Abstract
Background
This study aimed to quantify fatigue, dyspnea, and physical activity and identify associated factors in children and adolescents with postacute COVID-19 syndrome.
Methods
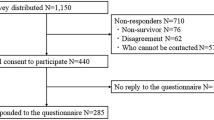
A prospective cohort study included 74 participants aged 6–18 years with postacute COVID-19 symptoms and 120 age- and sex-matched controls without SARS-CoV-2 antibodies. Participants completed questionnaires assessing fatigue, dyspnea, and physical activity and underwent pulmonary function tests.
Results
Children with postacute COVID-19 syndrome reported significantly greater fatigue (parent-rated scores: mean 67.9 vs. 82.4, p < 0.001; child-rated scores: 73.7 vs. 83.0, p < 0.001), increased dyspnea (mMRC grades 3–4: 10.9% vs. 4.1%, p = 0.001), and lower physical activity (median 787.8 vs. 1658.5 MET*min/week, p < 0.001) than controls. They also had a higher prevalence of mixed (8.1% vs. 1.7%, p = 0.029) and restrictive lung disease (29.7% vs. 10.8%, p = 0.001). Older age and COVID-19 were identified as risk factors for fatigue and reduced activity. Fatigue correlated with reduced physical activity but not with pulmonary function.
Conclusion
Children and adolescents with postacute COVID-19 syndrome, particularly older individuals, experience greater fatigue and reduced physical activity than controls. These findings highlight the importance of quantifying postacute COVID-19 symptoms and their associations with physiological assessments.
Impact
-
This prospective, age- and sex-matched cohort study revealed that children and adolescents with postacute COVID-19 syndrome perceived higher fatigue levels, had higher dyspnea scores, had a greater prevalence of mixed lung and restrictive lung disease, and exhibited less physical activity than their control counterparts.
-
Fatigue correlated with reduced physical activity but was not consistently correlated with pulmonary function test results.
-
This study highlights the importance of quantifying postacute COVID-19 symptoms and exploring the associations between individual symptoms and the impact of coronavirus infection on various systems, including the neurological, musculoskeletal, cardiopulmonary, and immune systems.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data supporting this study’s findings are available in the supplementary file (PostAcuteCOVID data.cvs).
References
Wilde, H. et al. Hospital admissions linked to SARS-CoV-2 infection in children and adolescents: cohort study of 3.2 million first ascertained infections in England. BMJ 382, e073639 (2023).
Antoon, J. W. et al. COVID-19 and acute neurologic complications in children. Pediatrics 150, e2022058167 (2022).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27, 601–615 (2021).
Funk, A. L. et al. Post-COVID-19 conditions among children 90 days after SARS-CoV-2 infection. JAMA Netw. Open 5, e2223253 (2022).
Haddad, A. et al. Long COVID symptoms in exposed and infected children, adolescents and their parents one year after SARS-CoV-2 infection: A prospective observational cohort study. EBioMedicine 84, 104245 (2022).
Sansone, F. et al. Long COVID in children: A multidisciplinary review. Diagnostics (Basel) 13, 1990 (2023).
Stephenson, T. et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): a national matched cohort study. Lancet Child. Adolesc. Health 6, 230–239 (2022).
Kikkenborg Berg, S. et al. Long COVID symptoms in SARS-CoV-2-positive adolescents and matched controls (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child. Adolesc. Health 6, 240–248 (2022).
Lopez-Leon, S. et al. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci. Rep. 12, 9950 (2022).
Ho, H. L. et al. Seroprevalence of COVID-19 in Taiwan revealed by testing anti-SARS-CoV-2 serological antibodies on 14,765 hospital patients. Lancet Reg. Health-W. Pac. 3, 100041 (2020).
Chiang, Y. C., Hinds, P. S., Yeh, C. H. & Yang, C. P. Development and psychometric testing of a Chinese version of the Fatigue Scale-Children in Taiwan. J. Clin. Nurs. 17, 1201–1210 (2008).
Varni, J. W., Burwinkle, T. M., Katz, E. R., Meeske, K. & Dickinson, P. The PedsQL in pediatric cancer: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module. Cancer 94, 2090–2106 (2002).
Mahler, D. A. & Wells, C. K. Evaluation of clinical methods for rating dyspnea. Chest 93, 580–586 (1988).
Liou, Y. M., Jwo, C. J., Yao, K. G., Chiang, L. C. & Huang, L. H. Selection of appropriate Chinese terms to represent intensity and types of physical activity terms for use in the Taiwan version of IPAQ. J. Nurs. Res. 16, 252–263 (2008).
Bergier, J., Kapka-Skrzypczak, L., Biliński, P., Paprzycki, P. & Wojtyła, A. Physical activity of Polish adolescents and young adults according to IPAQ: a population based study. Ann. Agr. Env. Med. 19, 109–115 (2012).
Graham, B. L. et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 200, e70–e88 (2019).
Chang, S. M. et al. Reference equations for spirometry in healthy Asian children aged 5 to 18 years in Taiwan. World Allergy Organ. J. 12, 100074 (2019).
