Abstract
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused unprecedented pressure on healthcare systems globally. The lack of quality guidelines on the management of COVID-19 in rheumatologic disease, renal disease, hematological malignancy, and solid organ transplant recipients has resulted in a wide variation in clinical practice.
Methods
Using a Delphi process, a panel of 16 key opinion leaders developed clinical practice statements regarding vaccine recommendations in areas where standards are absent or limited. Agreement among practicing physicians with consensus statements was also assessed via an online physician survey. The strength of the consensus was determined by the following rating system: a strong rating was defined as all four key opinion leaders (KOLs) rating the statement ≥ 8, a moderate rating was defined as three out of four KOLs rating the statement ≥ 8, and no consensus was defined as less than three out of four KOLs provided a rating of ≤ 8. Specialists voted on agreement with each consensus statement for their disease area using the same ten-point scoring system.
Results
Key opinion leaders in rheumatology, nephrology, and hematology achieved consensuses for all nine statements pertaining to the primary and booster series with transplant physicians reaching consensus on eight of nine statements. Experts agreed that COVID-19 vaccines are safe, effective, and well tolerated by patients with rheumatological conditions, renal disease, hematologic malignancy, and recipients of solid organ transplants. The Delphi process yielded strong to moderate suggestions for the use of COVID-19 messenger ribonucleic acid (mRNA) vaccines and the necessity of the COVID-19 booster for the immunocompromised population. The expert panel had mixed feelings concerning the measurement of antibody titers, higher-dose mRNA vaccines, and the development of disease-specific COVID-19 guidance.
Conclusions
These results confirmed the necessity of COVID-19 vaccines and boosters in immunocompromised patients with rheumatologic disease, renal disease, hematological malignancy, and solid organ transplant recipients. Statements where consensus was not achieved were due to absent or limited evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There is a substantial COVID-19 disease burden in the European Union. |
This paper assesses the need, development, and agreement among key opinion leaders regarding the prevention of COVID-19 in the immunocompromised population. |
What was learned from this study? |
This Delphi panel study advances informed decision-making on how to prevent COVID-19 in individuals with rheumatologic disease, renal disease, hematological malignancy, and solid organ transplant. |
The multidisciplinary panel emphasized the need for actionable recommendations for COVID-19 boosters and vaccines in immunocompromised patient populations to reduce the incidence of disease and minimize the severity of complications to due to COVID-19. |
Introduction
Vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been demonstrated to be safe and highly effective for the general population in both large clinical trials and real-world data. There are two types of COVID-19 vaccines approved for use by the European Medicine Agency (EMA), which differ in their means of immunostimulation via novel messenger ribonucleic acid (mRNA) technology or traditional protein subunits. The two mRNA vaccines that were approved for the prevention of COVID-19 are mRNA-1273 (Spikevax®, Moderna, Inc.; Cambridge, MA, USA) [1] and BNT162b2 (Comirnaty®, Pfizer/BioNTech; New York, NY, USA/Mainz, Germany) [2]. The EMA has also approved two protein vaccines (NVX-CoV2373, Nuvaxovid®, Novavax; Gaithersburg, MD, USA, and B.1.351 and B.1.1.7, Bimervax®, Hipra Human Health S.L.; Catalonia, Spain) [3, 4] and two adenoviral vector vaccines (Ad26.COV2-S, Jcovden®, Janssen; Beerse, Belgium and ChAdOx1-S, Vaxzevria®, AstraZeneca; Gaithersburg, MD, USA) [5, 6]. Despite being a high-risk subgroup, immunocompromised individuals and patients receiving immunosuppressive medications (Tian-FIA) were excluded from participating in pivotal trials of the aforementioned vaccines [7,8,9,10,11,12].
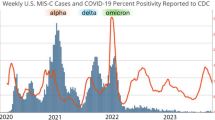
The COVID-19 pandemic has disproportionately impacted immunocompromised patients. Vaccine efficacy against symptomatic infection, severe disease, hospitalization, or death has been widely proven in the immunocompetent population [13,14,15,16,17,18,19,20,21,22]. However, vaccine efficacy may vary in immunocompromised populations, conditions that also increase risk for progression to severe disease, prolonged hospitalizations, and death. To date, there has been a lack of definitive insight and understanding of the appropriate vaccine, dosing schedules, and frequency of boosters needed for specific groups of immunocompromised people. While there are established vaccination recommendations for the healthy population, there are inconsistencies and a lack of specificity in vaccine guidelines for immunocompromised populations. Current COVID-19 vaccine guideline recommendations are for all groups of immunocompromised individuals and are not specific to a distinct immunocompromised state, despite the increased risk for morbidity and mortality among some disease groups.
The BNT162b2 and mRNA-1273 COVID-19 vaccines have both been shown in large phase III clinical trials to be more than 90% effective at preventing lab-confirmed COVID-19 illness and severe infections [13, 14]. The single-dose Ad26.COV2.S reduced the incidence of symptomatic COVID-19 with a reported overall efficacy of 66.1% based on data from the phase III clinical trial [16]. Although there is broad acceptance that the incidence of severe COVID-19 illness is lower following vaccination and booster with BNT162b2 or mRNA-1273 as compared to an adenovirus vaccine in immunocompetent individuals, the overall impact on specific immunocompromised populations is largely unknown [23]. A retrospective cohort study in Europe reported SARS-CoV-2 infections occurred at a rate of 58.7 per 1000 person-years in ChAdOx1-S—ChAdOx1-S recipients and 37.1 per 1000 person-years in BNT162b2– BNT162b2 recipients [24]. From a recent systematic literature review and meta-analysis of 80 global studies, Nejad et al. reported that immunocompromised individuals who were administered mRNA vaccines induced higher immunity after the second dose compared to vector vaccines [25]. Furthermore, the response to homologous versus heterologous booster vaccinations remains unclear. Meta-analysis of three randomized clinical trials including healthy adults found that the highest antibody responses had been reported for the homologous vaccination regimen of mRNA-1273/mRNA-1273/mRNA-1273, followed by the heterologous regimen of BNT162b2 /BNT162b2 /m RNA-1273 [26]. A German study conducted on kidney transplant recipients reported that seroconversion was observed in 75% of patients with heterologous vaccination and 67.8% of patients with mRNA exclusive vaccination (odds ratio, 1.72; 95% confidence interval, 0.59–4.99; P = 0.32) [27].
Conflicting evidence has been reported regarding dosing schedules for immunocompromised persons. Embi et al. reported immunocompromised persons should receive three doses and a booster of mRNA COVID-19 vaccines [28], however, Mues et al. observed a two-dose mRNA regimen was effective in preventing COVID-19 among immunocompromised patients [29]. In a recent systematic review and meta-analysis of 82 studies [30], response to first and second vaccine doses among the immunocompromised groups showed significantly disparate results across disease states. Risk ratios for seroconversion associated with the first and second vaccine doses were lowest for organ transplant recipients, followed by patients with hematological cancers, immune-mediated inflammatory disorders, and solid cancers as compared to immunocompetent individuals. A recent pairwise meta-analysis found that mRNA-1263 was clinically more effective (50 or 100 mcg/dose) when compared to BNT162b2 (30 mcg/dose) using the GRADE framework [31] in immunocompromised populations that included studies in patients with rheumatic disease, hemodialysis and kidney transplant patients, patients with cancer, and solid organ transplant recipients (SOTRs). Results from 17 studies found a significantly reduced risk of SARS-CoV-2 infection [RR, 0.85 (95% CI 0.75–0.97); P = 0.0151; I2 = 67.7%], severe SARS-CoV-2 infection [RR, 0.85 (95% CI 0.77–0.93); P = 0.0009; I2 = 0%], COVID-19-associated hospitalization (RR, 0.88 [95% CI 0.79–0.97]; P < 0.0001; I2 = 0%], and COVID-19-associated mortality [RR, 0.63 (95% CI 0.44–0.90); P = 0.0119; I2 = 0%] [31]. Thus, vaccine regimes may need to be tailored according to the cause and degree of immunocompromise.
