municipal level often delay the implementation of effective health actions.
Uncertainty about the new work procedures required during sanitary emergencies had a negative effect on the QoL of the CHWs. This experience is important to keep in mind when designing new local interventions and public policies that incorporate the demands and needs of CHWs. Moreover, the QoL of other Brazilian health care workers, such as nurses, was equally affected during this period20,58,59.
The capacity of the public secondary and tertiary-level health care infrastructure was highly taxed, sometimes overburdened, during this period. Control measures at the primary care level and the occupational safety of the CHWs were not part of the initial action plan. This is reflected in a review60 of public health care measures covering the period 2019–2020: the twenty most relevant topics included health workers’ mental health (5th place), health worker and patient safety (9th place), and training/distance learning (10th place). Primary care was not included among the twenty topics.
The workload of CHWs in territories, employing their know-how and experience to bridge the gap between the community and the health care system, escalated during lockdown, affecting their QoL and increasing their risk of developing CMDs. This harmful effect was to some degree felt in society as a whole as the inevitable result of the sanitary emergency, fear of exposure to a novel illness, and the flow of reports of increased mortality20.
Health workers are exposed to various types of violence, including living with, interacting with, and witnessing situations of violence in the area, through direct or indirect contact with victims of violence or aggressors61. Faced with this scenario, CHWs are the most exposed professionals, since they directly perform functions outside the health unit, such as home visits and active searches, and are vulnerable to threats during the community approach61,62,63,64. CHWs represent the health facility and, hence, the State. Nevertheless, they are also under pressure from a local parallel power, with unknown rules. Thus, the daily activities of CHWs occur in a territory under a precarious balance between the power of the State and the power of local gangs65 where CHWs are most inhibited in territories where the State has less control and where health challenges are particularly severe9. The consequences of victimization in the workplace include psychosomatic symptoms and can manifest themselves in the form of feelings of distrust, discouragement, loss of meaning in work, stress, anxiety, isolation, low self-esteem, among others66, which tend to worsen over time, which can lead to disruption of interpersonal relationships, absenteeism, turnover, illness, absenteeism, disruption of work organization67 and possibly professional quality of life. Thus, the importance to evaluate quality of life of CHW on the context of stressors, such as urban violence and Covid-19.
The lessons learned during this period will help strengthen the public health care system and improve the management and support of frontline workers. Job burnout has serious implications for health, employee retention and the work environment. Policies are urgently needed to protect the health and QoL of health care workers and, at the same time, to increase the resilience of the health care system.
Methodologically speaking, the present study was limited by its exclusive reliance on self-reported data, which introduced some degree of subjectivity and memory bias in the participants’ responses. Additionally, the cross-sectional study design adopted precluded an analysis of causality.
The effects of the COVID-19 pandemic on the QoL of CHWs require long-term monitoring. Studies on sanitary emergencies have generally paid little attention to primary care workers’ health and occupational safety, but the effects are gradually becoming more perceptible.
Conclusions
The long-term effects of the stressful context of violence and health emergencies on the QoL of CHWs are not yet fully understood and require longitudinal evaluations. Nevertheless, the decrease in QoL of Brazilian frontline CHWs associated with health emergencies identified in the present study has highlighted the need to improve working conditions and procedures. Respondents reported high levels of CMDs, which were mitigated by social support outside the workplace. The health, well-being, and quality of life of CHWs are essential to their role as a link between the community and the health system, and to making the health system more resilient and efficient.
The health crisis has sparked a social emergency, prompting significant shifts in the professional landscape that have impacted workers across all levels of care, affecting their quality of life. This impact has been particularly evident in Primary Health Care (PHC), which stands as the frontline of community care. The post-traumatic effects experienced by workers, stemming from societal pressures, underscore the critical need to address two key aspects of workers' well-being within the PHC setting.
Firstly, there's a clear imperative to establish and maintain a psychosocial support service tailored to the needs of PHC workers within their workplace. Secondly, it's essential to bolster social interactions within interprofessional teams through dialogic and participatory communication among team members and the community. This approach is vital for fostering a supportive environment and ultimately enhancing the quality of life for the PHC workforce.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Castro, M. C. et al. Brazil’s unified health system: The first 30 years and prospects for the future. Lancet 394(10195), 345–356 (2019).
