Abstract
The uptake of COVID-19 booster vaccination among older adults in China is suboptimal. Here, we report the results of a parallel-group cluster-randomized controlled trial evaluating the efficacy of promoting COVID-19 booster vaccination among grandparents (≥60 years) through a health education intervention delivered to their grandchildren (aged ≥16 years) in a Chinese cohort (Chinese Clinical Trial Registry: ChiCTR2200063240). The primary outcome was the uptake rate of COVID-19 booster dose among grandparents. Secondary outcomes include grandparents’ attitude and intention to get a COVID-19 booster dose. A total of 202 college students were randomized 1:1 to either the intervention arm of web-based health education and 14 daily reminders (n = 188 grandparents) or control arm (n = 187 grandparents) and reported their grandparents’ COVID-19 booster vaccination status at baseline and 21 days. Grandparents in the intervention arm were more likely to receive COVID-19 booster vaccination compared to control cohort (intervention, 30.6%; control, 16.9%; risk ratio = 2.00 (95% CI, 1.09 to 3.66)). Grandparents in the intervention arm also had greater attitude change (β = 0.28 (95% CI, 0.04 to 0.52)) and intention change (β = 0.32 (95% CI, 0.12 to 0.52)) to receive a COVID-19 booster dose. Our results show that an educational intervention targeting college students increased COVID-19 booster vaccination uptake among grandparents in China.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
According to our protocol, the individual deidentified data and documents are not publicly available due to institutional ethics committee regulations but can be made available upon reasonable scientific request to the corresponding author, H.Z., with each request subject to ethical and legislative review from the respective data sources. After internal review and approval, deidentified data and documents will be shared under agreements. The source data, study protocol and statistical analysis plan are provided with this paper. All other data supporting the findings of this study are available from the corresponding author upon reasonable request.
Code availability
The R code used in the analyses is available at Zenodo (10.5281/zenodo.10701551), but this study did not generate new or customized codes or software. The Poisson regression models were fitted using the glm function. The robust standard errors of Poisson models were computed using the glm.cluster function from the miceadds R package. The generalized estimation equation models were computed using the geeglm function from the geepack R package. The multiple imputation was performed using mice R package. The forest plots were created using the forestploter R package.
References
World Health Organization. WHO Coronavirus (COVID-19) Dashboard, https://covid19.who.int/ (2023).
Zhang, Q., Bastard, P., Cobat, A. & Casanova, J. L. Human genetic and immunological determinants of critical COVID-19 pneumonia. Nature 603, 587–598 (2022).
Wei, Z. et al. The importance of booster vaccination in the context of Omicron wave. Front. Immunol. 13, 977972 (2022).
O’Driscoll, M. et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature 590, 140–145 (2021).
Mohammed, I. et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Hum. Vaccin. Immunother. 18, 2027160 (2022).
Jiang, N. et al. Changes of COVID-19 knowledge, attitudes, practices and vaccination willingness among residents in Jinan, China. Front. Public Health 10, 917364 (2022).
Detailed Implementation of Prevention and Control Measures (Joint Prevention and Control Mechanism of the State Council, 2022); http://www.gov.cn/xinwen/gwylflkjz216/index.htm
Zang, S., Zhang, X., Qu, Z., Chen, X. & Hou, Z. Promote COVID-19 vaccination for older adults in China. China CDC Wkly 4, 832–834 (2022).
Dardalas, I. et al. Predictors of influenza vaccination among elderly: a cross-sectional survey in Greece. Aging Clin. Exp. Res. 32, 1821–1828 (2020).
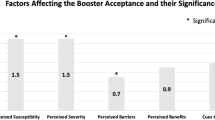
Qin, C. et al. Acceptance of the COVID-19 vaccine booster dose and associated factors among the elderly in China based on the health belief model (HBM): a national cross-sectional study. Front. Public Health 10, 986916 (2022).
Veronese, N. et al. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people: a systematic review and meta-analysis. Ageing Res. Rev. 72, 101489 (2021).
Wang, G. et al. Determinants of COVID-19 vaccination status and hesitancy among older adults in China. Nat. Med. 29, 623–631 (2023).
Wang, J. et al. Willingness to accept COVID-19 vaccine among the elderly and the chronic disease population in China. Hum. Vaccin. Immunother. 17, 4873–4888 (2021).
Arpino, B., Bordone, V. & Di Gessa, G. COVID-19 precautionary behaviors and vaccine acceptance among older individuals: the role of close kin. Proc. Natl Acad. Sci. USA 120, e2214382120 (2023).