Vaccination is the most promising way to minimize negative outcomes from COVID-19, and because of a rapid change in our outlook about the vaccines, there is a need for specific guidance for vaccination among immunocompromised populations. Vaccine trials have excluded immunocompromised groups, such as patients with cancer, renal disease, SOTR, and those with rheumatological disorders, leading to a paucity of data on the efficacy and safety of vaccines in these groups. This creates challenges as clinical and policy decisions must be made based on extrapolation of data gathered from populations with better physiologic immunological baselines, physician experience and real-world evidence.
As COVID-19 is becoming endemic, national healthcare systems are now tasked with recommending the best use of available vaccines for distinct populations specific to their own geographic region. There are limitations to the current body of real-world evidence studies and a lack of published literature specific to COVID-19 vaccinations for immunocompromised populations in the European Union. Because the immunologic principles related to the use of vaccines and the impact of vaccine-preventable illnesses on patients cross a broad range of immunocompromised states, our objective was to define and delineate vaccination considerations for four immunocompromised disease areas within the context of the European Union. We employed a Delphi panel methodology similar to that used by the American College of Rheumatology [32] to gauge key opinion leader (KOL) agreement, incorporate insights, and revise accordingly to achieve consensus recommendations. The goal was to provide adapted recommendations for immunocompromised populations within four specific disease states (e.g., rheumatologic disease, renal disease, hematological malignancy, and SOTR) to ensure they receive the appropriate direction on vaccines. The development process followed a rigorous and formal methodology, was based on disease and EU-specific literature reviews, incorporated panelist expertise from specialists in the four disease states, integrated input from related medical experts in other disciplines (e.g., infectious disease, epidemiology), and included direct participation by healthcare professionals in the EU to elucidate their insights and preferences regarding the consensus statements.
Primary Objectives
-
To gain insights into the perspectives of key opinion leaders in each disease area regarding vaccine recommendations for individuals with rheumatologic disease, renal disease, hematological malignancy, and solid organ transplant recipients in the European Union.
-
To establish a set of consensus statements on COVID-19 vaccinations of patients in four immunocompromised conditions: renal disease, solid organ transplant, rheumatology, and hematology/oncology.
Secondary Objective
-
To assess the level of agreement among practicing physicians within each disease area with the consensus statements reached among key opinion leaders via an online physician across the European Union.
Methods
A similar methodology is presented elsewhere for the United States panel https://doi.org/10.1007/s40121-024-01052-8.
Modified Delphi Panel: Overview and Approach
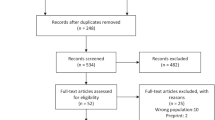
The Delphi technique is a scientific method to organize and manage structured group communication processes to derive consensus. A two-phase, online consensus Delphi study was undertaken with an expert panel consisting of four key opinion leaders (KOLs) with expertise in infectious disease, rheumatology, transplant, hematology/oncology, or nephrology to establish consensus on a set of disease-specific recommendations for COVID-19 vaccination in immunocompromised populations (Fig. 1).
Delphi panel: Overview and approach (also presented here: https://doi.org/10.1007/s40121-024-01052-8). SME subject matter expert, KOL key opinion leader
Delphi Panel Preparation: Development of Draft Consensus Statements
A multi-disciplinary team identified key topics to serve as themes for the consensus statements with subject matter experts from epidemiology, immunology, evidence synthesis, and a medical director with specific expertise in infectious disease, vaccinology, and immune deficiencies. Topics identified consisted of three domains of interest of consideration in disease-specific populations: primary/initial vaccination series (e.g., need for vaccination, number of vaccines), booster/updated vaccinations (e.g., frequency), and additional vaccination considerations (e.g., value of antibody titers, vaccine type). Draft consensus statements were constructed based on the multi-disciplinary team findings and were then used to refine the literature search criteria.
We previously conducted a systematic review of prospective observational studies comparing the efficacy of COVID-19 vaccination in immunocompromised and immunocompetent participants [42]. We supplemented this base of evidence with a targeted literature review of evidence published after January 1, 2022, that addressed COVID-19 vaccinations in the specific immunocompromised populations that addressed the initial statement items. Further, we sought European Union-specific evidence. Up to five supporting articles for each statement topic were collected and summarized. We used the following hierarchy for evidence gathering (strongest to weakest): systematic literature review or meta-analysis; real-world evidence that met the following criteria: population included immunocompromised populations or patients with rheumatological conditions, renal disease, hematological malignancy, or solid organ transplants, encompassed a large sample size, and equal distribution of different vaccines covered; clinical trials in priority order: randomized double-blinded, single-blinded, open-label; cohort studies; recommendations/reviews published by disease-specific groups (e.g., European Hematology Association), and government bodies (e.g., Centers for Disease Control).
Draft consensus statements for each of the four disease-specific groups were revised based on supporting evidence from the literature [9, 23,24,25,26,27, 30, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89]. Subsequently, the draft consensus statements were presented to key opinion leaders.
Delphi Panel Phase 1: Qualitative Interviews
Forty-five-minute interviews were conducted with four KOLs per disease group in the EU. KOLs first rated their agreement with the statement on a scale of 1–10, where 1 is “Do not agree at all” and 10 is “significantly agree”. Trained moderators reviewed each draft statement (~ 15 statements) with KOLs (~ 3–5 min per statement) to obtain feedback on supporting resources/information, ways to improve the accuracy of statements, and further define and refine wording. In some cases, additional literature search and review was performed when respondents requested more supporting evidence. Respondents were asked to rework statements to provide a higher level of agreement. Once reworded, the statements were reassessed by KOLs using the same rating scale.
Delphi Panel Phase 2: Finalization of Consensus Statements
Revised consensus statements were shared with the four KOLs on a virtual bulletin board. The same KOLs completed three rounds of review in an interactive online bulletin board in 30-min sessions on three separate days, each round of engagement included targeted questions followed by a review to reassess steps to refine the statement for the next round. Consensus was determined by the results of day three. The strength of the consensus was determined by the following rating: strong rating was defined as all four KOLs rating the statement ≥ 8, moderate rating was defined as three out of four KOLs rating the statement ≥ 8, and no consensus was defined as less than three out of four KOLs provided a rating of ≤ 8.
Delphi Panel Phase 3: Physician Survey
An online survey was conducted to assess physician agreement with the final consensus statements developed by KOLs prior to publication. Fifty specialists per disease area were recruited to take part in the survey from the European Union (N = 200). Specialists voted on agreement with each consensus statement for their disease area using the same ten-point scoring system utilized in the Delphi panel via an online survey. Specialists were provided the option of including a reason for the rating they provided. The percentage of physicians surveyed (n = 50 per group) who rated their agreement with the statement as ≥ 8 out of 10 is reported.