Alonso, C. M. C., Béguin, P. D. & Duarte, F. J. C. M. Trabalho dos agentes comunitários de saúde na Estratégia Saúde da Família: metassíntese. Rev. Saúde Pública 52, 14 (2018).
Ministério da Saúde. Portaria no 2.436, de 21 de setembro de 2017. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes para a organização da atenção básica, no âmbito do Sistema Único de Saúde (SUS). Diário Oficial da União 2017; 22 sep
Vieira-Meyer, A. P. G. F., Morais, A. P. P., Campelo, I. L. B. & Guimarães, J. M. X. Violence and vulnerability of the Community Health Worker in the territory: Implications for tackling COVID-19. Ciênc Saúde Colet 26, 657–668 (2021).
Consejo Ciudadano para la Seguridad Publica y la Justicia Penal; WorldAtlas https://www.worldatlas.com/cities/the-most-dangerous-cities-in-the-world.html#h_34597806750751638029371800
Vilar, D. L. F. & Moreira, A. P. O papel do Programa Bolsa Família na desigualdade de renda na região Nordeste do Brasil. Informe Econômico (UFPI) 44(1), 93–110 (2022).
Kerr, L. et al. COVID-19 no Nordeste brasileiro: sucessos e limitações nas respostas dos governos dos estados. Cien. Saude Colet. 25, 4099–4120 (2020).
Almeida, J. F., Peres, M. F. T., Tourinho, M. F. & Fonseca, T. L. A violência no território e a construção de vínculos entre os agentes comunitários de saúde e os usuários em um serviço de atenção primária. Rev. Epos. 7(1), 92–109 (2016).
Almeida, J. F., Peres, M. F. T. & Fonseca, T. L. O território e as implicações da violência urbana no processo de trabalho dos agentes comunitários de saúde em uma unidade básica. Saude Soc. 28(1), 207–221. https://doi.org/10.1590/S0104-12902019170543 (2019).
Vieira-Meyer, A. P. G. F. et al. Gender and violence in the daily routine of community health workers in Fortaleza, Brazil. J. Community Health 48, 810–818. https://doi.org/10.1007/s10900-023-01221-9 (2023).
Vieira-Meyer, A. P. G. F. et al. Readiness of Community Health Agents for COVID19. Eur. J. Public Health 32, iii221 (2022).
Nussbaumer-Streit, B. et al. Quarantine alone or in combination with other public health measures to control COVID19: A rapid review. Cochrane Database Syst. Rev. 2020, CD013574 (2020).
Holt-Lunstad, J., Birmingham, W. & Jones, B. Q. Is there something unique about marriage? the relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Ann. Behav. Med. 35, 239–244 (2008).
The WHOQOL Group. The World Health Orga nization quality of life assessment (WHOQOL): po sition paper from the World Health Organization. Soc. Sci. Med. 10, 1403–1409 (1995).
Fleck, M. P. et al. Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida “WHOQOL-bref”. Rev. Saúde Pública 34(2), 178–183. https://doi.org/10.1590/S0034-89102000000200012 (2000).
Cremonese, G. R., Motta, R. F. & Traesel, E. S. Implicações do trabalho na saúde mental dos Agentes Comunitários de Saúde. Cad Psicol. Soc. Trabalho 16(2), 279–293 (2013).
Cassel, J. The contribution of the social environment to host resistance: The fourth Wade Hampton Frost Lecture. Am. J. Epidemiol. 104(2), 107–123 (1976).
Kaplan, B. H., Cassel, J. C. & Gore, S. Social support and health. Med. Care 15(5), 47–58 (1977).
Kelly, M. E. et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Syst. Rev. J. 6(259), 5–18 (2017).
Souza, R. F. et al. Repercussões dos fatores associados à qualidade de vida em enfermeiras de unidades de terapia intensiva. Rev. Salud Publica 20(4), 453–459 (2018).
