Abstract
The aim of this study was to investigate the impact of the COVID-19 pandemic on pelvic trauma surgery in Poland. This study comprises 132 consecutive patients admitted for pelvic fracture surgery from 2019 to 2022, separating them into 2 groups; pre-COVID (1 year before the outbreak of pandemic − 2019) and COVID period (in Poland 2020–2022). The data was collected respectively in a single trauma center. Demographic data was collected, additionally, the type of fracture according to Young-Burgess and Letournel-Judet classification system, date of the injury and surgery, the surgical approach and stabilization methods, mechanism of trauma, concomitant injuries, body mass index (BMI), blood transfusions, number of days spent in the hospital, and surgery duration. Patients during the pandemic had statistically significantly shorter duration of hospital stay, and lesser amount of blood units transfused comparing to the non- pandemic group, 4.50 days vs. 6.90 days (p < 0.001) and 1.20 units vs. 1.40 units (p = 0.0401) respectively. Patients with acetabulum fractures required more blood transfusion units (p < 0.0001), comparing to those with pelvic ring injuries. Moreover, the acetabulum fractures were more time demanding comparing to pelvic ring injury (151 min vs. 128 min, respectively) (p < 0.0001) as well as length of hospital stay was longer (5.18 days, 3.85 days (respectively) (p = 0.042). During the COVID-19 period, comparing patients with acetabulum fractures to those with pelvic ring injuries, they required more blood transfusion units, the acetabulum fractures were more time demanding with increased days of hospitalization. Additionally, patients during the COVID-19 period remained hospitalized for a shorter period of time and received lesser amount of blood transfusions with pelvic ring injuries.
Similar content being viewed by others
Introduction
Among all skeletal injuries, approximately 3% is composed of pelvic fractures. They are associated with high morbidity, mortality and healthcare cost1. Most of these injuries result from high-energy blunt trauma incidents, such as traffic accidents or falls from a height. Combined pelvic ring and acetabular fractures ranges from 5 to 16% of all pelvic and acetabular injuries with reported mortality rates of 1.5–13%2,3. However, isolated acetabular fractures tend to have a lower fatality rate, as they seldom affect the patient’s hemodynamic stability4. Higher forces may lead to the pelvic ring disruption typically observed in approximately 13–17% of all cases involving pelvic fractures and is recognized as a potentially life-threatening condition5. Among polytrauma patients, it is considered that the main factor leading to increased mortality risk is the possibility of hemorrhaging from disrupted vessels (mainly veins) due to shear forces and bony fragments6,7. The other factors causing an increase in mortality are the presence of shock or coma, and concomitant head and chest injuries8.
It is estimated that the direct and indirect median treatment cost is 29 425 Euros per patient9. Furthermore, after unstable pelvic fractures, approximately 65% of the patients restore their ability to maintain their independence in the activities of daily living10, while a total of 58% individuals can not resume their previous employment11. Therefore, the analysis of several factors associated with pelvic injuries is crucial in finding ways to reduce mortality, morbidity and improve quality of life among patients who experienced such a devastating trauma. As a logical consequence of the above, in this study, patients who suffered pelvic fractures was divided into pelvic ring injury and acetabular fracture subgroups to characterize clinical differences between them, if they exist.
At the beginning of 2020 a global pandemic of the Coronavirus, later known as Covid-19, had begun. According to World Health Organization data, almost 800 000 0000 patients suffered from this disease and over 7 000 000 related deaths has been recorded by April 202412. Those staggering numbers somehow reflect the scale of global issues that had to be challenged. Many hospitals were obliged to introduce new laws, to relocate and to deal with massive change involving staff and the access to the drugs and medical equipment. Those changes also affected trauma surgery to some extent. However, pelvic fractures during the pandemic could not be neglected by any chance due to the life threatening nature of those injuries, commonly associated with other critical injuries, such as head trauma, abdominal and thoracic hemorrhage13,14,15.
The aim of this study was to assess the impact of the COVID-19 pandemic on the epidemiology of pelvic and acetabular trauma treated operatively, specifically investigating body mass index (BMI), duration of surgery, length of hospital stay, number of blood transfusions, mechanism of injury and concomitant injuries in these patients. Secondly, to compare the epidemiologic data of the COVID period with patients treated 1 year before the outbreak of the COVID pandemic in Poland.
