Abstract
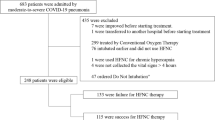
The aim was to identify predictors for early identification of HFNC failure risk in patients with severe community-acquired (CAP) pneumonia or COVID-19. Data from adult critically ill patients admitted with CAP or COVID-19 and the need for ventilatory support were retrospectively analysed. HFNC failure was defined as the need for invasive ventilation or death before intubation. 60 patients with CAP and 185 with COVID-19 were included. 27 (45%) patients with CAP and 69 (37.3%) patients with COVID-19 showed HFNC failure. Lower oxygenation index, lower respiratory oxygenation (ROX) index, and higher respiratory rate at the start of HFNC were significantly associated with HFNC failure. ROC-analysis identified a respiratory rate of 27/min as the optimal cut-off for predicting HFNC failure, with a specificity of 59% and a sensitivity of 75%, and an oxygenation index after HFNC initiation of 99.6 (specificity 81%, sensitivity 74%). In COVID-19, an elevated CRB65-score at hospital admission and at HFNC-initiation was significantly associated with HFNC failure. In CAP and COVID patients an oxygenation index < 99.6, a respiratory rate > 27/min and a ROX index < 4.88 were predictors for HFNC failure whereas a CRB65 score > 3 at hospital admission and > 2 at HFNC start was predictive for HFNC failure in COVID-19.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
References
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S et al (2017) Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 50:1602426
Rochwerg B, Granton D, Wang DX, Helviz Y, Einav S, Frat JP et al (2019) High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med 45:563–572
D’Cruz RF, Hart N, Kaltsakas G (2020) High-flow therapy: physiological effects and clinical applications. Breathe 16:200224
Shih C-C, Liang P-C, Chuang Y-H, Huang Y-J, Lin P-J, Wu C-Y (2020) Effects of high-flow nasal oxygen during prolonged deep sedation on postprocedural atelectasis. Eur J Anaesthesiol 37:1025–1031
Bräunlich J, Mauersberger F, Wirtz H (2018) Effectiveness of nasal highflow in hypercapnic COPD patients is flow and leakage dependent. BMC Pulm Med 18:14
Kang BJ, Koh Y, Lim C-M, Huh JW, Baek S, Han M et al (2015) Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med 41:623–632
Antonelli M, Conti G, Moro ML, Esquinas A, Gonzalez-Diaz G, Confalonieri M et al (2001) Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med 27:1718–1728
Garner O, Dongarwar D, Salihu HM, Barrantes Perez JH, Abraham J, McBride C et al (2021) Predictors of failure of high flow nasal cannula failure in acute hypoxemic respiratory failure due to COVID-19. Respir Med 185:106474
Nicolini A, Piroddi IMG, Barlascini C, Senarega R (2014) Predictors of non-invasive ventilation failure in severe respiratory failure due to community acquired pneumonia. Tanaffos 13:20–28
Roca O, Messika J, Caralt B, García-de-Acilu M, Sztrymf B, Ricard J-D et al (2016) Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care 35:200–205
Chandel A, Patolia S, Brown AW, Collins AC, Sahjwani D, Khangoora V et al (2021) High-flow nasal cannula therapy in COVID-19: using the ROX index to predict success. Respir Care 66:909–919
Calle-Peña ST, Diaz Tavara ED, Aguirre-Milachay E, León-Figueroa DA, Valladares-Garrido MJ (2024) Predictors of high-flow nasal cannula failure in COVID-19 patients in a northern Peruvian hospital. BMC Pulm Med 24:414
Koyama H, Sakai K, Fukaguchi K, Hadano H, Aida Y, Kamio T et al (2024) A comparison study of temporal trends of SARS-CoV2 RNAemia and biomarkers to predict success and failure of high flow oxygen therapy among patients with moderate to severe COVID-19. PLoS ONE 19:e0305077
Grünewaldt A, Peiffer K-H, Bojunga J, Rohde GGU (2023) Characteristics, clinical course and outcome of ventilated patients at a non-surgical intensive care unit in Germany: a single-centre, retrospective observational cohort analysis. BMJ Open 13:e069834
Ewig S, Bauer T, Richter K, Szenscenyi J, Heller G, Strauss R et al (2013) Prediction of in-hospital death from community-acquired pneumonia by varying CRB-age groups. Eur Respir J 41:917–922
Jiang J, Yang J, Jin Y, Cao J, Lu Y (2018) Role of qSOFA in predicting mortality of pneumonia: a systematic review and meta-analysis. Medicine 97:e12634
Gravelyn TR, Weg JG (1980) Respiratory rate as an indicator of acute respiratory dysfunction. JAMA 244:1123–1125
Strauß R, Ewig S, Richter K, König T, Heller G, Bauer TT (2014) The prognostic significance of respiratory rate in patients with pneumonia: a retrospective analysis of data from 705,928 hospitalized patients in Germany from 2010–2012. Deutsches Arzteblatt international 111(503–8):i–v
Booth A, Reed AB, Ponzo S, Yassaee A, Aral M, Plans D et al (2021) Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis. PLoS ONE 16:e0247461
Schwägler A (2021) 020-020l_S3_Behandlung-von-erwachsenen-Patienten-mit-ambulant-erworbener-Pneumonie__2021–05
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K et al (2019) Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 200(7):e45–e67. https://doi.org/10.1164/rccm.201908-1581ST
Guo Q, Li H-Y, Song W-D, Li M, Chen X-K, Liu H et al (2023) Updating cut-off values of severity scoring systems for community-acquired pneumonia to orchestrate more predictive accuracy. Ann Med 55:2202414