Rocha, M. A. M., Carvalho, F. M. & Lins-Kusterer, L. E. F. Qualidade de vida relacionada à saúde de profissionais de enfermagem na Bahia na pandemia da COVID-19. Esc. Anna Nery 26(5), e20210467 (2022).
Mascarenhas, C. H. M., Prado, F. O. & Fernandes, M. H. Fatores associados à qualidade de vida de Agentes Comunitários de Saúde. Ciênc saúde coletiva 18(5), 1375–1386. https://doi.org/10.1590/S1413-81232013000500023 (2013).
Tasca, R. et al. Gerenciando o SUS no nível municipal ante a Covid-19: uma análise preliminar. Saúde Debate 46(spe1), 15–32. https://doi.org/10.1590/0103-11042022E101 (2022).
Fernandez, M., Lotta, G. & Corrêa, M. Desafios para a Atenção Primária à Saúde no Brasil: uma análise do trabalho das agentes comunitárias de saúde durante a pandemia de COVID-19. Trabalho Educação Saúde 19, e00321153. https://doi.org/10.1590/1981-7746-sol00321 (2021).
BRASIL. Cobertura da atenção básica. Disponível em https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relCoberturaAPSCadastro.xhtml acesso em 13 de maio 2024
PNUD. Programa das Nações Unidas para o Desenvolvimento. Atlas do Desenvolvimento Humano no Brasil 2013. Brasília: PNUD, Ipea, FJP, 2013. Disponível em: https://www.undp.org/pt/brazil/idhm-municipios-2010. Available in: 21 nov. 2023.
IBGE. Instituto Brasileiro de Geografia e Estatística. Censo Demográfico 2022. Rio de Janeiro: IBGE, 2022. Disponível em: https://censo2022.ibge.gov.br/panorama/. Acesso em: 25 jan. 2024.
Brasil. Ministério da Saúde. Secretaria de Atenção Primária à Saúde. e-SUS Atenção Primária. Brasília, 2020a. [Acessado 14 Set 2022]. Available in: https://aps.saude.gov.br/ape/esus
World Health Organization. Division of Mental Health and Prevention of Substance Abuse. (1997). WHOQOL: measuring quality of life. World Health Organization. [Acessado 24 Mai 2023]. Available in: https://apps.who.int/iris/handle/10665/63482
Almeida-Brasil, C. C. et al. Qualidade de vida e características associadas: aplicação do WHOQOL-BREF no contexto da Atenção Primária à Saúde. Ciênc Saúde Coletiva 22(5), 1705–1716. https://doi.org/10.1590/1413-81232017225.20362015 (2017).
Barreto do Carmo, M. B. et al. Screening for common mental disorders using the SRQ-20 in Brazil: what are the alternative strategies for analysis?. Rev. Bras. Psiquiatr. 40(2), 115–122. https://doi.org/10.1590/1516-4446-2016-2139 (2018).
Santos, K. et al. Avaliação de um instrumento de mensuração de morbidade psíquica: estudo de validação do self-reporting questionnaire (SRQ-20). Rev. Baiana de Saúde Pública 34(3), 54 (2011).
Lee, S. A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 44(7), 393–401. https://doi.org/10.1080/07481187.2020.1748481 (2020).
Zimet, G. D., Dahlem, N., Zimet, S. & Farley, G. The multidimensional scale of perceived social support. J. Pers. Assess. 52(1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2 (1988).
Cardoso, H. F. & Baptista, M. N. Escala de Percepção de Suporte Social (versão adulta)—EPSUS-A: Estudo das qualidades psicométricas. Psico-USF 19(3), 499–510. https://doi.org/10.1590/1413-82712014019003012 (2014).
Gabardo-Martins, L. M. D., Ferreira, M. C. & Valentini, F. Propriedades psicométricas da escala multidimensional de suporte social percebido. Temas Psicol 25(4), 1873–1883 (2017).
Okun, M. A. & Lockwood, C. M. Does level of assessment moderate the relation between social support and social negativity? A meta-analysis. Basic Appl. Soc. Psychol. 25(1), 15–35. https://doi.org/10.1207/S15324834BASP2501_2 (2003).