Delphi Panel Member Sample
Three KOLs in the European Union with experience in each disease-specific areas (e.g., autoimmune rheumatic disease, renal disease, solid organ transplant, or hematologic/oncology) were recruited for the Delphi panel and were supported by an infectious disease specialist.
To accomplish the objective of understanding the consensus of vaccination recommendations among disease-specific experts, a nonrandom sampling process consistent with standard Delphi panel approaches was utilized to select KOLs for this panel. A third-party recruitment vendor with local representatives in the region was used to support the qualification, recruitment, and scheduling of the participants. The Delphi panel members were anonymous to the study team and the eligibility selection for KOLs included treatment area specialists in the field of renal disease, rheumatology, solid organ transplant, and hematology-oncology. In order to qualify as a panel member, the criteria that were utilized for selecting the experts were based on breadth of experience and knowledge of the topic, number of published articles, and frequency of engagements specific to immunocompromised individuals. To ensure the panel reflected experts treating patients with immunocompromised conditions, additional criteria were set to ensure each expert currently provided vaccination recommendations to a high-volume of immunocompromised patients. In addition, the study used a double-blind design where the participants were blind to the sponsor of the study and the sponsor did not have access to personal information on the participants to further reduce bias. The study team did not have direct access to the participants’ personal information.
All physicians who participated were remunerated for their time. The group was selected based on six criteria. Within the past 12 months, KOLs must have seen at least 100 patients, at least 50 immunocompromised patients; scored at least five points out of seven points on a COVID-19 knowledge questionnaire, spend ≥ 25% of working hours performing clinical management, must have responsibilities for vaccine recommendations, published at least one article, and had at least five scientific engagements (published articles, conference presentations, contribution to policies created or updated, treatment guidelines written or updated, lectures or panels led, and participant in clinical trials and advisory boards) on the specified disease area (Table 1).
Ethical Approval
This study was designed in compliance with the standards of the professional association’s code of ethical conduct (GDPR, Insights Association, ESOMAR, GRBN, Intellus Worldwide, and country-specific privacy and data protection laws). This study did not involve patients or collect any patient information. This study was specifically designed to capture professional opinion.
Statistical Analysis
Descriptive statistics including number, percent, and means were calculated. Qualitative analyses of survey data on the reasons reported by specialists were performed in Excel using thematic coding.
Results
Primary/Initial Series COVID-19 Vaccinations
KOLs in each disease state panel across the EU were presented with a total of five statements focused on primary/initial series COVID-19 vaccinations. Generalized statements were modified to be specific for each disease state and further revised among KOLs during the Delphi panel to address disease-specific considerations. Statements addressing primary series COVID-19 vaccines for each disease area, the consensus reached among the KOLs, and the level of agreement obtained from physicians in the disease areas are presented in Table 2.
Overall, the statements are similar across disease states in that they address the increased risk of COVID-19 complications in these specific immunocompromised populations.
Disease-Specific COVID-19 Risk
KOLs for all four disease states reached a strong consensus indicating that patients with rheumatological conditions, renal disease, hematological malignancy, and SOTR are at a higher risk of hospitalization and death due to COVID-19 infection. Similarly, all surveyed physicians strongly agreed with the KOL consensus except for the rheumatologists who moderately agreed (70%). Some of the rheumatologists reported that disease burden was dependent on immunomodulator use, presence of comorbidities, and the risk status of an individual patient and as such they did not feel that risk can be generalized to the entire population of patients with rheumatic conditions.
Primary Series Safety
KOLs indicated moderate to strong consensus in the four disease areas. KOLs generally agreed that COVID-19 vaccines are safe and well tolerated among the disease-specific populations with strong consensus achieved in rheumatology and nephrology and moderate consensus in hematology and SOTR. All physicians surveyed agreed with the KOL consensus (76–88%), with a lower rating of agreement among transplant physicians (64%) who expressed uncertainty of risk with respect to vaccine-related adverse events in transplant recipients.
Need for Vaccination
KOLs for all four disease states indicated strong statement consensus. The statement recommends that immunocompromised patients should receive vaccinations for COVID-19 to reduce the risk of infection, lessen disease severity, and minimize complications. Physicians surveyed across the four disease states also strongly agreed with the consensus statements.
Number of Doses in Primary Series
KOL’s achieved strong consensus in three disease areas, with SOTR specialists reaching moderate consensus about the number of doses recommended for primary series COVID-19 vaccinations. Experts in rheumatology, hematology/oncology, and nephrology agreed it was appropriate to administer an extended primary series of three vaccines to disease-specific patients to reduce disease severity or complications. The surveyed physicians in rheumatology (74%), hematology (76%), and nephrology (84%) moderately to strongly agreed with the consensus of the panel experts, with no agreement among the transplant physicians (66%). Feedback provided by one transplant physician indicated that the three-dose primary series was too intense, and another transplant physician believed that the dosing and scheduling of the primary series in transplant recipients should take into account COVID-19 infection history.
Frequency of Doses in Primary Series
Strong consensus was achieved among KOLs concerning the vaccination schedule of COVID-19 primary series vaccines. However, there were slight differences in the consensus statement such that rheumatic conditions and SOTR recommend receiving two doses of COVID-19 vaccines 28 days apart, with the third dose administered 3–6 months after the second dose. Additionally, SOTR received a specific indication that the vaccine should not be administered in the first 2–4 weeks after initiating immunomodulatory medications. For renal and hematological conditions, the consensus statement recommends three doses of vaccines within 4–6 months, with each vaccine administered 28 days apart. Physicians surveyed in hematology (71%) and renal disease (74%) moderately agreed with the consensus statements. Physicians surveyed in rheumatology and solid organ transplant disagreed with the statements citing a lack of pre-existing established guidelines and evidence to support them.
COVID-19 Booster Vaccinations
KOLs in each disease state panel across the EU were presented up to four statements focused on COVID-19 booster vaccine considerations. Statements addressing booster series COVID-19 vaccines for each disease area, consensus reached among the KOLs, and the level of agreement obtained from physicians in the disease areas are presented in Table 3.
Booster Vaccine Safety
All four disease state KOLs indicated strong consensus. COVID-19 booster vaccines were recommended as safe and well tolerated by immunocompromised patients. Surveyed physicians indicated strong to moderate agreement in hematology/oncology (78%) and nephrology (86%). Rheumatology (58%) and transplant physicians (68%) did not agree with the consensus statement. Some of the concerns raised by the rheumatologists and transplant physicians included the safety of the COVID-19 booster in the immunocompromised population and its potential to elicit adverse events.
Need for Booster Vaccination
All four disease state KOLs indicated strong consensus on importance of booster vaccines in reducing the risk of infection and the potential to minimize severe outcomes. Strong to moderate agreement was reached in the physician survey in hematology (82%), nephrology (82%) and transplant physicians (78%). Physicians in rheumatology reported a lower level of agreement (68%). The reasons provided included that there was insufficient data of the efficacy of changing booster formulations was more effective or it was felt that new variants were prevalent too frequently to be certain.
