Abstract
Aims
Abnormalities in liver biochemistry are common in COVID-19 patients. Hepatic vein Doppler waveform, typically triphasic, may become biphasic or monophasic in cirrhosis, correlating with liver dysfunction, fibrosis, inflammation, and portal hypertension. This study investigates liver ultrasound (US) features in COVID-19 patients, correlating hepatic vein Doppler waveform and portal vein velocity (PVV) with inflammatory indexes and clinical outcomes.
Methods
Fifty-seven patients with SARS-CoV-2 infection participated in a crosssectional study. Bedside upper abdomen US evaluations, including B-mode and Doppler, were conducted using a convex probe. Hepatic vein Doppler waveforms were classified as triphasic, biphasic, or monophasic, and the hepatic vein waveform index (HVWI) was calculated. PVV was measured over three cardiac cycles. Tracings were blindly analyzed by three operators to ensure consistency.
Results
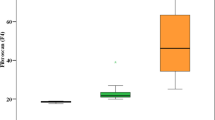
Low HVWI and high PVV correlated with elevated LDH, ALT, d-dimer, and ferritin (p < 0.05). HVWI showed significant negative correlations with ferritin, d-dimer, and ALT (p < 0.05). d-Dimer and ferritin were higher in patients with biphasic/monophasic waveforms (p < 0.05). High PVV and larger spleen diameters predicted worse respiratory outcomes, including CPAP and tracheal intubation (p < 0.05). Optimal cut-off values for PVV (21.7 cm/s) and spleen diameter (9.84 cm) maximized sensitivity and specificity for predicting these outcomes. FIB-4 scores did not correlate with respiratory outcomes or hepatic hemodynamics (p > 0.05). Hemodynamic alterations were not significantly influenced by the presence of SLD (Steatotic Liver Disease).
Conclusions
COVID-19 patients exhibit altered intrahepatic hemodynamics, with hepatic vein waveform abnormalities potentially reflecting liver inflammation and fibrosis. PVV and spleen diameter may serve as non-invasive predictors of respiratory outcomes.




Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Marjot T, Webb GJ, Barritt AS 4th, Moon AM, Stamataki Z, Wong VW, Barnes E (2021) COVID-19 and liver disease: mechanistic and clinical perspectives. Nat Rev Gastroenterol Hepatol 18(5):348–364. https://doi.org/10.1038/s41575-021-00426-4. (Epub 2021 Mar 10)
Dufour JF, Marjot T, Becchetti C, Tilg H (2022) COVID-19 and liver disease. Gut 71(11):2350–2362. https://doi.org/10.1136/gutjnl-2021-326792. (Epub 2022 Jun 14)
Baldelli L, Marjot T, Barnes E, Barritt AS, Webb GJ, Moon AM (2023) SARS-CoV-2 infection and liver disease: a review of pathogenesis and outcomes. Gut Liver. 17(1):12–23. https://doi.org/10.5009/gnl220327. (Epub 2022 Dec 2)
Guan WJ et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720
Sultan S et al (2020) AGA institute rapid review of the gastrointestinal and liver manifestations of COVID-19, meta- analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology 159:320-334.e27
Richardson S et al (2020) Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA 323:2052–2059
Goyal P et al (2020) Clinical characteristics of Covid-19 in New York city. N Engl J Med 382:2372–2374
Youssef M et al (2020) COVID-19 and liver dysfunction: a systematic review and meta- analysis of retrospective studies. J Med Virol 92:1825–1833
Hundt MA, Deng Y, Ciarleglio MM, Nathanson MH, Lim JK (2020) Abnormal liver tests in COVID-19: a retrospective observational cohort study of 1827 patients in a major US Hospital Network. Hepatology 72:1169–1176
Elmunzer BJ et al (2020) Digestive manifestations in patients hospitalized with COVID-19. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2020.09.041
Fu Y et al (2020) Clinical features of COVID-19-infected patients with elevated liver biochemistries: a multicenter, retrospective study. Hepatology. https://doi.org/10.1002/hep.31446