Materials and methods
General characteristics
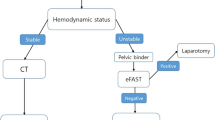
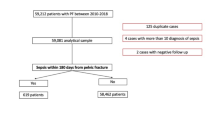
This study comprises 132 consecutive patients admitted for pelvic fracture surgery in 2019–2022, separating them into 2 groups: pre-COVID (1 year before the outbreak of pandemic— 2019) and COVID period (in Poland 2020–2022). The data was collected respectively in a single trauma center and patients were treated operatively due to acetabulum fracture or pelvic ring injury, using De Puy Synthes implants for pelvic fixation. The inclusion criteria were pelvic fractures and indications for operative treatment (Lateral Compression (LC) II and III, Anterior Posterior Compression (APC) II and III, Vertical Sheer (VS), acetabulum fractures with displacement more than 2 mm, unstable fracture pattern. The exclusion criteria were non-operative treatment for pelvic fractures, fractures requiring primary total hip arthroplasty (THA), and periprosthetic acetabular fractures. Upon admission, all patients underwent evaluation using X-ray and computed tomography (CT) scans of the pelvis.
Demographic data was collected, moreover, type of fracture according to Young-Burgess and Letournel-Judet classification system, date of injury and surgery, the surgical approach and stabilization methods, mechanism of trauma, concomitant injuries, body mass index (BMI), blood transfusions, number of days spent in the hospital, and surgery duration. Pelvic fractures were classified according to the Young-Burgess system (LC—lateral compression, APC—anterior-posterior compression, VS—vertical shear). Acetabulum fractures were classified according to the Letournel and Judet system (A + T—anterior column with posterior hemi-transverse fracture, AC—anterior column, BC—both column, PC—posterior column, PC + W—posterior column + posterior wall, PW—posterior wall, T—transverse, T + P—transverse with posterior wall fracture), while pelvic ring fractures were classified according to the Young and Burgess system (LC—lateral compression, APC—anterior-posterior compression, VS—vertical shear). Additionally, Arbeitsgemeinschaft für Osteosynthesefragen (OA) classification also categorizes acetabular fractures as follows: Type A: partial articular isolated wall or column fracture A1: posterior wall fracture with or without marginal impaction. A2: posterior column fracture possible marginal impaction. A3: anterior wall or column fracture with or without marginal impaction. type B: partial articular transverse type fracture B1: transverse fracture ± posterior wall fracture ± marginal impaction. B2: T-fracture ± posterior wall fracture ± marginal impaction. B3: posterior hemitransverse and anterior wall or column fracture. Type C: simple or multifragmentary complete articular both column fracture.
The surgical approaches used for pelvic fractures were the ilio-inguinal and Kocher-Langenbeck approaches. The ilioinguinal approach was chosen for cases involving anterior wall and anterior column fractures, both column fractures and the posterior hemi-transverse fractures. The Kocher-Langenbeck approach was preferred in the posterior wall and posterior column fractures and in most of the T-shaped transverse fractures. None of those patients had been operated on in two-stage procedure with initial external fixation.
Ethics
The study was conducted in accordance with the Declaration of Helsinki guidelines for human experiments. Prior to the study, permission for the study and approval of the experimental protocol was obtained from the Bioethics Committee of the Nicolaus Copernicus University in Torun (approval number KB 645/2022). Written informed consent was obtained from all patients or their legal guardians upon admission to the hospital to include them in scientific studies.
Statistical analysis
All group comparisons and statistical analyses were conducted by two independent investigators using Prism software (GraphPad). Relationships between the studied parameters were evaluated using the Spearman’s rank correlation coefficient. Nominal variables were characterized with number of observations and their structure. Their comparison between the two groups was run with Pearson’s chi-square test with or without Yates continuity correction, depending on expected values for adequate contingency tables.
Numerical variables were described using basic statistics i.e., mean and standard deviation in the case of normal distribution and median plus range for an abnormal distribution. Their distributions were verified with Shapiro-Wilk test. Comparisons of the variables between groups were executed with Welch t test for independent groups and Mann-Whitney U test, depending on normality of their distribution. A p-value of less than 0.05 was considered statistically significant.
Results
The analyzed group consisted totally of 91 patients after surgery, 50 acetabulum fixation and 41 pelvic ring fixations. Out of the total group, 21 were females 70 were males. There were 13 females and 37 males in the acetabulum treated subgroup and 8 females and 33 males in pelvic ring subgroup. There were no statistically significant differences in sex structure between groups (p = 0.4649).