Duan J, Yang J, Jiang L, Bai L, Hu W, Shu W et al (2022) Prediction of noninvasive ventilation failure using the ROX index in patients with de novo acute respiratory failure. Ann Intensive Care 12:110
Yaroshetskiy AI, Merzhoeva ZM, Tsareva NA, Trushenko NV, Nuralieva GS, Konanykhin VD et al (2022) Breathing pattern, accessory respiratory muscles work, and gas exchange evaluation for prediction of NIV failure in moderate-to-severe COVID-19-associated ARDS after deterioration of respiratory failure outside ICU: the COVID-NIV observational study. BMC Anesthesiol 22:307
Zhou X, Liu J, Pan J, Xu Z, Xu J (2022) The ROX index as a predictor of high-flow nasal cannula outcome in pneumonia patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. BMC Pulm Med 22:121
Candel BGJ, de Groot B, Nissen SK, Thijssen WAMH, Lameijer H, Kellett J (2023) The prediction of 24-h mortality by the respiratory rate and oxygenation index compared with National Early Warning Score in emergency department patients: an observational study. Eur J Emerg Med Off J Eur Soc Emerg Med 30:110–116
Wang C, Xu R, Zeng Y, Zhao Y, Hu X (2022) A comparison of qSOFA, SIRS and NEWS in predicting the accuracy of mortality in patients with suspected sepsis: a meta-analysis. PLoS ONE 17:e0266755
Richter T, Tesch F, Schmitt J, Koschel D, Kolditz M (2023) Validation of the qSOFA and CRB-65 in SARS-CoV-2-infected community-acquired pneumonia. ERJ Open Res. https://doi.org/10.1183/23120541.00168-2023
Corica B, Tartaglia F, D’Amico T, Romiti GF, Cangemi R (2023) Sex and gender differences in community-acquired pneumonia. Available from: https://link.springer.com/article/https://doi.org/10.1007/s11739-022-02999-7#ref-CR16. Date updated: 19 July 2023. Accessed 19 July 2023
Miguel-Diez J de, Lopez-Herranz M, Hernandez-Barrera V, Miguel-Yanes JM de, Perez-Farinos N, Wärnberg J et al (2021) Community-acquired pneumonia among patients with COPD in Spain from 2016 to 2019. Cohort Study Assessing Sex Differences in the Incidence and Outcomes Using Hospital Discharge Data. J Clin Med 10(21). https://doi.org/10.3390/jcm10214889
Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM et al (2015) Community-acquired pneumonia requiring hospitalization among US Adults. N Eng J Med 373:415–427
de Araújo MFM, Monteiro FPM, de Araújo TM, Lira Neto JCG, Santos LFS, Rolim ILTP et al (2023) Individual and mutual effects of diabetes, hypertension, and obesity on acute respiratory distress syndrome mortality rates in clinical patients: a multicentre study. Front Public Health 11:1219271
Moal B, Orieux A, Ferté T, Neuraz A, Brat GA, Avillach P et al (2023) Acute respiratory distress syndrome after SARS-CoV-2 infection on young adult population: International observational federated study based on electronic health records through the 4CE consortium. PLoS ONE 18:e0266985
Tian J, Xu Q, Liu S, Mao L, Wang M, Hou X (2020) Comparison of clinical characteristics between coronavirus disease 2019 pneumonia and community-acquired pneumonia. Curr Med Res Opin 36:1747–1752
Küçük AO, Pehlivanlar Küçük M, Pehlivanlar A, Ayaydın Mürtezaoğlu S, Çoban K, Topaloğlu Ö et al (2022) Kritik 2019 SARS-CoV-2 hastalarında hastalık başlangıç anından itibaren zaman akış çizelgesi. Tuberkuloz ve toraks 70:63–75
Weerakkody S, Arina P, Glenister J, Cottrell S, Boscaini-Gilroy G, Singer M et al (2022) Non-invasive respiratory support in the management of acute COVID-19 pneumonia: considerations for clinical practice and priorities for research. Lancet Respir Med 10:199–213
Wendel-Garcia PD, Mas A, González-Isern C, Ferrer R, Máñez R, Masclans J-R et al (2022) Non-invasive oxygenation support in acutely hypoxemic COVID-19 patients admitted to the ICU: a multicenter observational retrospective study. Crit Care 26:37
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y et al (2020) Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. The BMJ 369:m1966
Acknowledgements
We thank Professor Eva Herrmann for her excellent assistance in statistical analysis.
Funding
The study was carried out without external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: AG, formal analysis AG, writing—original draft preparation AG, MG—data collection and processing as part of his doctoral thesis review and editing GR. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A. Grünewaldt reports personal fees from Boehringer Ingelheim for lectures and GSK for consultancy during advisory board meetings. G. Rohde reports personal fees from Astra Zeneca, Berlin Chemie, BMS, Boehringer Ingelheim, Chiesi, Essex Pharma, Grifols, GSK, Insmed, MSD, Roche, Solvay, Takeda, Novartis, Pfizer and Vertex for consultancy during advisory board meetings, furthermore personal fees from Astra Zeneca, Berlin Chemie, BMS, Boehringer Ingelheim, Chiesi, Essex Pharma, Grifols, GSK, Insmed, MSD, Roche, Solvay, Takeda, Novartis, Pfizer and Vertex for lectures. M. Gaillard reports no competing interests.
Ethical approval
The study protocol was endorsed by the local ethics committee of the university hospital, Goethe university Frankfurt (study number 22-785).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Grünewaldt, A., Gaillard, M. & Rohde, G. Predictors of high-flow nasal cannula (HFNC) failure in severe community-acquired pneumonia or COVID-19. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03844-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03844-9