Frequency of Booster Doses
All four disease state KOLs indicated moderate to strong consensus. KOLs in rheumatology and SOTR were aligned with the need for booster vaccines at 6–12-month intervals. KOLs in renal and hematology indicated moderate consensus. The timing varied between booster vaccines recommendations by disease states with recommendations by KOLs in hematology of “at least 6 months” (strong consensus) and rheumatology of “6–12 months” (moderate consensus). Renal disease and SOTR KOLs reached moderate and strong consensus, respectively, on a frequency of “every 12 months” for booster vaccine recommendation. There was no agreement among surveyed physicians for booster dose recommendations with rheumatologists (64%), hematologists/oncologists (55%), and transplant physicians (60%), whereas renal disease specialists agreed (78%). A lack of evidence, patient’s COVID-19 infection history, and severity of patient immunosuppression were most commonly cited as the contributing factors to the lack of agreement among physicians.
Boosters and COVID-19 Infection
Recommendations for booster vaccines in immunocompromised patients with past COVID-19 infection reached moderate to strong consensus in three of four disease states. KOLs in rheumatology and renal disease were aligned and strongly agreed with recommending the booster vaccine to reduce the risk of infection and severity of outcomes. KOL consensus was not achieved for SOTR. Among surveyed physicians, hematologists/oncologists (75%) and nephrologists (76%) reported agreement with consensus statements. Rheumatologists (62%) and transplant physicians (60%) were not in agreement with the expert panel. Reported reasons for the divergent opinion provided were that booster recommendations should be personalized to the individual patient based on previous COVID-19 infection status and serology.
Additional COVID-19 Vaccine Considerations
Four KOLs in each disease state panel across the EU were presented up to six statements that addressed additional considerations for COVID-19 vaccine recommendations. Statements addressing additional vaccine considerations for each disease area, consensus reached among the KOLs, and the level of agreement obtained from physicians in the disease areas are presented in Table 4.
Disease State-Specific Criteria
Statements with specific recommendations for vaccination tailored to considerations specific to the disease states were presented. KOLs indicated moderate to strong consensus.
For rheumatic conditions, the following statement did not reach consensus: A gap of 28 days in immunomodulatory treatment is recommended after COVID-19 vaccines to enhance their efficacy in patients with autoimmune inflammatory rheumatic disease.
The following statement for patients with hematologic malignancies reached moderate consensus among KOLs: Immunocompromised patients with hematological malignancies undergoing anti-CD20 antibody therapy can achieve higher seropositivity rates when the interval between therapy and vaccination exceeds 6 months.
The statement specific to SOTR patients reached a strong consensus among KOLs: SOTR are recommended to receive any COVID-19 vaccination at least 2 weeks before initiation of immunosuppressive therapy.
The statement for renal disease received differing recommendations by KOLs and was not tested in subsequent rounds of the Delphi panel.
Surveyed physicians did not agree with any of the above statements. The statement for renal disease was not tested in the survey.
Recommendation for mRNA Vaccines
Recommendations for mRNA vaccines over other vaccine platforms reached moderate to strong consensus in KOLs across all four disease states. Physicians surveyed among all disease states disagreed with the consensus statements and did not support the superiority of mRNA vaccines in the immunocompromised population (range, 44–64%). The cited reasons for the disagreement were most commonly a lack of data or evidence to support this statement.
Heterologous mRNA Vaccine Recommendation
With the recommendation for mRNA vaccines above, the question of whether to introduce mRNA vaccines if another vaccine platform was initiated in the primary series and whether patients should be switched to mRNA (heterologous) or whether subsequent vaccination should be consistent with the initial platform (homologous). Consensus was reached among KOLs in rheumatology and hematology (moderate) and renal disease (strong) with the recommendation to provide an mRNA vaccine in immunocompromised patients who were initiated with a non-mRNA vaccine regimen. SOTR KOLs failed to achieve consensus. Surveyed physicians across all disease states disagreed with the statements (range, 44–56%). The majority of physicians reported that they did not have pre-existing knowledge regarding the heterologous/homologous vaccine regimens.
Role of Measuring Antibody Titers
Testing of COVID-19 antibody titers may provide insight about the patient’s level of protection against infection and/or may be utilized to evaluate the need for booster vaccinations. KOLs in SOTR reached moderate consensus indicating that antibody titers can inform physician decision making. KOLs in rheumatology, hematology, and renal disease did not reach consensus. KOLs expressed concern that regular measurement of antibody titers was impractical, that the target titer level remained undetermined, and that specific resources may be lacking. Physicians surveyed across all disease states disagreed with the statements and did not advocate regular measurement of antibody titers (range, 32–60%). Most of the physicians alluded to impracticality of routine antibody titers measurement as not clinically realistic, not considered standard of care, or that there was little evidence to support this recommendation.
COVID-19 Vaccine Higher Dosing
Statements concerning the use of high-dose vaccines to provide greater protection were presented. Consensus was not achieved by the KOLs for any disease state panel. Some KOLs expressed caution about broadly recommending a higher-dose mRNA vaccine. Survey physicians did not agree with the statements (range, 24–40%) with the main reason provided as a lack of evidence that higher doses were indicative of clinical benefit.
Specific Guidelines Needed for Disease Area
A statement of the need for specific guidelines in each disease area was presented to KOLs. Moderate consensus was reached among KOLs in rheumatology and hematology and KOLs indicated believed disease-specific guidance for COVID-19 vaccinations would be beneficial for physicians. No consensus was reached on specific recommendations among renal disease KOLs. No statement was tested for SOTR. Physicians in all disease states did agree on a statement concerning disease-specific COVID-19 guidelines as necessary.
Discussion
In the current study, we utilized a Delphi panel approach to establish disease-specific recommendations for immunocompromised patients with rheumatological conditions, renal disease, hematologic malignancies, and SOTR. The reiterative process found that the primary/initial series and booster vaccination statements reached consensus across disease state panels. The process involved presentation of supporting evidence in a population of experts with research experience and clinical practice. KOLs in rheumatology, nephrology, and hematology achieved consensus for all nine statements pertaining to the primary and booster series with transplant physicians reaching consensus on eight of nine statements.
There was a strong consensus among KOLs that immunocompromised patients should receive a three-dose primary series of COVID-19 vaccines due to their high burden of disease in contrast with the two-dose primary series employed in the general population. KOLs considered COVID-19 vaccines to be safe, effective, and well tolerated by patients with rheumatological conditions, renal disease, hematologic malignancy, and solid organ transplant. Similarly, KOLs aligned with strong to moderate consensus regarding the safety of the COVID-19 booster and its necessity for the immunocompromised population. COVID-19 mRNA vaccines were preferred over other vaccine platforms (e.g., protein, IAV) for patients with autoimmune inflammatory rheumatic diseases, renal immunodeficiencies, hematologic malignancies, and SOT by all expert panels.
There was variance in ratings across all disease states regarding the role of boosters in hybrid immunity and specific timing of the booster vaccinations. KOLs in rheumatology and renal disease strongly agreed that patients with previous exposure to COVID-19 infection should be recommended to take a booster dose to reduce infection severity and outcomes. While KOLs in hematology and SOT had expressed the need for more robust data on previous COVID-19 exposure and its corresponding impact on immunity levels. Consensus was not reached by the SOT panel with some KOLs suggesting that they would recommend a booster if it targeted a variant different from the previous exposure. Different perceptions on the timing and frequency of booster doses also emerged. The rheumatology and SOT panels strongly agreed with the booster vaccination frequency statement. However, ratings obtained from KOLs in renal and hematology indicated moderate consensus. These KOLs suggested that exact intervals for boosters should not be pre-defined, as they should vary based upon external and internal factors relating to seasonality and concomitant medications. Similarly, the Centers for Disease Control and Prevention (CDC) in the United States acknowledges that immunosuppressive regimens may vary and states that clinical judgments regarding the timing of vaccination can be made outside the recommended dosing intervals. This aligns with physicians’ feedback that the vaccine dosing schedule largely depends on individual patients’ clinical profiles and treatment statuses.