The studied cohort had a mean body mass index (BMI) of 26.48 (SD = 4.15; range 17.85–44.87). In the acetabulum fracture subgroup, the mean BMI was 26.26 (SD = 2.77; range 20.89–31.70) and in the pelvic ring injury it was 26.74 (SD = 5.40; range 17.85–44.87), Fig. 1A., Tables 1, 2 and 3.
The mean duration of surgery was 128.5 min, (SD = 63.66), ranging from 25 to 270 min. In the acetabulum fracture subgroup, the mean duration of surgery was 151.2 min (SD = 59.3), ranging from 60 to 270 min and in the pelvic ring injury subgroup a mean value of 100.9 min, (SD = 58.16) ranging from 25 to 260 min; Fig. 1B; Tables 1, 2, 3, 4, 5, 6, 7 and 8.
The mean length of hospital stay was 4.54 days (SD = 6.09), (range 1 to 34 days). Specifically, in the acetabulum fracture subgroup it was a mean of 5.18 days (SD = 7.01), (range 2 to 34 days) and in the pelvic ring injury subgroup it was a mean of 3.76 days (SD = 4.71), (range 1–31 days); C, Tables 1, 2, 3, 4, 5, 6, 7 and 8.
The average number of blood transfusions received was 1.09 units, (SD = 1.27), with a range of 0 to 5 units. In the acetabulum fracture subgroup, mean was 1.58 units, (SD = 1.34), ranging from 0 to 5 units, and in the pelvic ring injury subgroup it was a mean of 0.51 units, (SD = 0.87), ranging from 0 to 3 units (Fig. 1D), Tables 1, 2, 3, 5 and 6.
The BMI values showed no significant differences in the acetabulum and pelvic ring injury subgroups (p = 0.9510). On the other hand, patients with acetabulum fractures demanded more blood transfusions units (p < 0.0001) comparing to pelvic ring fractures. Moreover, the acetabulum fractures were more time demanding (p < 0.0001) when compared to pelvic ring injury, as well as length of hospital stay (p = 0.042). Comparison between the mentioned details was presented in Fig. 1A–D; Tables 1, 2, 3, 5 and 6.
The mechanism of injury in the studied cohort was differentiated, but there were no statistically significant differences between the specific trauma types (p = 0.1428) (Fig. 2). Traffic accidents were the most common type of trauma, 29 patients. The pedestrian and industrial injuries were the rarest types of trauma– 4 patients in the studied cohort and 5 patients, respectively.
Additional injuries in polytrauma patients were documented in 53 patients (20 patients in acetabulum injury and 33 patients in pelvic ring injuries). Definition of polytrauma according to Veterans Affairs (VA) is: “two or more injuries to physical regions or organ systems, one of which may be life threatening, resulting in physical, cognitive, psychological, or psychosocial impairments and functional disability”16. Following that definition Fig. 2 is presented. However, there was no statistically significant difference between additional trauma types (p = 0.6281) (Fig. 3). In the pelvic ring injury subgroup, the most common concomitant injuries were: tibial fractures, lumbar spine fractures and femur fractures. Among individuals with acetabulum fractures the most prevalent associated injuries were femur and lumbar fractures (Fig. 3).
Furthermore, we compared the studied cohort of pelvic fractures treated operatively during the COVID-19 with patients treated operatively in 2019 due to pelvic fractures, 1 year before the outbreak of the pandemic. The pre-COVID group consisted of 41 patients after surgery, 17 acetabulum fixation and 24 pelvic ring fixations. Out of the total group, there were 8 females and 33 males. There were 2 females and 15 males in acetabulum treated subgroup and were 6 females and 18 males in pelvic ring subgroup. There were no statistically significant differences in sex structure between the groups (p = 0.6471) (Fig. 4).
Analyzing the pelvic ring injury, the BMI values showed no significant differences in the pre-COVID and COVID subgroups (p = 0.7384), and time of surgery (p = 0.2012). In contrast, patients treated operatively during the COVID period had significantly shorter stay in the hospital (p < 0.0001) and less units of blood transfusions (p = 0.0401). Comparison between the mentioned details was presented in Fig. 4.
(A) Comparison of BMI in pelvic ring injury subgroups before and during COVID. (B) Comparison of operative time in pelvic ring injury subgroups before and during COVID. (C) Comparison of days spent in hospital in pelvic ring injury subgroups before and during COVID. (D) Comparison of blood transfusion units in pelvic ring injury subgroups before and during COVID years. Hosp.- hospital. Trans.- transfusion.
