Abstract
Background
The impact of coronavirus disease 2019 (COVID-19) on postoperative recovery from oncology surgeries should be understood for the clinical decision-making. Therefore, this study was designed to evaluate the postoperative cumulative 28-day mortality and the morbidity of surgical oncology patients during the COVID-19 pandemic.
Methods
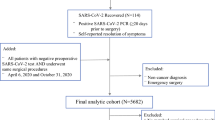
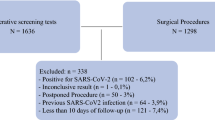
This retrospective cohort study included patients consecutively admitted to intensive care units (ICU) of three centres for postoperative care of oncologic surgeries between March to June 2019 (first phase) and March to June 2020 (second phase). The primary outcome was cumulative 28-day postoperative mortality. Secondary outcomes were postoperative organic dysfunction and the incidence of clinical complications. Because of the possibility of imbalance between groups, adjusted analyses were performed: Cox proportional hazards model (primary outcome) and multiple logistic regression model (secondary outcomes).
Results
After screening 328 patients, 291 were included. The proportional hazard of cumulative 28-day mortality was higher in the second phase than that in the first phase in the Cox model, with the adjusted hazard ratio of 4.35 (95% confidence interval [CI] 2.15–8.82). The adjusted incidences of respiratory complications (odds ratio [OR] 5.35; 95% CI 1.42–20.11) and pulmonary infections (OR 1.53; 95% CI 1.08–2.17) were higher in the second phase. However, the adjusted incidence of other infections was lower in the second phase (OR 0.78; 95% CI 0.67–0.91).
Conclusions
Surgical oncology patients who underwent postoperative care in the intensive care unit during the COVID-19 pandemic had higher hazard of 28-day mortality. Furthermore, these patients had higher odds of respiratory complications and pulmonary infections.
Trials registration The study is registered in the Brazilian Registry of Clinical Trials under the code RBR-8ygjpqm, UTN code U1111-1293-5414.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
Data used in the analysis of the study may be made available through a request to the corresponding author.
References
Iacobucci G. Covid-19: all nonurgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. https://doi.org/10.1136/bmj.m1106.
Erol T, Mahmudzada K, Kirimtay B, Doğu D, Oruç M, Yorganci K. Effect of COVİD-19 pandemic on general surgery practice and resident education. Acta Med Mediterr. 2021;37(6):3069–74. https://doi.org/10.19193/0393-6384_2021_6_481.
Bajunaid K, Alqurashi A, Alatar A, et al. Neurosurgical procedures and safety during the COVID-19 pandemic: a case-control multicenter study. World Neurosurg. 2020;143:e179–87. https://doi.org/10.1016/j.wneu.2020.07.093.
de Bock E, Herman ES, Bastian OW, Filipe MD, Vriens MR, Richir MC. Systematic review and meta-analysis determining the effect of implemented COVID-19 guidelines on surgical oncology volumes and clinical outcomes. Surg Oncol. 2022. https://doi.org/10.1016/j.suronc.2022.101859.
Coccolini F, Perrone G, Chiarugi M, et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020. https://doi.org/10.1186/s13017-020-00307-2.
Bhangu A, Nepogodiev D, Glasbey JC, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. https://doi.org/10.1016/S0140-6736(20)31182-X.
Leal J, O’Grady HM, Armstrong L, et al. Patient and ward related risk factors in a multi-ward nosocomial outbreak of COVID-19: outbreak investigation and matched case–control study. Antimicrob Resist Infect Control. 2023. https://doi.org/10.1186/s13756-023-01215-1.
Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31(8):1065–74. https://doi.org/10.1016/j.annonc.2020.05.009.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis.related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10.
Silva JM, De Freitas Chaves RC, Corrêa TD, et al. Epidemiology and outcome of high-surgical-risk patients admitted to an intensive care unit in Brazil. Rev Bras Ter Intensiva. 2020;32(1):17–27. https://doi.org/10.5935/0103-507X.20200005.
Metnitz PGH, Moreno RP, Almeida E, et al. SAPS 3-from evaluation of the patient to evaluation of the intensive care unit. Part 1: objectives, methods and cohort description. Intensive Care Med. 2005;31(10):1336–44. https://doi.org/10.1007/s00134-005-2762-6.
Silva Junior JM, Malbouisson LMS, Nuevo HL, et al. Applicability of the Simplified Acute Physiology Score (SAPS 3) in Brazilian hospitals. Rev Bras Anestesiol. 2010;60(1):26–31.