He, F. J. et al. A school-based education programme to reduce salt intake in children and their families (School-EduSalt): protocol of a cluster randomised controlled trial. BMJ Open 3, e003388 (2013).
Murayama, Y. et al. The effect of intergenerational programs on the mental health of elderly adults. Aging Ment. Health 19, 306–314 (2015).
Chu, L. et al. Obtaining information from different sources matters during the COVID-19 pandemic. Gerontologist 61, 187–195 (2021).
Jia, Y. et al. Health literacy and disparities in knowledge, attitude and practice regarding COVID-19 among college students during the COVID-19 outbreak in China: a cross-sectional study. Risk Manag. Healthc. Policy 14, 4477–4488 (2021).
Guo, Z. et al. Young adults’ intention to encourage COVID-19 vaccination among their grandparents: a nationwide cross-sectional survey of college students in China. Vaccine X 16, 100439 (2024).
Freeman, D. et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): a single-blind, parallel-group, randomised controlled trial. Lancet Public Health 6, e416–e427 (2021).
Okuhara, T. et al. Encouraging COVID-19 vaccination via an evolutionary theoretical approach: a randomized controlled study in Japan. Patient Educ. Couns. 105, 2248–2255 (2022).
Schmid, P., Rauber, D., Betsch, C., Lidolt, G. & Denker, M. L. Barriers of influenza vaccination intention and behavior: a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 12, e0170550 (2017).
Crawshaw, A. F. et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: a systematic review. Lancet Infect. Dis. 22, e254–e266 (2022).
Liu, S. et al. Factors associated with pneumococcal vaccination among an urban elderly population in China. Hum. Vaccin. Immunother. 10, 2994–2999 (2014).
Wagner, A. L., Montgomery, J. P., Xu, W. & Boulton, M. L. Influenza vaccination of adults with and without high-risk health conditions in China. J. Public Health 39, 358–365 (2017).
Pan, C., Cao, N., Kelifa, M. O. & Luo, S. Age and cohort trends in disability among Chinese older adults. Front. Public Health 11, 998948 (2023).
Kan, T. & Zhang, J. Factors influencing seasonal influenza vaccination behaviour among elderly people: a systematic review. Public Health 156, 67–78 (2018).
Spitzer, S., Shaikh, M. & Weber, D. Older Europeans’ health perception and their adaptive behaviour during the COVID-19 pandemic. Eur. J. Public Health 32, 322–327 (2022).
Qin, C. et al. COVID-19 vaccination coverage among 42,565 adults amid the spread of Omicron variant in Beijing, China. Vaccines 11, 739 (2023).
Antonucci, T. C., Jackson, J. S. & Biggs, S. Intergenerational relations: theory, research, and policy. J. Soc. Issues 63, 679–693 (2007).
Umberson, D. Family status and health behaviors: social control as a dimension of social integration. J. Health Soc. Behav. 28, 306–319 (1987).
Number of Students in Higher Education Institutions (Ministry of Education of the People’s Republic of China, 2021); http://www.moe.gov.cn/jyb_sjzl/moe_560/2021/quanguo/202301/t20230104_1038055.html
Number of Higher Education Institutions (Ministry of Education of the People’s Republic of China, 2021); http://www.moe.gov.cn/jyb_sjzl/moe_560/2021/quanguo/202301/t20230104_1038056.html
Notice on Printing and Distributing the Work Plan for Strengthening the Vaccination of the Elderly Against the Novel Coronavirus (Joint Prevention and Control Mechanism of the State Council, 2022); http://www.gov.cn/xinwen/2022-11/29/content_5729388.htm
Pearce, M. et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatry 79, 550–559 (2022).
Bian, J. et al. College students’ influence on COVID-19 vaccination uptake among seniors in China: a protocol of combined cross-sectional and experimental study. BMC Public Health 23, 1322 (2023).
Zhang, X. et al. Impact of web-based health education on HPV vaccination uptake among college girl students in Western and Northern China: a follow-up study. BMC Womens Health 22, 46 (2022).
Siu, J. Y., Cao, Y. & Shum, D. H. K. Perceptions of and hesitancy toward COVID-19 vaccination in older Chinese adults in Hong Kong: a qualitative study. BMC Geriatr. 22, 288 (2022).
Ye, W. et al. Persuasive effects of message framing and narrative format on promoting COVID-19 vaccination: a study on Chinese college students. Int. J. Environ. Res. Public Health 18, 9485 (2021).
Rothman, A. J. & Salovey, P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol. Bull. 121, 3–19 (1997).