When compared acetabulum fractures, the BMI values showed no significant differences in the pre-COVID and COVID subgroups (p = 0.7185), time of surgery (p = 0.6347), length of the hospital stay (p = 0.4488) and blood transfusion units (p = 0.8152). Comparison between mentioned details was presented in Fig. 5.
(A) Comparison of BMI in acetabulum injury subgroups before COVID. (B) Comparison of operative time in acetabulum injury subgroups before COVID. (C) Comparison of days spent in hospital in acetabulum injury subgroups before COVID. (D) Comparison of blood transfusion units in acetabulum injury subgroups before COVID.
Discussion
The findings of this study indicate that patients who suffered from acetabular fractures required a notably greater number of blood units transferred and the duration of surgery was longer compared to pelvic ring injuries subgroup. Both results were statistically significant (p = 0.0002 and p < 0.0001 respectively). Furthermore, in the acetabular fracture group the most concomitant injuries were femur fracture, pneumothorax, skull fracture, while in the pelvic ring ijuries subgroup were pneumothorax, lumbar spine fracture, femur fracture but they did not reach statistical significance (p = 0.3417).
In regard to the COVID-19 pandemic’s impact on the gathered data, we found that patients during pandemic had statistically significantly shorter duration of hospital stay and lesser amount of blood units transferred comparing to the non- pandemic group, 4.5 days vs. 6.9 days (Fig. 4C) and 1.2 units vs. 1.4 units (Fig. 4D), respectively.
Gender
This study presented that 70% of patients who experienced pelvic ring injury were male and 30% were female, while 78% of individuals who suffered from acetabular fracture were male and 22% female. There was not significant difference in sex structure between subgroups. The findings about acetabular fracture were consistent with result of investigation of Melhem et al. who studied data of 32 614 patients in France. They presented that there was male predominance in acetabular fractures (61% males, 39% females). Likewise, Boudissa et al.17 and Maia et al.18 provided male sample dominance in acetabular fractures. Males accounted for 74% and 85.5% of the studied population, respectively. However, the literature shows contradictory data on the sex structure and pelvic ring injuries. For instance, among 164 694 patients who suffered from pelvic ring injury, 72% were female19. Similar results were presented by Buller et al. who investigated 1 464 458 subjects, and 69.7% of them were female20. Balogh et al. showed two distinct demographic groups with pelvic ring injuries what may explain discrepancy between studies. They distinguished high-energy pelvic ring injuries represented mainly by young men (64% male; mean age 41) and low-energy osteoporotic pelvic ring injuries that affects old women (61% female; mean age 83)21. However, this study did not investigate the age of the patients, but the main cause of the injuries was traffic accident that belongs to high-energy mechanisms what may potentially explain the male predominance. The pandemic had no impact on the male/ female ratio in the studied population. Mohan et al. and Usman et al. presented similar results in male/ female ratio, where males accounted for 68% of all pelvic fractures during the COVID-19 Pandemic22,23.
BMI
The studied cohort had a mean BMI of 26.34 (ranging from 17.8 to 44.8) and no statistically important differences was found in COVID and pre- COVID patients in regards to BMI (Fig. 4A). In the acetabulum fracture subgroup, the mean BMI was 26.31 (ranging from 18.1 to 39.1), while in the pelvic ring injury it was 26.37 (ranging from 17.8 to 44.8). A similar result to the current study was obtained by Henstenburg et al. who presented that average BMI of 131 patients was 28.7 ± 6.8724. In another publication, which included 39 individuals who suffered from acetabulum fracture, the authors provided the mean BMI of 23.025. However, none of the mentioned investigations compared BMI between acetabulum fracture and pelvic ring injury groups. Furthermore, in the available literature, information on BMI among subjects with pelvic fracture is limited.