Other vaccine considerations were addressed by statements pertaining to heterologous/ homologous mRNA booster vaccine recommendations, regular measurement of antibody titers, administration of higher doses of mRNA vaccines, and the need for disease-specific guidelines that were not recommended by the expert panels. Renal disease KOLs felt strongly that if a vaccine regimen is initiated with a non-mRNA vaccine, continuation with heterologous mRNA regimen is recommended to reduce potential severe disease complications. However, SOT KOLs were not in alignment with this recommendation for their patients. All panels expressed concern regarding the measurement of antibody titers except the SOT physicians who found this more feasible due to the frequency of antibody testing in transplant recipients. The other KOLs found that the healthcare system would incur additional costs and resources without any clear clinical benefit justifying regular measurement of antibody titers. The CDC also does not recommend antibody testing for the assessment of vaccine-mediated immune response and stated that it should not be used for vaccine decision-making. The expert panels were cautious to broadly recommend a higher-dose mRNA vaccine due to the lack of comparative effectiveness studies that assessed the value of differential dosing in increasing clinical benefit. Rheumatology and hematology KOLs agreed that disease-specific COVID-19 guidance would be beneficial for physicians, while nephrology experts felt that the risk of developing severe COVID-19 outcomes is individualized for each renal patient.
Overall, there was strong to moderate agreement among physicians surveyed with the KOL consensus statements pertaining to the primary COVID-19 vaccine series. Both providers and KOLs strongly agreed that there is a need for COVID-19 vaccinations across all four immunocompromised populations addressed. However, transplant physicians and rheumatologists did not agree with the expert panel on the timing of the administration of the three-dose primary series. Both transplant physicians and rheumatologists stressed the importance of immunomodulatory and immunosuppressive therapies and the need for their consideration when scheduling both primary series and boosters. Surveyed rheumatologists did not agree with consensus statements regarding COVID-19 boosters with the physicians citing a lack of evidence as the primary reason for disagreement. Most notably, rheumatologists, hematologists/oncologists, and transplant physicians agreed with the KOL panels opinion that mRNA COVID-19 vaccines are the most effective in immunocompromised individuals.
Large variances in agreement were seen between practicing specialists and KOLs underscoring the need for education and guidance. Through the qualitative portion of the study, we were able to address knowledge gaps and address concerns with the provision of further supporting evidence. The most common reason cited for a lack of agreement among physicians with consensus statements generated by KOLs was insufficient evidence. However, due to the difference in approach wherein the physician survey was conducted at a single point in time and no feedback was provided to them, it may be that they were not aware of the evidence available. The iterative process and opportunity to provide and evaluate supporting evidence by the panel allowed for revision to statements such that agreement could be reached. These interactions were not possible for the large survey. Several surveyed specialists admitted they lacked knowledge or were not certain regarding the specific use of mRNA vaccines in the immunocompromised population and the implementation of a heterologous mRNA vaccine after initiation of a non-mRNA vaccine. Despite knowledge gaps, practicing specialists did not feel disease-specific guidance would be beneficial. One of the strengths of this study is its use of Delphi methodology. Each subsequent round of KOL interaction allowed for incorporation of KOL feedback and to refine statement recommendations, increasing the degree of consensus and, in some cases, reaching unanimity. Delphi panel participants were able to offer anonymous responses during the group process. This study was conducted among a diverse group of experts across Europe.
One limitation of our study was the lack of inclusion of any statements regarding the role of monoclonal antibodies in the prevention of COVID-19 in the immunocompromised population. Given that immunocompromised patients may have inadequate immune response after COVID-19 vaccination, passive immunization with preformed antibodies can potentially support an immune defense. Monoclonal antibody therapies are complementary to vaccines as part of an overall therapeutic approach. Vaccine immunity usually has slower uptake, providing protection after a few weeks while monoclonal antibodies are faster acting with the potential to provide months of immune assistance, hence likely beneficial in both prevention and treatment.
Although the Delphi method is a robust approach to assessing the levels of agreement, it is not without limitations. A main concern pertains to the construction of a truly representative expert panel. Our selection of KOLs was primarily based on strong clinical expertise and extensive research engagement. The literature in this area is rapidly evolving. No formal systematic review with stringent criteria for levels of evidence was performed owing to the sheer volume of COVID-19-related published studies and the frequency at which they were and continue to be published. However, a targeted literature review was conducted to gather evidence published after January 1, 2022, that addressed COVID-19 vaccinations in the specific immunocompromised populations relevant to the initial statement items. We sought region-specific evidence for European populations, but this was not always available and was substituted with the highest level of evidence possible.
Conclusions
Our multidisciplinary panel’s emphasis on actionable, near-term recommendations guided the Delphi consensus-building process and increased the relevance of the study’s findings to a broad group of stakeholders. Our goal was to provide guidance to providers on the use of COVID-19 vaccines and boosters for patients with immunocompromised conditions. The mRNA vaccine was a novel development at the onset of the COVID-19 pandemic, and considerations for vaccines developed on this platform may differ from other vaccines. Our findings suggest that KOLs felt the mRNA vaccines may be superior to other types of vaccines when used in the immunocompromised population. This study emphasizes the need of COVID-19 vaccines, including supplemental/booster dosing for patients across all four immunocompromised disease areas (i.e., rheumatologic disease, renal disease, hematological malignancy, and solid organ transplant recipients) Findings of this study are intended to aid in the care of individual patients but not to replace personalized care or diminish shared decision-making with patients. As new safety and efficacy evidence becomes available for COVID-19 vaccines, this document is intended to be updated and expanded as the literature evolves.
Data Availability
All data generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907–18.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.
Elkrief A, Desilets A, Papneja N, Cvetkovic L, Groleau C, Lakehal YA, et al. High mortality among hospital-acquired COVID-19 infection in patients with cancer: a multicentre observational cohort study. Eur J Cancer. 2020;139:181–7.
Lievre A, Turpin A, Ray-Coquard I, Le Malicot K, Thariat J, Ahle G, et al. Risk factors for Coronavirus Disease 2019 (COVID-19) severity and mortality among solid cancer patients and impact of the disease on anticancer treatment: A French nationwide cohort study (GCO-002 CACOVID-19). Eur J Cancer. 2020;141:62–81.
de Joode K, Dumoulin DW, Tol J, Westgeest HM, Beerepoot LV, van den Berkmortel F, et al. Dutch Oncology COVID-19 consortium: Outcome of COVID-19 in patients with cancer in a nationwide cohort study. Eur J Cancer. 2020;141:171–84.
Saini KS, Tagliamento M, Lambertini M, McNally R, Romano M, Leone M, et al. Mortality in patients with cancer and coronavirus disease 2019: A systematic review and pooled analysis of 52 studies. Eur J Cancer. 2020;139:43–50.
Caillard S, Chavarot N, Francois H, Matignon M, Greze C, Kamar N, et al. Is COVID-19 infection more severe in kidney transplant recipients? Am J Transpl. 2021;21(3):1295–303.