Koo CY, Hyder JA, Wanderer JP, Eikermann M, Ramachandran SK. A meta-analysis of the predictive accuracy of postoperative mortality using the american society of anesthesiologists’ physical status classification system. World J Surg. 2015;39(1):88–103. https://doi.org/10.1007/s00268-014-2783-9.
Tennant PWG, Murray EJ, Arnold KF, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620–32. https://doi.org/10.1093/ije/dyaa213.
Wu S, Liu W, Zhang M, et al. Preventive measures significantly reduced the risk of nosocomial infection in elderly inpatients during the COVID-19 pandemic. Exp Ther Med. 2022. https://doi.org/10.3892/etm.2022.11499.
Bhangu A, Lawani I, Ng-Kamstra JS, et al. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107(9):1097–103. https://doi.org/10.1002/bjs.11646.
Nepogodiev D, Omar OM, Glasbey JC, et al. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440–9. https://doi.org/10.1002/bjs.11746.
Glasbey JC, Nepogodiev D, Simoes JF, et al. Elective cancer surgery in COVID-19–free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol. 2020;39(1):66–78. https://doi.org/10.1200/JCO.20.01933.
Wilcox ME, Rowan KM, Harrison DA, Doidge JC. Does unprecedented ICU capacity strain, as experienced during the COVID-19 pandemic, impact patient outcome? Crit Care Med. 2022;50(6):e548–56. https://doi.org/10.1097/ccm.0000000000005464.
Demoule A, Fartoukh M, Louis G, et al. ICU strain and outcome in COVID-19 patients: a multicenter retrospective observational study. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0271358.
Leung E, Pervaiz Z, Lowe-Zinola J, et al. Maintaining surgical care delivery during the COVID-19 pandemic: a comparative cohort study at a tertiary gynecological cancer centre. Gynecol Oncol. 2021;160(3):649–54. https://doi.org/10.1016/j.ygyno.2020.12.013.
Akhtar N, Rajan S, Chakrabarti D, et al. Continuing cancer surgery through the first six months of the COVID-19 pandemic at an academic university hospital in India: a lower-middle-income country experience. J Surg Oncol. 2021;123(5):1177–87. https://doi.org/10.1002/jso.26419.
Blache G, El Hajj H, Jauffret C, et al. Care as usual: an acceptable strategy to apply during the COVID-19 pandemic in a French tertiary gynaecologic oncology department. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.653009.
Vanni G, Pellicciaro M, Materazzo M, et al. Awake breast cancer surgery: strategy in the beginning of COVID-19 emergency. Breast Cancer. 2021;28(1):137–44. https://doi.org/10.1007/s12282-020-01137-5.
Santambrogio R, Farina G, D’Alessandro V, Iacob G, Gemma M, Zappa MA. Guidelines adaptation to the COVID-19 outbreak for the management of hepatocellular carcinoma. J Laparoendosc Adv Surg Tech. 2021;31(3):266–72. https://doi.org/10.1089/lap.2020.0559.
Acknowledgment
Authorship: FSLV: analysis and interpretation of data and writing of the manuscript; LLN: data acquisition and review of the manuscript for important scientific content; RT: data acquisition and review of the manuscript for important scientific content; APNJ: analysis and interpretation of data and review of the manuscript for important scientific content; JHFP: data acquisition and review of the manuscript for important scientific contents; RAJS: data acquisition and review of the manuscript for important scientific content; FPS: data acquisition and review of the manuscript for important scientific content; DR: data acquisition and review of the manuscript for important scientific content; BDBM: data acquisition and interpretation and review of the manuscript for important scientific content; LDD: data acquisition and interpretation and review of the manuscript for important scientific content; LMSM: data acquisition and interpretation and review of the manuscript for important scientific contents; URJ: data interpretation and review of the manuscript for important scientific content; and JMSJ: conception, design, data analysis and interpretation and writing of the manuscript. All authors approved the final manuscript and voted for publication. The study was not pre-registered in an independent registry.
Funding
The funding source had no role in the study design, conduction, or analysis. Funding was provided by A. C. Camargo Cancer Center, Faculdade de Medicina da Universidade de São Paulo, and Hospital de Câncer de Barretos.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors declare to have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vianna, F.S.L., Neves, L.L., Testa, R. et al. Impact of the COVID-19 Pandemic on the Outcomes of Patients Undergoing Oncological Surgeries: CORONAL Study. Ann Surg Oncol 31, 3639–3648 (2024). https://doi.org/10.1245/s10434-024-15152-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-024-15152-9