Duration of surgery
Regarding the operative time, acetabulum fractures required more time spent in the operation theater. Thus, it may be assumed that these injuries were more challenging compared to pelvic ring injuey. There have been no statistically important differences found in the covid and pre- covid duration of pelvic surgeries (Fig. 4B). It may be explained with no reasonable causes that could affect the procedure itself, since all the procedures had been performed in the same manner, with the same tools and equipment explained in “materials and methods” section. Furthermore, there has been no literature concerning the impact of the covid pandemic on the duration of pelvic fixation surgeries. Nonetheless, several publications have been presented within last year concerning the impact of COVID-19 Pandemic on proximal femoral fractures. For instance, Anusitviwat et al. did not found any significant differences in duration of proximal femoral fixation surgeries between pandemic and non-pandemic group26. In the acetabulum fracture the mean time of surgery was 153 min (ranging from 60 to 270 min), while in the pelvic ring injury it was 102 min (ranging from 25 to 260 min). To our knowledge, there are only 2 investigations describing the time of surgery in acetabulum fractures and there is a lack of any studies on pelvic ring injury. Application of Kocher-Langenbeck approach in posterior wall fractures was examined by Dailey et al. who noticed similar result to our mean operative time of 153.5 min. They also presented that using anterior intrapelvic approach in both column fractures or anterior column posterior hemi-transverse fractures, time required was 270 min27.
Length of hospital stay
The results of days spent in hospital among patients with acetabulum and pelvic ring injuries were proven to be statistically insignificant (5.1 and 4.9 days respectively). The mean length of hospital stay was 5.1 days. Similar result was obtained by Malik et al. who found that 79.2% of patients with acetabulum or pelvic fracture spent in the hospital from 0 to 9 days28. What is more, we found that patients who were operated on during pandemic experienced a statistically significant shorter duration of hospital stay comparing to the non-pandemic group (4.5 days vs. 6.9 days; Fig. 4C). Likewise, Anusitviwat et al. and Amzallag et al. found that patients admitted for proximal femoral fixation during Pandemic had shorter length of hospital stay 11.1 ± 5.6 and 9.6 ± 4.1 days and 10.0 vs. 12.0 days, respectively26,29. Both results were proven to be statistically significant26,29. It can be explained mainly due to the shorter period of postoperative rehabilitation within the clinic due to the epidemiologic restrictions and also by the reduction of workload due to the cancellation of elective surgeries29.
However, most studies indicate longer period spent in the hospital. For instance, Prieto-Alhambra et al. presented that the mean length of stay was 9 days30. Other researchers reported longer hospital stay that was 15 days31,32. Interestingly, Marrinan et al. found association between age and length of hospital among patients who suffered from osteoporotic pelvic fracture. They showed that the median length of hospital stay was 30 days for females (averagely 85 years) and 39 days for males (averagely 79 years)33. The current study presented relatively short time spent in hospital. The discrepancy may be because patients with acetabulum or pelvic ring injuries are operatively managed only in our trauma center in the region. Therefore, some individuals were transported to our hospital after prior stabilization of their general condition in another medical center and did not require additional procedures before surgery. The number of days spent in other hospitals was not counted.
Blood transfusion units
Patients with acetabulum fractures demanded more blood transfusion units comparing to pelvic ring injuries (averagely 1.5 unit vs. 0.8 units respectively; p = 0.0002). Interestingly, we also found a statistically significant difference in reduction of blood transfusion in patients hospitalized during pandemic (1.2 vs. 1.4 mean blood units; Fig. 4D). We suspect that this reduction could be explained by more restrictive regulations concerning qualification for blood transfusion due to the massive growth of blood transfusion in severely ill covid patients34.
However, our findings do not align with the outcomes of other investigations and results differ between trauma centers. For instance, Magnussen et al. found that patient with isolated acetabular fractures required the same number of blood units as those with isolated pelvic ring injuries. Furthermore, they statistically proved, that mean blood transfusion unit was 4.8135. Likewise, Abdelrahman et al. analyzed 1814 patients who suffered pelvic fractured and noticed higher demand for blood transfusion. In their study, mean number of transferred blood units was 631. Furthermore, in the study of Palmcrantz et al., they noted that average value of blood units transferred was 2.336. It is suspected that the difference between our facility and mentioned studies may result from the percentage of hemodynamically unstable patients. For example, 44% of patients included in Abdelrahman et al. investigations, were hemodynamically instable during admission31. Hence, we suspect that due to small sample size in our study, the percentage of hemodynamically instable patients may have been lower, resulting in a decreased demand for blood transfusion.
Mechanism of injury
In the current study, the main cause of pelvic injury was traffic accidents, and this agrees with many studies. For instance, road traffic crashes in the United Kingdom accounted for 62.9% of all accidents32. Likewise, in the Netherlands it was 64.9%5 and in Turkey 66.8%37. In India, the percentage of traffic accidents in pelvic injuries was higher and reached 77.3%38, while in Bangladesh it was 48%39. However, some research indicate that in the near future pelvic ring injuries may be more frequently linked to falls rather than vehicle accidents due to subsequent advancements in vehicle (i.e. speed limiters) and road safety40. Mohan et al. presented that fall from height was the main cause of pelvic fractures during COVID pandemic, however, they also did not observe any significant differences in patterns of injury due to the pandemic22. Similarly, we did not find any statistically significant changes of the main causes of pelvic trauma due to the pandemic (Fig. 2).