Couchoud C, Bayer F, Ayav C, Bechade C, Brunet P, Chantrel F, et al. Low incidence of SARS-CoV-2, risk factors of mortality and the course of illness in the French national cohort of dialysis patients. Kidney Int. 2020;98(6):1519–29.
Raja MA, Mendoza MA, Villavicencio A, Anjan S, Reynolds JM, Kittipibul V, et al. COVID-19 in solid organ transplant recipients: A systematic review and meta-analysis of current literature. Transpl Rev (Orlando). 2021;35(1): 100588.
Tian Y, Qiu X, Wang C, Zhao J, Jiang X, Niu W, et al. Cancer associates with risk and severe events of COVID-19: A systematic review and meta-analysis. Int J Cancer. 2021;148(2):363–74.
Hilbrands LB, Duivenvoorden R, Vart P, Franssen CFM, Hemmelder MH, Jager KJ, et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol Dial Transpl. 2020;35(11):1973–83.
Consortium FRSSSCI C. Severity of COVID-19 and survival in patients with rheumatic and inflammatory diseases: data from the French RMD COVID-19 cohort of 694 patients. Ann Rheum Dis. 2021;80(4):527–38.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16.
Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet. 2021;397(10277):881–91.
Sadoff J, Gray G, Vandebosch A, Cardenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201.
Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia. Lancet. 2021;397(10275):671–81.
Heath PT, Galiza EP, Baxter DN, Boffito M, Browne D, Burns F, et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021;385(13):1172–83.
Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397(10287):1819–29.
Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412–23.
Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, et al. Effect of 2 inactivated SARS-CoV-2 vaccines on symptomatic COVID-19 infection in adults: a randomized clinical trial. JAMA. 2021;326(1):35–45.
Tanriover MD, Doganay HL, Akova M, Guner HR, Azap A, Akhan S, et al. Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey. Lancet. 2021;398(10296):213–22.
Kelly JD, Leonard S, Hoggatt KJ, Boscardin WJ, Lum EN, Moss-Vazquez TA, et al. Incidence of severe COVID-19 illness following vaccination and booster with BNT162b2, mRNA-1273, and Ad26.COV2.S vaccines. JAMA. 2022;328(14):1427–37.
Open SC, Parker EPK, Horne EMF, Hulme WJ, Tazare J, Zheng B, et al. Comparative effectiveness of two- and three-dose COVID-19 vaccination schedules involving AZD1222 and BNT162b2 in people with kidney disease: a linked OpenSAFELY and UK Renal Registry cohort study. Lancet Reg Health Eur. 2023;30: 100636.
Mehrabi Nejad MM, Shobeiri P, Dehghanbanadaki H, Tabary M, Aryannejad A, Haji Ghadery A, et al. Seroconversion following the first, second, and third dose of SARS-CoV-2 vaccines in immunocompromised population: a systematic review and meta-analysis. Virol J. 2022;19(1):132.
Mojadadi MS, Javadinia SA, Attarian F, Samami E, Sobhani M. Anti-SARS-CoV-2 spike IgG following injection of the third dose vaccine: A systematic review with meta-analysis of heterologous versus homologous vaccination. Front Public Health. 2022;10: 960598.
Benning L, Morath C, Bartenschlager M, Kim H, Reineke M, Beimler J, et al. Neutralizing antibody response against the B.1.617.2 (delta) and the B.1.1.529 (omicron) variants after a third mRNA SARS-CoV-2 vaccine dose in kidney transplant recipients. Am J Transplant. 2022;22(7):1873–83.
Embi PJ, Levy ME, Naleway AL, Patel P, Gaglani M, Natarajan K, et al. Effectiveness of 2-Dose Vaccination with mRNA COVID-19 Vaccines Against COVID-19-Associated Hospitalizations Among Immunocompromised Adults - Nine States, January-September 2021. MMWR Morb Mortal Wkly Rep. 2021;70(44):1553–9.
Mues KE, Kirk B, Patel DA, Gelman A, Chavers LS, Talarico CA, et al. Real-world comparative effectiveness of mRNA-1273 and BNT162b2 vaccines among immunocompromised adults identified in administrative claims data in the United States. Vaccine. 2022;40(47):6730–9.
Lee A, Wong SY, Chai LYA, Lee SC, Lee MX, Muthiah MD, et al. Efficacy of COVID-19 vaccines in immunocompromised patients: systematic review and meta-analysis. BMJ. 2022;376: e068632.
Wang X, Haeussler K, Spellman A, Phillips LE, Ramiller A, Bausch-Jurken MT, et al. Comparative effectiveness of mRNA-1273 and BNT162b2 COVID-19 vaccines in immunocompromised individuals: a systematic review and meta-analysis using the GRADE framework. Front Immunol. 2023;14:1204831.
Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 4. Arthritis Rheumatol. 2022;74(5):e21–36.
Gatti M, Rinaldi M, Bussini L, Bonazzetti C, Pascale R, Pasquini Z, et al. Clinical outcome in solid organ transplant recipients affected by COVID-19 compared to general population: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28(8):1057–65.
Overvad M, Koch A, Jespersen B, Gustafsson F, Krause TG, Hansen CH, et al. Outcomes following SARS-CoV-2 infection in individuals with and without solid organ transplantation-A Danish nationwide cohort study. Am J Transpl. 2022;22(11):2627–36.
Kamar N, Abravanel F, Marion O, Couat C, Izopet J, Del Bello A. Three doses of an mRNA Covid-19 vaccine in solid-organ transplant recipients. N Engl J Med. 2021;385(7):661–2.
Lane S, Yeomans A, Shakir S. Systematic review of spontaneous reports of myocarditis and pericarditis in transplant recipients and immunocompromised patients following COVID-19 mRNA vaccination. BMJ Open. 2022;12(7): e060425.
Sanders JF, Bemelman FJ, Messchendorp AL, Baan CC, van Baarle D, van Binnendijk R, et al. The RECOVAC Immune-response Study: the immunogenicity, tolerability, and safety of COVID-19 vaccination in patients with chronic kidney disease, on dialysis, or living with a kidney transplant. Transplantation. 2022;106(4):821–34.
Mehrabi Nejad MM, Moosaie F, Dehghanbanadaki H, Haji Ghadery A, Shabani M, Tabary M, et al. Immunogenicity of COVID-19 mRNA vaccines in immunocompromised patients: a systematic review and meta-analysis. Eur J Med Res. 2022;27(1):23.
Tenforde MW, Patel MM, Ginde AA, Douin DJ, Talbot HK, Casey JD, et al. Effectiveness of severe acute respiratory syndrome coronavirus 2 messenger RNA vaccines for preventing coronavirus disease 2019 hospitalizations in the United States. Clin Infect Dis. 2022;74(9):1515–24.
Au WY, Cheung PP. Effectiveness of heterologous and homologous COVID-19 vaccine regimens: living systematic review with network meta-analysis. BMJ. 2022;377:e069989.
Kabbani D, Yotis DM, Ferreira VH, Shalhoub S, Belga S, Tyagi V, et al. Immunogenicity, safety, and breakthrough severe acute respiratory syndrome coronavirus 2 infections after Coronavirus Disease 2019 vaccination in organ transplant recipients: a prospective multicenter Canadian study. Open Forum Infect Dis. 2023;10(5):ofad200.