Lobburi, P. The influence of organizational and social support on turnover intention in collectivist contexts. J. Appl. Bus. Res. 28(1), 93–104. https://doi.org/10.19030/jabr.v28i1.6687 (2012).
Brugnoli, A. V. M., Gonçalves, T. R., Silva, R. C. D. & Pattussi, M. P. Evidence of the validity of the Multidimensional Scale of Perceived Social Support (MSPSS) in university students. Ciênc. Saúde Colet. 27(11), 4223–4232 (2022).
Kruk, M. E. et al. Building resilient health systems: A proposal for a resilience index. BMJ 357(8109), 1–8 (2017).
Wermelinger, M. et al. A feminilização do mercado de trabalho em saúde no Brasil. Divulg. Saúde Debate 45, 54–70 (2010).
Durão, A. V. R. et al. Qualificação e gênero no trabalho das Agentes Comunitárias de Saúde. In Trabalhadores técnicos em saúde: aspectos da qualificação profissional no SUS (eds Morosini, M. V. G. C. et al.) 421–446 (EPSJV, Rio de Janeiro, 2013).
Barbosa, R. H. S., Menezes, C. A. F., David, H. M. S. L. & Bornstein, V. J. Gênero e trabalho em Saúde: um olhar crítico sobre o trabalho de agentes comunitárias/os de Saúde. Interface (Botucatu) 16(42), 751–765. https://doi.org/10.1590/S1414-32832012000300013 (2012).
Angelo, M. Cultura e cuidado da família. In Antropologia para enfermagem (eds Nakamura, E. et al.) (Manole, São Paulo, 2009).
ONU Mulheres Brasil. Violência contra mulheres e meninas é pandemia invisível, afirma diretora executiva da ONU Mulheres. Brasília (DF): ONU Mulheres Brasil (2020). Available in: https://www.onumulheres.org.br/noticias/violencia-contra-as-mulheres-e-meninas-e-pandemia-invisivelafirma-diretora-executiva-da-onu-mulheres/
Lima, K. F. et al. Educational technology for promoting parental self-efficacy in controlling childhood asthma. Rev. Rene 23, e71588. https://doi.org/10.15253/2175-6783.20222371588 (2022).
Lima, C. R., Menezes, I. H. C. F. & Peixoto, M. R. G. Educação em saúde: avaliação de intervenção educativa com pacientes diabéticos, baseada na teoria social cognitiva. Ciênc. Educ. 24(1), 141–215 (2018).
Vidotti, V., Martins, J. T., Galdino, M. J. Q., Ribeiro, R. P. & Robazzi, M. L. C. C. Burnout syndrome, occupational stress and quality of life among nursing workers. Enferm. Glob. 18(3), 344–376. https://doi.org/10.6018/eglobal.18.3.325961 (2019).
Ekbäck, M., Benzein, E., Lindberg, M. & Årestedt, K. The Swedish version of the multidimensional scale of perceived social support (MSPSS)—A psychometric evaluation study in women with hirsutism and nursing students. Health Qual. Life Outcomes 11, 16 (2013).
Leite, C. N. et al. Violência na Estratégia de Saúde da Família: riscos para a saúde dos trabalhadores e ao atendimento. Rev. Enferm. UERJ 28(1), e45789–e45789 (2020).
Machado, C. B. et al. Violência urbana e repercussão nas práticas de cuidado no território da saúde da família. Rev. Enferm. UERJ 24(5), e25458–e25458 (2016).
Machado, C. B. & Daher, D. V. Violência urbana: Repercussões e consequências na assistência à saúde em uma Unidade de Saúde da Família. Ciência Cuidado e Saúde Maringá 14(4), 1445–1452 (2015).
Costa, A. M., Rizzotto, M. L. F. & Lobato, L. V. C. Fome, desemprego, corrupção e mortes evitáveis: Faces da necropolítica. Saúde Debate 45(130), 555–558. https://doi.org/10.1590/0103-1104202113000 (2021).