Associated injuries
Within the group of patients with pelvic ring injuires group the most common associated injuries were pneumothorax, lumbar spine fractures and femur fractures, while in acetabulum fracture group femur fractures, pneumothorax and skull fractures. The results of current study seem to be coherent to Lunsjo et al.’s investigation. They did not distinguished pelvic ring and acetabulum fracture group, but provided that chest injuries (pneumothorax, hemothorax, rib fractures), skull fractures and spine fractures were the most often additional damages41. Although the main cause of pelvic injury is traffic accident, the most common associated injuries between studies vary. For instance, Ferede et al. presented that lower extremity (35.9%), abdominal (25%) and chest (17.2%) were the most affected areas of the body in pelvic injuries42. An investigation by Ghosh et al. showed that the most common additional injuries were lower extremity injury (mainly femur fracture), blunt abdominal trauma, urogenital injury and head injury38. Additionally, a study by Schmal et al. found that most frequent associated injuries were bladder and urethra laceration (29%), retroperitoneal hematoma (27%) and the lumbosacral plexus lesion (27%)43. The discrepancies in the presented studies may result from a few reasons. Firstly, small or moderate sample size and number of investigations seem to be limiting. Secondly, the broad definition of a traffic accident that can involve pedestrians and users of cars, motorcycles, bicycles and other vehicles. What is more, other factors like speed during the crash, vehicle safety systems, the direction of the applied force to mention a few, may lead to a wide spectrum of concomitant injuries in pelvic fractures.
Limitations
It is crucial to point out some limitations to this study. Firstly, the sample size was moderate and consisted of a local population admitted to a single trauma center. Secondly, this was a retrospective study, so some biases could appear and influence the results. Thirdly, all patients were operated by the same operative team what could impact investigated factors, especially duration of surgery, number of blood units transfused, and length of hospital stay. In addition, only a few papers available so far as compared the concerning epidemiology of pelvic and proximal humerus fractures before and post the COVID pandemic22,23,26,29,44,45. In our study we did not assess the patients with Injury Severity Score (ISS) nor New Injury Severity Score (NISS). Especially NISS has been proven to facilitate good assessment of the injuries in order to provide accurate treatment46,47. Lack of trauma severity scoring may have an impact on obtained results.
Conclusions
During the COVID-19 period patients with acetabulum fractures required more blood transfusion units, comparing to pelvic ring injury and moreover, the acetabulum fractures were more time demanding with increased days of hospitalization. Comparing the COVID-19 period with 1 year before the pandemic outbreak, patients during the COVID-19 period remained hospitalized for a shorter period and received lesser amount of blood transfusions with pelvic ring injuries.
Data availability
Data is provided within the manuscript file or its supplementary file.
References
Halawi, M. J. Pelvic ring injuries: surgical management and long-term outcomes. J. Clin. Orthop. Trauma. 7, 1–6 (2016).
Veerappa, L. A., Tippannavar, A., Goyal, T. & Purudappa, P. P. A systematic review of combined pelvic and acetabular injuries. J. Clin. Orthop. Trauma. 11, 983–988 (2020).
Halvorson, J. J. et al. Combined acetabulum and pelvic ring injuries. JAAOS - J. Am. Acad. Orthop. Surg. 22, 304 (2014).
Basile, G. et al. Pelvic ring and acetabular fracture: concepts of traumatological forensic interest. Injury 53, 475–480 (2022).
Hermans, E., Biert, J. & Edwards, M. J. R. Epidemiology of pelvic ring fractures in a level 1 trauma center in the Netherlands. Hip Pelvis. 29, 253–261 (2017).
Gabbe, B. J. et al. Predictors of mortality following severe pelvic ring fracture: results of a population-based study. Injury 42, 985–991 (2011).
Rommens, P. M. & Hessmann, M. H. Staged reconstruction of pelvic ring disruption: differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-Type lesions. J. Orthop. Trauma. 16, 92 (2002).
Ooi, C. K., Goh, H. K., Tay, S. Y. & Phua, D. H. Patients with pelvic fracture: what factors are associated with mortality? Int. J. Emerg. Med. 3, 299–304 (2010).