Gursoy, D., Ekinci, Y., Can, A. S. & Murray, J. C. Effectiveness of message framing in changing COVID-19 vaccination intentions: moderating role of travel desire. Tour Manag. 90, 104468 (2022).
Borah, P. Message framing and COVID-19 vaccination intention: moderating roles of partisan media use and pre-attitudes about vaccination. Curr. Psychol. 3, 1–10 (2022).
Introduce the Relevant Situation of Scientific and Accurate Prevention and Control of Epidemic Situation (Joint Prevention and Control Mechanism of the State Council, 2022); http://www.gov.cn/xinwen/gwylflkjz205/index.htm
Hemming, K. & Taljaard, M. Sample size calculations for stepped wedge and cluster randomised trials: a unified approach. J. Clin. Epidemiol. 69, 137–146 (2016).
Campbell, M. J., Donner, A. & Klar, N. Developments in cluster randomized trials and statistics in medicine. Stat. Med. 26, 2–19 (2007).
Lee, R. Y. et al. Association of physician orders for life-sustaining treatment with ICU admission among patients hospitalized near the end of life. JAMA 323, 950–960 (2020).
Pintilie, M. Competing Risks: A Practical Perspective (Wiley, 2006).
Acknowledgments
We thank Prof. Zunyou Wu, late chief epidemiologist from the Chinese Center for Disease Control and Prevention, for his kind support and encouragement to our study. H.Z. is supported by the Natural Science Foundation of China Excellent Young Scientists Fund (82022064). The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank our partners at Sun Yat-sen University and Bengbu University. We thank all participants who made this research possible.
Author information
Authors and Affiliations
Contributions
H.Z. and J.B. contributed to the study design. J.B., W.Z., Z.G., X.L. and L.F. contributed to data collection, data analysis and manuscript preparation. J.B. and L.F. optimized the statistical analysis method. Z.L., Y.S., Y.G., Y.C., Q.L., L.H., C.S., T.F. and H.Z. reviewed and verified the data in the study. J.B., W.Z., Z.G., X.L. and L.F. contributed equally to this paper. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 A subgroup per-protocol analysis of the primary outcome of COVID-19 booster dose uptake among grandparents.
RR = risk ratio. CI = confidence interval. In the forest plot, the points are represented as the point estimate of risk ratio, and the lines are represented as the range of the 95% confidence interval. Model 1 is a Poisson regression model. Model 2 is a Poisson regression model with robust standard error. In the two models, adjustment is made for grandparents’ sex, age, residence, education, history of cohabitation with the enrolled grandchild, living status, frequency of leaving the home, and presence of one or more chronic disease. P value is from interaction tests using Model 2. Analyses are two-sided at 5% significance level.
Extended Data Fig. 2 A subgroup intention-to-treat analysis of the primary outcome of COVID-19 booster dose uptake among grandparents.
RR = risk ratio. CI = confidence interval. In the forest plot, the points are represented as the point estimate of risk ratio, and the lines are represented as the range of the 95% confidence interval. Model 1 is a Poisson regression model. Model 2 is a Poisson regression model with robust standard error. In the two models, adjustment is made for grandparents’ sex, age, residence, education, history of cohabitation with the enrolled grandchild, living status, frequency of leaving the home, and presence of one or more chronic disease. P value is from interaction tests using Model 2. Analyses are two-sided at 5% significance level.
Extended Data Fig. 3 Secondary outcome of changes in grandparents’ attitude and intention to get a COVID-19 booster dose.
In the PP set, the number of participants is 147 in the intervention arm and 154 in the control arm. In the ITT set, the number of participants is 188 in the intervention arm and 187 in the control arm. Mean scores in the ITT set are estimated by multiple imputation.
Supplementary information
Supplementary Information
Supplementary materials of intervention, study protocol, statistical analysis plan and CONSORT 2010 checklist.
Supplementary Table 1
Inclusion and exclusion criteria.
Supplementary Table 2
Summary of enrollment.
Supplementary Table 3
Diagram of the study events.
Supplementary Table 4
Diagram of intervention for college students.
Supplementary Table 5
Completer analysis of the study.
Supplementary Table 6
Reliability analysis of the attitude and intention scores among grandparents.
Supplementary Table 7
Sensitivity analysis for the subgroup analysis using generalized estimating equation (GEE) model.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bian, J., Zhang, W., Guo, Z. et al. Influence of grandchildren on COVID-19 vaccination uptake among older adults in China: a parallel-group, cluster-randomized controlled trial. Nat Aging 4, 638–646 (2024). https://doi.org/10.1038/s43587-024-00625-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-024-00625-z