Aulanko, I. et al. Working conditions during the COVID-19 pandemic in primary and tertiary healthcare: A comparative cross-sectional study. Int. J. Occup. Med. Environ. Health 36(1), 139–150. https://doi.org/10.13075/ijomeh.1896.01944 (2023).
Skagerström, J., Fernemark, H., Nilsen, P., Seing, I., Hårdstedt, M., Karlsson, E. et al. Challenges of primary health care leadership during the COVID-19 pandemic in Sweden: a qualitative study of managers' experiences. Leadersh Health Serv (Bradf Engl). 2023(ahead-of-print):389–401. Available in: https://doi.org/10.1108/LHS-08-2022-0089
Machado, A. V. et al. COVID-19 and health systems in Brazil and around the world: effects on the working conditions and health of health workers. Ciência & Saúde Coletiva 28(10), 2965–2978 (2023).
Giovanella, L. et al. Denial, disdain and deaths: notes on the criminal activity of the federal government in fighting Covid-19 in Brazil. Saúde debate 44, 895–901 (2020).
Paula, J. J. et al. Quality of life of health care professionals in pandemic times. Clin. Neuropsychiatry 18(3), 113–118 (2021).
Caliari, J. S. et al. Quality of life of nurse practitioners during the COVID-19 pandemic. Rev. Bras. Enferm. 75(Suppl 1), e20201382 (2021).
United Nations (UN). Policy brief: COVID-19 and the need for actions on mental health. May 13, 2020. [Acessado 10 Jun 2022]. Available in: https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf
Lancman, S. et al. Repercussões da violência na saúde mental de trabalhadores do Programa Saúde da Família. Rev Saúde Pública 43(4), 682–688 (2009).
Flórido, H. G. et al. Gerenciamento das situações de violência no trabalho na estratégia de saúde da família pelo enfermeiro. Texto Contexto-Enferm. 29, e20180432 (2020).
Almeida, J. F., Peres, M. F. T. & Fonseca, T. L. O território e as implicações da violência urbana no processo de trabalho dos agentes comunitários de saúde em uma unidade básica. Saúde Soc. 28(1), 207–221 (2019).
Vieira-Meyer, A. P. G. F. et al. Violência no território e saúde mental de agentes comunitários de saúde em uma metrópole brasileira. Cad. Saúde Pública 38(12), e00022122 (2022).
Velloso, I. S. C., Araujo, M. T., Rocha, A. D. M. & Alves, M. A visão dos profissionais de saúde sobre a violência no cotidiano de trabalho em uma unidade básica. Rev. Min. Enferm. 9(4), 302–308 (2005).
Trindade, L. L. et al. Agressão verbal contra profissionais de saúde da atenção primária e terciária: estudo de métodos mistos. Rev. Enferm. UFSM 12(15), 1–17 (2022).
Olímpio, A. C. S. et al. Violência ocupacional na atenção primária e as interfaces com as condições e a organização do trabalho. Sanare Revista De Polít. Públicas 20(2), 97–106. https://doi.org/10.36925/sanare.v20i2.1559 (2021).
Acknowledgements
We want to express our gratitude to all the community health workers.
Funding
The research from which this manuscript is derived received financial support from the Lemann Foundation (University of Harvard), Fundação Oswaldo Cruz (Fiocruz) Programa de Políticas Públicas, Modelos de Atenção e Gestão do Sistema e Serviços de Saúde (PMA) and the Research Foundation of the State of Ceara (Funcap).
Author information
Authors and Affiliations
Contributions
F.D.S.F. Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing. S.F.F. Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing. N.F.C.V. Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing. I.L.B.C. Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing. M.C. was involved in the data analyses and the definition of intellectual content and reviewed the manuscript. A.K.Y. Involved in the data analyses and definition of intellectual content and reviewed the manuscript. All the authors approved the version to be published and agreed to be accountable for all the aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. A.P.G.F.V.M. Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; writing—original draft; writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Forte, F.D.S., Vieira, N.F.C., Farias, S.F. et al. Quality of life and associated factors for community health workers in the context of the COVID-19 pandemic in northeastern Brazil. Sci Rep 14, 13312 (2024). https://doi.org/10.1038/s41598-024-63828-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-63828-9