Abstract
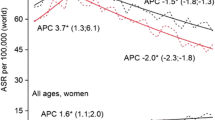
In Japan, high-quality cancer statistics are collected through cancer registries. However, these data are rarely summarized or reported in research articles. We compiled statistical data on lung cancer in Japan including the COVID-19 pandemic. In 2019, the number of cases of lung cancer in Japan was 126,548. The age-adjusted incidence rate of lung cancer increased from 23.2/100,000 to 42.4/100,000 in males and from 7.2/100,000 to 18.3/100,000 in females between 1975 and 2019. The age-adjusted mortality rate of lung cancer in Japan increased since 2000, after which it decreased. This trend was similar in both males and females. We also investigated statistics on lung cancer worldwide (Australia, Sweden, England, and the United States [USA]). The age-adjusted incidence rate of lung cancer in the data standardized to the world population for males has increased only in Japan; for females, it has decreased only in the USA. Global age-adjusted lung cancer mortality rates have been declining in all countries. In addition, the COVID-19 pandemic has not affected the age-adjusted mortality rate of lung cancer. On the other hand, the number of individuals undergoing lung cancer screening in Japan decreased from 7.92 million in 2019 to 6.59 million in 2020. The COVID-19 pandemic may have affected individuals undergoing lung cancer screening, and its impact on lung cancer needs to be continuously monitored in the future.






Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Horinouchi H, Kusumoto M, Yatabe Y et al (2022) Lung cancer in Japan. J Thorac Oncol 17(3):353–361. https://doi.org/10.1016/j.jtho.2021.11.020
Sobue T (2000) A case-control study for evaluating lung cancer screening in Japan. Cancer 89(11 Suppl):2392–2396. https://doi.org/10.1002/1097-0142(20001201)89:11+%3c2392::aid-cncr13%3e3.3.co;2-a
Punekar SR, Shum E, Grello CM et al (2022) Immunotherapy in non-small cell lung cancer: Past, present, and future directions. Front Oncol 12:877594. https://doi.org/10.3389/fonc.2022.877594
Chirieac LR, Dacic S (2010) Targeted therapies in lung cancer. Surg Pathol Clin 3(1):71–82. https://doi.org/10.1016/j.path.2010.04.001
Collaborators GBDCoD (2024) Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440):2100–2132. https://doi.org/10.1016/S0140-6736(24)00367-2
Nakatani H (2019) Population aging in Japan: policy transformation, sustainable development goals, universal health coverage, and social determinates of health. Glob Health Med 1(1):3–10. https://doi.org/10.35772/ghm.2019.01011
Spiro SG, Silvestri GA (2005) One hundred years of lung cancer. Am J Respir Crit Care Med 172(5):523–529. https://doi.org/10.1164/rccm.200504-531OE
Redpath TW (1997) MRI developments in perspective. Br J Radiol. https://doi.org/10.1259/bjr.1997.0010
Townsend DW (2008) Combined positron emission tomography-computed tomography: the historical perspective. Semin Ultrasound CT MR 29(4):232–235. https://doi.org/10.1053/j.sult.2008.05.006
Urikura A, Yoshida T, Matsubara K et al (2023) Number of computed tomography scanners and regional disparities based on population and medical resources in Japan. Radiol Phys Technol 16(3):355–365. https://doi.org/10.1007/s12194-023-00725-2
Huang F, Pan B, Wu J et al (2017) Relationship between exposure to PM25 and lung cancer incidence and mortality: A meta-analysis. Oncotarget 8(26):43322–43331. https://doi.org/10.18632/oncotarget.17313
Thandra KC, Barsouk A, Saginala K et al (2021) Epidemiology of lung cancer. Contemp Oncol (Pozn) 25(1):45–52. https://doi.org/10.5114/wo.2021.103829
Nagasawa T, Saito J, Odawara M et al (2022) Smoking cessation interventions and implementations in Japan: a study protocol for a scoping review and supplemental survey. BMJ Open 12(12):e063912. https://doi.org/10.1136/bmjopen-2022-063912
Tabuchi T, Nakamura M, Nakayama T et al (2016) Tobacco price increase and smoking cessation in japan, a developed country with affordable tobacco: a national population-based observational study. J Epidemiol 26(1):14–21. https://doi.org/10.2188/jea.JE20140183
Nguyen PT, Katanoda K, Saito E et al (2022) Trends in lung cancer incidence by gender, histological type and stage at diagnosis in Japan, 1993 to 2015: A multiple imputation approach. Int J Cancer 151(1):20–32. https://doi.org/10.1002/ijc.33962