Stanojevic, S., Wade, A. & Stocks, J. Reference values for lung function: past, present and future. Eur. Resp. J. 36, 12–19 (2010).
Moffett, A. T. et al. Global, race-neutral reference equations and pulmonary function test interpretation. JAMA Netw. Open 6, e2316174 (2023).
Marcotullio, C. et al. Neuropsychological symptoms and quality of life during the COVID-19 Pandemic in children: A survey in a pediatric population in the Abruzzo Region, Italy. Child.-Basel 11, 532 (2024).
Greenham, M. et al. Fatigue following pediatric arterial ischemic stroke: Prevalence and associated factors. Stroke 52, 3286–3295 (2021).
Chuang, H. J., Lin, C. W., Hsiao, M. Y., Wang, T. G. & Liang, H. W. Long COVID and rehabilitation. J. Formos. Med. Assoc. 123(Suppl 1), S61–s69 (2024).
Stephenson, T., Shafran, R. & Ladhani, S. N. Long COVID in children and adolescents. Curr. Opin. Infect. Dis. 35, 461–467 (2022).
Morand, A. et al. Similar patterns of [(18)F]-FDG brain PET hypometabolism in paediatric and adult patients with long COVID: a paediatric case series. Eur. J. Nucl. Med. Mol. Imaging 49, 913–920 (2022).
Serviente, C., Decker, S. T. & Layec, G. From heart to muscle: pathophysiological mechanisms underlying long-term physical sequelae from SARS-CoV-2 infection. J. Appl. Physiol. (1985) 132, 581–592 (2022).
Avittan, H. & Kustovs, D. Cognition and mental health in pediatric patients following COVID-19. Int. J. Environ. Res. Public Health 20, 5061 (2023).
Knoke, L. et al. Pulmonary function and long-term respiratory symptoms in children and adolescents after COVID-19. Front. Pediatr. 10, 851008 (2022).
Öztürk, G. K., Beken, B., Doğan, S. & Akar, H. H. Pulmonary function tests in the follow-up of children with COVID-19. Eur. J. Pediatr. 181, 2839–2847 (2022).
Onay, Z. R. et al. Impact of Long COVID on lung function in children. Medeni. Med. J. 39, 74–84 (2024).
Sansone, F. et al. Lung function assessment in children with Long-Covid syndrome. Pediatr. Pulmonol. 59, 472–481 (2024).
Evans, P. C. et al. Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc. Res. 116, 2177–2184 (2020).
Xu, J. et al. SARS-CoV-2 induces transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respir. Res. 21, 182 (2020).
Buonsenso, D. et al. Clinical characteristics, activity levels and mental health problems in children with long coronavirus disease: a survey of 510 children. Future Microbiol 17, 577–588 (2022).
Li, B. et al. Physical activity and mental health in children and youth during COVID-19: a systematic review and meta-analysis. Child Adolesc. Psychiatry Ment. Health 17, 92 (2023).
WHO. Global Recommendations on Physical Activity for Health. https://www.ncbi.nlm.nih.gov/books/NBK305057/pdf/Bookshelf_NBK305057.pdf (2010).
Morello, R. et al. Risk factors for post-COVID-19 condition (Long Covid) in children: A prospective cohort study. EClinicalMedicine 59, 101961 (2023).
Chen, Y. H. & Fang, C. T. Achieving COVID-19 zero without lockdown, January 2020 to March 2022: The Taiwan model explained. J. Formos. Med. Assoc. 123(Suppl 1), S8–s16 (2024).
Chen, Y. H., Cheuh, Y. N., Chen, C. M. & Kuo, H. W. Epidemiological characteristics of the three waves of COVID-19 epidemic in Taiwan during April 2022 to March 2023. J. Formos. Med. Assoc. 122, 1174–1182 (2023).
Acknowledgements
We would like to express our sincere gratitude and respect to all the staff and patients at the post-COVID multidisciplinary integrated clinics of National Taiwan University Children Hospital for their continuous efforts, technical support, and patience. Without their help, this study could not have been conducted. This study was supported by the National Science and Technology Council (NSTC 111-2321-B-002-017 and NSTC 112-2321-B-002-013) and National Taiwan University Hospital (NTUH 112-W001 and NTUH 113-W001). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
C.W.L., L., Y.C., and S.F.G. contributed to the conception and design of the study, interpretation of the data, drafting of the article, and critical visualization of the article. C.W.L., K.Y.C., Y.C.L., J.H.W., T.Y.Y., C.Y.L., Y.M.L., and Y.C.C. collected and analyzed the data. L.M.H. provided suggestions for improving the manuscript. All authors contributed to and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent statement
This study was approved by the Research Ethics Committee of the National Taiwan University Hospital (202206053RINC). Written informed consent was obtained from all participants or their guardians before study implementation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, CW., Chen, KY., Wu, JH. et al. Postacute COVID-19 fatigue, dyspnea and reduced activity in children and adolescents. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-03897-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-03897-2