Moolgavkar SH, Moller H, Woodward A. Principles of the epidemiological approach to QEP. IARC Sci Publ. 1999;131:61–73.
Osmanodja B, Ronicke S, Budde K, Jens A, Hammett C, Koch N, et al. Serological response to three, four and five doses of SARS-CoV-2 vaccine in kidney transplant recipients. J Clin Med. 2022;11(9).
Terbinafine is best treatment for fungal nail infection. BMJ. 1999;318(7190):B.
Ferreira VH, Ierullo M, Mavandadnejad F, Kurtesi A, Hu Q, Hardy WR, et al. Omicron BA.4/5 neutralization and t-cell responses in organ transplant recipients after booster messenger RNA vaccine: a multicenter cohort study. Clin Infect Dis. 2023;77(2):229–36.
Schietzel S, Anderegg M, Limacher A, Born A, Horn MP, Maurer B, et al. Humoral and cellular immune responses on SARS-CoV-2 vaccines in patients with anti-CD20 therapies: a systematic review and meta-analysis of 1342 patients. RMD Open. 2022;8(1).
Hovd M, Asberg A, Munthe LA, Heldal K, Reisaeter AV, Vaage JT, et al. Humoral vaccine response and breakthrough infections in kidney transplant recipients during the COVID-19 pandemic: a nationwide cohort study. EClinicalMedicine. 2023;60: 102035.
Taheri S. Efficacy and safety of booster vaccination against SARS-CoV-2 in dialysis and renal transplant patients: systematic review and meta-analysis. Int Urol Nephrol. 2023;55(4):791–802.
Teh JSK, Coussement J, Neoh ZCF, Spelman T, Lazarakis S, Slavin MA, et al. Immunogenicity of COVID-19 vaccines in patients with hematologic malignancies: a systematic review and meta-analysis. Blood Adv. 2022;6(7):2014–34.
Piechotta V, Mellinghoff SC, Hirsch C, Brinkmann A, Iannizzi C, Kreuzberger N, et al. Effectiveness, immunogenicity, and safety of COVID-19 vaccines for individuals with hematological malignancies: a systematic review. Blood Cancer J. 2022;12(5):86.
Noori M, Azizi S, Abbasi Varaki F, Nejadghaderi SA, Bashash D. A systematic review and meta-analysis of immune response against first and second doses of SARS-CoV-2 vaccines in adult patients with hematological malignancies. Int Immunopharmacol. 2022;110: 109046.
Rinaldi I, Pratama S, Wiyono L, Tandaju JR, Wardhana IL, Winston K. Efficacy and safety profile of COVID-19 mRNA vaccine in patients with hematological malignancies: systematic review and meta-analysis. Front Oncol. 2022;12: 951215.
Chuleerarux N, Manothummetha K, Moonla C, Sanguankeo A, Kates OS, Hirankarn N, et al. Immunogenicity of SARS-CoV-2 vaccines in patients with multiple myeloma: a systematic review and meta-analysis. Blood Adv. 2022;6(24):6198–207.
Ku JH, Sy LS, Qian L, Ackerson BK, Luo Y, Tubert JE, et al. Vaccine effectiveness of the mRNA-1273 3-dose primary series against COVID-19 in an immunocompromised population: a prospective observational cohort study. Vaccine. 2023;41(24):3636–46.
Mai AS, Lee A, Tay RYK, Shapiro L, Thakkar A, Halmos B, et al. Booster doses of COVID-19 vaccines for patients with haematological and solid cancer: a systematic review and individual patient data meta-analysis. Eur J Cancer. 2022;172:65–75.
Gong IY, Vijenthira A, Betschel SD, Hicks LK, Cheung MC. COVID-19 vaccine response in patients with hematologic malignancy: a systematic review and meta-analysis. Am J Hematol. 2022;97(4):E132–5.
Pinana JL, Martino R, Vazquez L, Lopez-Corral L, Perez A, Chorao P, et al. SARS-CoV-2-reactive antibody waning, booster effect and breakthrough SARS-CoV-2 infection in hematopoietic stem cell transplant and cell therapy recipients at one year after vaccination. Bone Marrow Transpl. 2023;58(5):567–80.
Ito Y, Honda A, Kurokawa M. COVID-19 mRNA vaccine in patients with lymphoid malignancy or anti-CD20 antibody therapy: a systematic review and meta-analysis. Clin Lymphoma Myeloma Leuk. 2022;22(8):e691–707.
Chu C, Schonbrunn A, Fischer D, Liu Y, Hocher JG, Weinerth J, et al. Immune response of heterologous versus homologous prime-boost regimens with adenoviral vectored and mRNA COVID-19 vaccines in immunocompromised patients. Front Immunol. 2023;14:1187880.
Risk M, Hayek SS, Schiopu E, Yuan L, Shen C, Shi X, et al. COVID-19 vaccine effectiveness against omicron (B.1.1.529) variant infection and hospitalisation in patients taking immunosuppressive medications: a retrospective cohort study. Lancet Rheumatol. 2022;4(11):e775-e84.
Thakur B, Dubey P, Benitez J, Torres JP, Reddy S, Shokar N, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep. 2021;11(1):8562.
Ng WH, Tipih T, Makoah NA, Vermeulen JG, Goedhals D, Sempa JB, et al. Comorbidities in SARS-CoV-2 patients: a systematic review and meta-analysis. mBio. 2021;12(1).
Li X, Zhong X, Wang Y, Zeng X, Luo T, Liu Q. Clinical determinants of the severity of COVID-19: a systematic review and meta-analysis. PLoS ONE. 2021;16(5): e0250602.
Zitt E, Davidovic T, Schimpf J, Abbassi-Nik A, Mutschlechner B, Ulmer H, et al. The Safety and Immunogenicity of the mRNA-BNT162b2 SARS-CoV-2 Vaccine in Hemodialysis Patients. Front Immunol. 2021;12: 704773.
Frittoli M, Cassia M, Barassi A, Ciceri P, Galassi A, Conte F, et al. Efficacy and safety of COVID-19 vaccine in patients on renal replacement therapy. Vaccines (Basel). 2022;10(9).
Quiroga B, Soler MJ, Ortiz A, Martinez Vaquera S, Jarava Mantecon CJ, Useche G, et al. Safety and immediate humoral response of COVID-19 vaccines in chronic kidney disease patients: the SENCOVAC study. Nephrol Dial Transpl. 2022;37(10):1868–78.
Ozturk S, Turgutalp K, Arici M, Odabas AR, Altiparmak MR, Aydin Z, et al. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrol Dial Transpl. 2020;35(12):2083–95.
Affeldt P, Koehler FC, Brensing KA, Gies M, Platen E, Adam V, et al. Immune response to third and fourth COVID-19 vaccination in hemodialysis patients and kidney transplant recipients. Viruses. 2022;14(12).
Melin J, Svensson MK, Albinsson B, Winqvist O, Pauksens K. A third dose SARS‑CoV‑2 BNT162b2 mRNA vaccine results in improved immune response in hemodialysis patients. Ups J Med Sci. 2022;127.
Haarhaus M, Duhanes M, Lesevic N, Matei B, Ramsauer B, Da Silva RR, et al. Improved immunologic response to COVID-19 vaccine with prolonged dosing interval in haemodialysis patients. Scand J Immunol. 2022;95(5): e13152.