Ohe Y, Ohashi Y, Kubota K et al (2007) Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: Four-Arm Cooperative Study in Japan. Ann Oncol 18(2):317–323. https://doi.org/10.1093/annonc/mdl377
Schiller JH, Harrington D, Belani CP et al (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346(2):92–98. https://doi.org/10.1056/NEJMoa011954
Kubota K, Watanabe K, Kunitoh H et al (2004) Phase III randomized trial of docetaxel plus cisplatin versus vindesine plus cisplatin in patients with stage IV non-small-cell lung cancer: the Japanese Taxotere Lung Cancer Study Group. J Clin Oncol 22(2):254–261. https://doi.org/10.1200/jco.2004.06.114
Fukuoka M, Wu YL, Thongprasert S et al (2011) Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol 29(21):2866–2874. https://doi.org/10.1200/JCO.2010.33.4235
Inoue A, Kobayashi K, Maemondo M et al (2013) Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naive non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol. https://doi.org/10.1093/annonc/mds214
Borghaei H, Paz-Ares L, Horn L et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373(17):1627–1639. https://doi.org/10.1056/NEJMoa1507643
Brahmer J, Reckamp KL, Baas P et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373(2):123–135. https://doi.org/10.1056/NEJMoa1504627
Saito M, Shiraishi K, Kunitoh H et al (2016) Gene aberrations for precision medicine against lung adenocarcinoma. Cancer Sci 107(6):713–720. https://doi.org/10.1111/cas.12941
Ramalingam S, Gray J, Ohe Y et al (2019) Osimertinib vs comparator EGFR-TKI as first-line treatment for EGFRm advanced NSCLC (FLAURA): Final overall survival analysis. Ann Oncol 30:v914–v915
Peters S, Camidge DR, Shaw AT et al (2017) Alectinib versus crizotinib in untreated ALK-positive non–small-cell lung cancer. N Engl J Med 377(9):829–838
Moro-Sibilot D, Cozic N, Pérol M et al (2019) Crizotinib in c-MET-or ROS1-positive NSCLC: results of the AcSé phase II trial. Ann Oncol 30(12):1985–1991
Planchard D, Besse B, Groen HJ et al (2016) Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol 17(7):984–993
Almeda N, Gómez-Gómez I (2022) The impact of the COVID-19 pandemic on smoking consumption: a systematic review of longitudinal studies. Front Psychiatry 13:941575. https://doi.org/10.3389/fpsyt.2022.941575
Machii R, Takahashi H (2023) Japanese cancer screening programs during the COVID-19 pandemic: Changes in participation between 2017–2020. Cancer Epidemiol 82:102313. https://doi.org/10.1016/j.canep.2022.102313
Machii R, Takahashi H, Miyazawa J et al (2024) Cancer screening in Japan 2 years after the COVID-19 pandemic: Changes in participation, 2017–2021. Prev Med Rep 39:102649. https://doi.org/10.1016/j.pmedr.2024.102649
Maringe C, Spicer J, Morris M et al (2020) The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 21(8):1023–1034. https://doi.org/10.1016/S1470-2045(20)30388-0
Vanderbruggen N, Matthys F, Van Laere S et al (2020) Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur Addict Res 26(6):309–315. https://doi.org/10.1159/000510822
Jarvis CI, Gimma A, van Zandvoort K et al (2021) The impact of local and national restrictions in response to COVID-19 on social contacts in England: a longitudinal natural experiment. BMC Med 19(1):52. https://doi.org/10.1186/s12916-021-01924-7
Islam N, Sharp SJ, Chowell G et al (2020) Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ 370:m2743. https://doi.org/10.1136/bmj.m2743
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Yamamoto has nothing to disclose. Dr. Shirasawa reports personal fees from MSD, personal fees from Asahi Kasei, personal fees from AstraZeneca.K.K, personal fees from Ono, personal fees from BMS, personal fees from Chugai, personal fees from Eli Lilly, personal fees from Daiichi Sankyo, outside the submitted work; . Dr. Naoki reports personal fees from AstraZeneca.K.K, personal fees from BMS, grants and personal fees from Chugai, grants and personal fees from Nippon Boehringer Ingelheim, grants from ONO, grants from Taiho , grants from PAREXEL, outside the submitted work; .
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yamamoto, H., Shirasawa, M. & Naoki, K. Analysis of lung cancer incidence, mortality trends, and smoking rates in Japan:1975–2022 with insights on the impact of COVID-19. Int J Clin Oncol 30, 199–209 (2025). https://doi.org/10.1007/s10147-025-02695-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-025-02695-4