Aprato, A. et al. Direct and indirect costs of surgically treated pelvic fractures. Arch. Orthop. Trauma. Surg. 136, 325–330 (2016).
Tötterman, A., Glott, T., Søberg, H. L. & Madsen, J. E. Røise, O. Pelvic trauma with displaced sacral fractures: functional outcome at one year. Spine 32, 1437 (2007).
Aprato, A. et al. Are work return and leaves of absence predictable after an unstable pelvic ring injury? J. Orthopaed Traumatol. 17, 169–173 (2016).
COVID-19 deaths | WHO COVID-19 dashboard. datadot https://data.who.int/dashboards/covid19/cases
Benders, K. E. M. & Leenen, L. P. H. Management of hemodynamically unstable pelvic ring fractures. Front. Surg. 7, 601321 (2020).
Walters, S. et al. Causes and associations with mortality in patients with pelvic ring injuries with haemorrhagic shock. Eur. J. Orthop. Surg. Traumatol. https://doi.org/10.1007/s00590-023-03516-y (2023).
Suzuki, T. et al. Combined injuries of the pelvis and acetabulum: nature of a devastating dyad. J. Orthop. Trauma. 24, 303–308 (2010).
VA.gov | Veterans Affairs. https://www.polytrauma.va.gov/news-and-resources/terminology-and-definitions.asp
Boudissa, M. et al. Epidemiology and treatment of acetabular fractures in a level-1 trauma centre: retrospective study of 414 patients over 10 years. Orthop. Traumatology: Surg. Res. 103, 335–339 (2017).
Maia, M. S. et al. Epidemiological analysis on acetabular fractures. Rev. Bras. Ortop. 46, 23–26 (2011).
Melhem, E., Riouallon, G., Habboubi, K., Gabbas, M. & Jouffroy, P. Epidemiology of pelvic and acetabular fractures in France. Orthop. Traumatology: Surg. Res. 106, 831–839 (2020).
Buller, L. T., Best, M. J. & Quinnan, S. M. A nationwide analysis of pelvic ring fractures: incidence and trends in treatment, length of stay, and mortality. Geriatr. Orthop. Surg. Rehabil. 7, 9–17 (2016).
Balogh, Z. et al. The epidemiology of pelvic ring fractures: A Population-Based study. J. Trauma. Acute Care Surg. 63, 1066 (2007).
Mohan, K. et al. Impact of the COVID-19 pandemic on pelvic and acetabular trauma: experiences from a National tertiary referral centre. Cureus 13, e15833.
Usman, M. et al. Evolving practice in management of Pelvic-Acetabular trauma: COVID-19 experience from a tertiary referral centre in the UK. Cureus 13, e18778 (2021).
Henstenburg, J. M., Larwa, J. A., Williams, C. S., Shah, M. P. & Harding, S. P. Risk factors for complications following pelvic ring and acetabular fractures: A retrospective analysis at an urban level 1 trauma center. J. Orthop. Trauma. Rehabilitation. 28, 22104917211006890 (2021).
Jang, J. H., Moon, N. H., Rhee, S. J., Jung, S. J. & Ahn, T. Y. Surgical outcomes of transverse acetabular fractures and risk factors for poor outcomes. BMC Musculoskelet. Disord. 22, 222 (2021).
Anusitviwat, C., Vanitcharoenkul, E., Chotiyarnwong, P. & Unnanuntana, A. Surgical treatment for fragility hip fractures during the COVID-19 pandemic resulted in lower short-term postoperative functional outcome and a higher complication rate compared to the pre-pandemic period. Osteoporos. Int. 33, 2217–2226 (2022).
Dailey, S. K. & Archdeacon, M. T. Open reduction and internal fixation of acetabulum fractures: does timing of surgery affect blood loss and OR time?? J. Orthop. Trauma. 28, 497 (2014).
Malik, A. T. et al. 30-day adverse events, length of stay and re-admissions following surgical management of pelvic/acetabular fractures. J. Clin. Orthop. Trauma. 10, 890–895 (2019).
Amzallag, N., Factor, S., Shichman, I., Ben-Tov, T. & Khoury, A. Hip fractures during the COVID-19 pandemic: demographics, treatment pathway, and outcomes. Isr. Med. Assoc. J. 23, 484–489 (2021).
Prieto-Alhambra, D. et al. Burden of pelvis fracture: a population-based study of incidence, hospitalisation and mortality. Osteoporos. Int. 23, 2797–2803 (2012).