Espi M, Charmetant X, Barba T, Mathieu C, Pelletier C, Koppe L, et al. A prospective observational study for justification, safety, and efficacy of a third dose of mRNA vaccine in patients receiving maintenance hemodialysis. Kidney Int. 2022;101(2):390–402.
Verdier JF, Boyer S, Chalmin F, Jeribi A, Egasse C, Maggi MF, et al. Response to three doses of the Pfizer/BioNTech BNT162b2 COVID-19 vaccine: a retrospective study of a cohort of haemodialysis patients in France. BMC Nephrol. 2022;23(1):189.
Fucci A, Giacobbe S, Guerriero I, Suzumoto Y, D’Andrea EL, Scrima M, et al. The DiaCoVAb study in South Italy: immune response to SARS-CoV-2 vaccination in dialysis patients. Kidney Blood Press Res. 2022;47(7):467–74.
Quiroga B, Soler MJ, Ortiz A, Gansevoort RT, Leyva A, Rojas J, et al. Long-term dynamic humoral response to SARS-CoV-2 mRNA vaccines in patients on peritoneal dialysis. Vaccines (Basel). 2022;10(10).
Beilhack G, Monteforte R, Frommlet F, Reindl-Schwaighofer R, Strassl R, Vychytil A. Humoral response to mRNA-1273 SARS-CoV-2 vaccine in peritoneal dialysis patients: Is boostering after six months adequate? Front Med (Lausanne). 2022;9: 905798.
Berar-Yanay N, Freiman S, Shapira M, Saffoury A, Elemy A, Hamze M, et al. Waning humoral response 3 to 6 months after vaccination with the SARS-COV-2 BNT162b2 mRNA vaccine in dialysis patients. J Clin Med. 2021;11(1).
Buchwinkler L, Solagna CA, Messner J, Pirklbauer M, Rudnicki M, Mayer G, et al. Antibody response to mRNA vaccines against SARS-CoV-2 with chronic kidney disease, hemodialysis, and after kidney transplantation. J Clin Med. 2021;11(1).
Mohseni Afshar Z, Babazadeh A, Janbakhsh A, Mansouri F, Sio TT, Sullman MJM, et al. Coronavirus disease 2019 (Covid-19) vaccination recommendations in special populations and patients with existing comorbidities. Rev Med Virol. 2022;32(3): e2309.
Lesny P, Anderson M, Cloherty G, Stec M, Haase-Fielitz A, Haarhaus M, et al. Immunogenicity of a first dose of mRNA- or vector-based SARS-CoV-2 vaccination in dialysis patients: a multicenter prospective observational pilot study. J Nephrol. 2021;34(4):975–83.
Mrak D, Sieghart D, Simader E, Tobudic S, Radner H, Mandl P, et al. Heterologous vector versus homologous mRNA COVID-19 booster vaccination in non-seroconverted immunosuppressed patients: a randomized controlled trial. Nat Commun. 2022;13(1):5362.
Manley HJ, Li NC, Aweh GN, Hsu CM, Weiner DE, Miskulin D, et al. SARS-CoV-2 vaccine effectiveness and breakthrough infections among patients receiving maintenance dialysis. Am J Kidney Dis. 2023;81(4):406–15.
Grainger R, Kim AHJ, Conway R, Yazdany J, Robinson PC. COVID-19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol. 2022;18(4):191–204.
Joudeh AI, Lutf AQ, Mahdi S, Tran G. Efficacy and safety of mRNA and AstraZeneca COVID-19 vaccines in patients with autoimmune rheumatic diseases: a systematic review. Vaccine. 2023;41(26):3801–12.
Sood A, Tran M, Murthy V, Gonzalez E. Immunogenicity and safety of SARS-CoV-2 vaccination in patients with rheumatic diseases: a systematic review and meta-analysis. J Clin Rheumatol. 2022;28(8):381–9.
Conway R, Grimshaw AA, Konig MF, Putman M, Duarte-Garcia A, Tseng LY, et al. SARS-CoV-2 infection and COVID-19 outcomes in rheumatic diseases: a systematic literature review and meta-analysis. Arthritis Rheumatol. 2022;74(5):766–75.
Kartnig F, Mrak D, Simader E, Tobudic S, Radner H, Mandl P, et al. Safety and immunogenicity of a third COVID-19 vaccination in patients with immune-mediated inflammatory diseases compared with healthy controls. Ann Rheum Dis. 2023;82(2):292–300.
Wieske L, van Dam KPJ, Steenhuis M, Stalman EW, Kummer LYL, van Kempen ZLE, et al. Humoral responses after second and third SARS-CoV-2 vaccination in patients with immune-mediated inflammatory disorders on immunosuppressants: a cohort study. Lancet Rheumatol. 2022;4(5):e338–50.
Bjorlykke KH, Orbo HS, Tveter AT, Jyssum I, Sexton J, Tran TT, et al. Four SARS-CoV-2 vaccine doses or hybrid immunity in patients on immunosuppressive therapies: a Norwegian cohort study. Lancet Rheumatol. 2023;5(1):e36–46.
Tan SYS, Yee AM, Sim JJL, Lim CC. COVID-19 vaccination in systemic lupus erythematosus: a systematic review of its effectiveness, immunogenicity, flares and acceptance. Rheumatology (Oxford). 2023;62(5):1757–72.
Acknowledgements
We would like to thank all of the disease experts and physicians who participated in the Delphi panel and the online survey.
Funding
A grant (Grant number: 7700053394) was obtained by ICON for this study from Moderna Inc. To avoid any conflict of interest, per terms of grants agreement, Moderna only provided high-level input on the populations of interest and the general need for guidelines. Moderna was not involved in the design, conduct of the study, interpretation of results or writing of this manuscript. ICON team independently from Moderna determined the focus of the surveys and interviews and generated the summary statements; was responsible for selecting the KOLs; was responsible for creating inclusion/exclusion of final panel members; conducted data collection and interviews; facilitated the process of the Delphi panel and developed the manuscripts. The journal’s Rapid Service Fee was paid for by the study grant.
Author information
Authors and Affiliations
Contributions
Samantha Kimball-Carroll and Joseph Brown, were involved in study conception and design. Material preparation and interpretation of results were performed by Kira Zhi Hua Lai, Jaya Paranilam, Joseph Brown, and Samantha Kimball-Carroll. Francesco Arcioni, and Antonio Franco participated in the Delphi panel. The manuscript was drafted by Jaya Paranilam and Samantha Kimball-Carroll. All authors commented on drafts of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Kira Zhi Hua Lai, Jaya Paranilam, Joseph Brown, and Samantha Kimball-Carroll are employed by ICON Plc and have previously worked with Moderna Inc. Francesco Arcioni and Antonio Franco have nothing to disclose.
Ethical Approval
This study was designed in compliance with the standards of the professional associations code of ethical conduct (GDPR, Insights Association, ESOMAR, GRBN, Intellus Worldwide, and country-specific privacy and data protection laws). This study did not involve patients or collect any patient information. This study was specifically designed to capture professional opinion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Paranilam, J., Arcioni, F., Franco, A. et al. Delphi Panel Consensus Statement Generation: COVID-19 Vaccination Recommendations for Immunocompromised Populations in the European Union. Infect Dis Ther 13, 2227–2253 (2024). https://doi.org/10.1007/s40121-024-01051-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-01051-9