Bertolini A, van de Peppel IP, Bodewes FAJA, Moshage H, Fantin A, Farinati F, Fiorotto R, Jonker JW, Strazzabosco M, Verkade HJ, Peserico G (2020) Abnormal liver function tests in patients with COVID-19: relevance and potential pathogenesis. Hepatology 72(5):1864–1872. https://doi.org/10.1002/hep.31480. (Epub 2020 Oct 20)
Phipps MM, Barraza LH, LaSota ED, Sobieszczyk ME, Pereira MR, Zheng EX, Fox AN, Zucker J, Verna EC (2020) Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large U.S. cohort. Hepatology 72(3):807–817. https://doi.org/10.1002/hep.31404
Yadav DK, Singh A, Zhang Q, Bai X, Zhang W, Yadav RK, Singh A, Zhiwei L, Adhikari VP, Liang T (2021) Involvement of liver in COVID-19: systematic review and meta-analysis. Gut 70(4):807–809. https://doi.org/10.1136/gutjnl-2020-322072. (Epub 2020 Jul 15)
Lei F, Liu YM, Zhou F, Qin JJ, Zhang P, Zhu L, Zhang XJ, Cai J, Lin L, Ouyang S, Wang X, Yang C, Cheng X, Liu W, Li H, Xie J, Wu B, Luo H, Xiao F, Chen J, Tao L, Cheng G, She ZG, Zhou J, Wang H, Lin J, Luo P, Fu S, Zhou J, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu L, Chen G, Li H, Huang X, Zhang BH, Yuan Y (2020) Longitudinal Association between markers of liver injury and mortality in COVID-19 in China. Hepatology 72(2):389–398. https://doi.org/10.1002/hep.31301
Roth NC, Kim A, Vitkovski T, Xia J, Ramirez G, Bernstein D, Crawford JM (2021) Post-COVID-19 cholangiopathy: a novel entity. Am J Gastroenterol 116(5):1077–1082. https://doi.org/10.14309/ajg.0000000000001154
Faruqui S, Okoli FC, Olsen SK, Feldman DM, Kalia HS, Park JS, Stanca CM, Figueroa Diaz V, Yuan S, Dagher NN, Sarkar SA, Theise ND, Kim S, Shanbhogue K, Jacobson IM (2021) Cholangiopathy after severe COVID-19: clinical features and prognostic implications. Am J Gastroenterol 116(7):1414–1425. https://doi.org/10.14309/ajg.0000000000001264
Bethineedi LD, Suvvari TK (2021) Post COVID-19 cholangiopathy—a deep dive. Dig Liver Dis 53(10):1235–1236. https://doi.org/10.1016/j.dld.2021.08.001. (Epub 2021 Aug 9)
Pedersen JF, Madsen LG, Larsen VA, Hamberg O, Horn T, Federspiel B, Bytzer P (2008) A Doppler waveform index to characterize hepatic vein velocity pattern and evaluate hepatic fibrosis. J Clin Ultrasound 36(4):208–211. https://doi.org/10.1002/jcu.20446
Siciliani L, Vitale G, Sorbo AR, Maurizio P, Lodovico RG (2016) Hepatic vein transit time of secondgeneration ultrasound contrast agent: new tool in the assessment of portal hypertension. J Ultrasound 20(1):43–52. https://doi.org/10.1007/s40477-016-0226-1
Zhang L, Yin J, Duan Y, Yang Y, Yuan L, Cao T (2011) Assessment of intrahepatic blood flow by Doppler ultrasonography: relationship between the hepatic vein, portal vein, hepatic artery and portal pressure measured intraoperatively in patients with portal hypertension. BMC Gastroenterol 19(11):84. https://doi.org/10.1186/1471-230X-11-84
Colli A, Cocciolo M, Riva C, Martinez E, Prisco A, Pirola M, Bratina G (1994) Abnormalities of Doppler waveform of the hepatic veins in patients with chronic liver disease: correlation with histologic findings. AJR Am J Roentgenol 162(4):833–837. https://doi.org/10.2214/ajr.162.4.8141001
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3. (Epub 2020 Mar 11. Erratum in: Lancet. 2020 Mar 28;395(10229):1038)
Cadamuro M, Lasagni A, Radu CM, Calistri A, Pilan M, Valle C, Bonaffini PA, Vitiello A, Toffanin S, Venturin C, Friòn-Herrera Y, Sironi S, Alessio MG, Previtali G, Seghezzi M, Gianatti A, Strazzabosco M, Strain AJ, Campello E, Spiezia L, Palù G, Frigo AC, Tosoni A, Nebuloni M, Parolin C, Sonzogni A, Simioni P, Fabris L (2024) Procoagulant phenotype of virus-infected pericytes is associated with portal thrombosis and intrapulmonary vascular dilations in fatal COVID-19. J Hepatol 81(5):872–885. https://doi.org/10.1016/j.jhep.2024.06.014. (Epub 2024 Jun 20)
Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, Zhang M, Tan J, Xu Y, Song R, Song M, Wang L, Zhang W, Han B, Yang L, Wang X, Zhou G, Zhang T, Li B, Wang Y, Chen Z, Wang X (2020) Neutrophilto-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med 18(1):206. https://doi.org/10.1186/s12967-020-02374-0
Karimi A, Shobeiri P, Kulasinghe A, Rezaei N (2021) Novel systemic inflammation markers to predict COVID-19 prognosis. Front Immunol 22(12):741061. https://doi.org/10.3389/fimmu.2021.741061
Medeiros AK, Barbisan CC, Cruz IR, de Araújo EM, Libânio BB, Albuquerque KS (2020) Torres US higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol (NY). 45(9):2748–2754. https://doi.org/10.1007/s00261-020-02648-7. (Epub 2020 Jul 18)
Sarkar S, Kannan S, Khanna P, Singh AK (2022) Role of platelet-to-lymphocyte count ratio (PLR), as a prognostic indicator in COVID-19: a systematic review and meta-analysis. J Med Virol 94(1):211–221. https://doi.org/10.1002/jmv.27297. (Epub 2021 Aug 31)
Ito GNW, Rodrigues VAC, Hümmelgen J, Meschino GSPG, Abou-Rejaile GM, Brenny ID, de Castro Júnior CR, Artigas RC, Munhoz JPS, Cardoso GC, Picheth GF (2022) COVID-19 pathophysiology and ultrasound imaging: a multiorgan review. J Clin Ultrasound 50(3):326–338. https://doi.org/10.1002/jcu.23160. (Epub 2022 Feb 26)
Soroida Y, Nakatsuka T, Sato M, Nakagawa H, Tanaka M, Yamauchi N, Wake T, Nakagomi R, Kinoshita MN, Minami T, Uchino K, Enooku K, Asaoka Y, Tanaka Y, Endo M, Nakamura A, Kobayashi T, Kurihara M, Hikita H, Sato M, Gotoh H, Iwai T, Fukayama M, Ikeda H, Tateishi R, Yatomi Y, Koike K (2019) A novel non-invasive method for predicting liver fibrosis by quantifying the hepatic vein waveform. Ultrasound Med Biol 45(9):2363–2371. https://doi.org/10.1016/j.ultrasmedbio.2019.05.028. (Epub 2019 Jul 12)
Galán M, Vigón L, Fuertes D, Murciano-Antón MA, Casado-Fernández G, Domínguez-Mateos S, Mateos E, Ramos-Martín F, Planelles V, Torres M, Rodríguez-Mora S, López-Huertas MR, Coiras M (2022) Persistent overactive cytotoxic immune response in a spanish cohort of individuals with long-COVID: identification of diagnostic biomarkers. Front Immunol 25(13):848886. https://doi.org/10.3389/fimmu.2022.848886
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 191:145–147. https://doi.org/10.1016/j.thromres.2020.04.013. (Epub 2020 Apr 10)
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180(7):934–943. https://doi.org/10.1001/jamainternmed.2020.0994. (Erratum: In: JAMA Intern Med. 2020 Jul 1; 180(7):1031)
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, HLH Across Speciality Collaboration, UK (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395(10229):1033–1034. https://doi.org/10.1016/S0140-6736(20)30628-0. (Epub 2020 Mar 16)
Boraschi P, Giugliano L, Mercogliano G, Donati F, Romano S, Neri E (2021) Abdominal and gastrointestinal manifestations in COVID-19 patients: is imaging useful? World J Gastroenterol 27(26):4143–4159. https://doi.org/10.3748/wjg.v27.i26.4143
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Giovanni Cappa, Caterina Zattera e Giuseppe Albi. The first draft of the manuscript was written by Luisa Siciliaini and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests, none funding support.
Ethical approval
The study was conducted in accordance with Helsinki ethical standards and was approved by the Institutional Review Board of Fondazione IRCCS Policlinico San Matteo, Pavia, Italy.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siciliani, L., Cappa, G., Zattera, C. et al. Altered liver hemodynamics in patients with COVID-19: a cross sectional study. J Ultrasound 28, 437–445 (2025). https://doi.org/10.1007/s40477-025-01012-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-025-01012-z