Abdelrahman, H. et al. Patterns, management, and outcomes of traumatic pelvic fracture: insights from a multicenter study. J. Orthop. Surg, Res. 15, 249 (2020).
Giannoudis, P. V. et al. Prevalence of pelvic fractures, associated injuries, and mortality: the united Kingdom perspective. J. Trauma. Acute Care Surg. 63, 875 (2007).
Marrinan, S., Pearce, M. S., Jiang, X. Y., Waters, S. & Shanshal, Y. Admission for osteoporotic pelvic fractures and predictors of length of hospital stay, mortality and loss of independence. Age Ageing. 44, 258–261 (2015).
Fernando, M. C., Hayes, T., Besser, M. & Falter, F. Comparison of blood and blood product transfusion in COVID-19 and Non-COVID-19 patients requiring extracorporeal membrane oxygenation for severe respiratory failure. J. Clin. Med. 12, 4667 (2023).
Magnussen, R. A., Tressler, M. A., Obremskey, W. T. & Kregor, P. J. Predicting blood loss in isolated pelvic and acetabular High-Energy trauma. J. Orthop. Trauma. 21, 603 (2007).
Palmcrantz, J. et al. Pelvic fractures at a new level 1 trauma centre: who dies from pelvic trauma? The Inkosi Albert luthuli central hospital experience. Orthop. Surg. 4, 216–221 (2012).
Saydam, M. et al. Correlation of pelvic fractures and associated injuries: an analysis of 471 pelvic trauma patients. Ulus Travma Acil Cerrahi Derg. 25, 489–496 (2019).
Ghosh, S., Aggarwal, S., Kumar, V., Patel, S. & Kumar, P. Epidemiology of pelvic fractures in adults: our experience at a tertiary hospital. Chin. J. Traumatol. 22, 138–141 (2019).
Hossain, A. et al. Epidemiology of pelvic fractures in adult: our experience at two tertiary care hospital in Dhaka, Bangladesh. J. Clin. Orthop. Trauma. 11, 1162–1167 (2020).
Leach, S. E. T., Skiadas, V., Lord, C. E. & Purohit, N. Pelvic fractures: experience of pelvic ring fractures at a major trauma centre. Clin. Radiol. 74, 649e19–649e26 (2019).
Lunsjo, K. et al. Associated injuries and not fracture instability predict mortality in pelvic fractures: A prospective study of 100 patients. J. Trauma. Acute Care Surg. 62, 687 (2007).
Ferede, B., Ayenew, A. & Belay, W. Pelvic fractures and associated injuries in patients admitted to and treated at emergency department of Tibebe ghion specialized hospital, Bahir Dar university, Ethiopia. Orthop. Res. Reviews. 13, 73–80 (2021).
Schmal, H., Markmiller, M., Mehlhorn, A. T. & Sudkamp, N. P. Epidemiology and outcome of complex pelvic injury. Acta Orthop. Belg. 71, 41–47 (2005).
Mackay, N. D., Wilding, C. P., Langley, C. R. & Young, J. The impact of COVID-19 on trauma and orthopaedic patients requiring surgery during the peak of the pandemic. Bone Jt. Open. 1, 520–529 (2020).
Ormeño, J. C., Martínez, R., Frías, C., Von Plessing, C. & Quevedo, I. Impact of the COVID-19 pandemic on osteoporotic hip fractures in Chile. Arch. Osteoporos. 17, 130 (2022).
Li, H. & Ma, Y. F. New injury severity score (NISS) outperforms injury severity score (ISS) in the evaluation of severe blunt trauma patients. Chin. J. Traumatol. 24, 261–265 (2021).
Chun, M. et al. New injury severity score and trauma injury severity score are superior in predicting trauma mortality. J. Trauma. Acute Care Surg. 92, 528–534 (2022).
Author information
Authors and Affiliations
Contributions
R.W., T.P. and P.W. formal analysis, resources, manuscript writing and editing; J.Z. M.Z. and M.W. supervision, funding acquisition, critical revision of the article, and final approval; J.E., M.D. and J.O. manuscript writing and editing; B.M. and A.J. critical revision of the article and final approval. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pielak, T., Zabrzyńska, M., Wójcicki, R. et al. Impact of COVID-19 pandemic outbreak on pelvic trauma surgical management. Sci Rep 15, 6323 (2025). https://doi.org/10.1038/s41598-025-90895-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90895-3