Abstract
Background
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is associated with long-term disability and poor quality of life (QoL). Cardinal ME/CFS symptoms (including post-exertional malaise, cognitive dysfunction and sleep disturbances) have been observed in Post COVID-19 Condition (PCC). To gain further insight into the potential role of ME/CFS as a post-COVID-19 sequela, this study investigates associations between symptoms and patient-reported outcomes, as well as symptom clusters.
Methods
Participants included Australian residents aged between 18 and 65 years formally diagnosed with ME/CFS fulfilling the Canadian or International Consensus Criteria or PCC meeting the World Health Organization case definition. Validated, self-administered questionnaires collected participants’ sociodemographic and illness characteristics, symptoms, QoL and functional capacity. Associations between symptoms and patient-reported outcomes were investigated with multivariate linear regression models. Hierarchical cluster analysis was performed to identify symptom clusters.
Results
Most people with ME/CFS (pwME/CFS) and people with PCC (pwPCC) were female (n = 48/60, 80.0% and n = 19/30, 63.3%, respectively; p = 0.12). PwME/CFS were significantly younger (x̄=41.75, s = 12.91 years) than pwPCC (x̄=48.13, s =10.05 years; p =0.017). Autonomic symptoms (notably dyspnoea) were associated with poorer scores in most patient-reported outcome domains for both cohorts. None of the four symptom clusters identified were unique to ME/CFS or PCC. Clusters were largely delineated by the presence of gastrointestinal and neurosensory symptoms, illness duration, ME/CFS criteria met and total symptoms.
Conclusions
Illness duration may explain differences in symptom burden between pwME/CFS and pwPCC. PCC diagnostic criteria must be refined to distinguish pwPCC at risk of long-term ME/CFS-like illness and subsequently deliver necessary care and support.
Plain English summary
Post COVID-19 Condition (PCC), or Long COVID, refers to the ongoing symptoms experienced after acute COVID-19 illness. The symptoms reported by people with PCC (pwPCC) resemble Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). However, existing diagnostic criteria for PCC are broad and cannot discern PCC subtypes (such as pwPCC experiencing ME/CFS-like illness), which may require different approaches to care. This study contributes to improving PCC case criteria and approaches to care for both ME/CFS and PCC by investigating the relationships between symptoms and patient-reported outcomes among pwPCC and people with ME/CFS (pwME/CFS).
For both cohorts, symptoms had a negative relationship with all aspects of health. Autonomic symptoms, notably breathing issues, returned the most negative associations. Pain, flu-like symptoms and lack of temperature control appeared more burdensome among pwPCC. These symptoms may signify the early stages of ME/CFS. Symptom clusters were also identified for the first time among a combined cohort of pwME/CFS and pwPCC in this study. Importantly, none of the symptom clusters were specific to ME/CFS or PCC. Instead, symptom clusters were defined by the prevalence of gastrointestinal and neurosensory symptoms, illness duration, ME/CFS criteria met and the total number of symptoms.
This study suggests that the few differences between ME/CFS and PCC may be explained by illness duration. These findings further implicate ME/CFS as a potential post-COVID-19 outcome. As ME/CFS is associated with profound reductions in quality of life and functioning, identifying pwPCC experiencing ME/CFS-like illness through refined diagnostic criteria must be prioritised to ensure the delivery of necessary care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a chronic multi-systemic illness associated with substantial reductions in quality of life (QoL) and profound functional impairments [1,2,3,4,5,6]. People with ME/CFS (pwME/CFS) experience poorer mental and emotional wellbeing, as well as a profound burden on physical health when compared with healthy people and the general population [2, 3, 7, 8]. The symptoms of ME/CFS are debilitating and impose considerable restrictions on one’s ability to participate in the activities of typical daily life [1, 4, 5, 9]. Post-exertional malaise – the worsening of symptoms following physical, mental or emotional exertion – is the cardinal symptom of ME/CFS [4,5,6, 9]. Other key symptoms include cognitive dysfunction, unrefreshed sleep, bodily pain and autonomic disturbances, such as thermostatic dysregulation, gastrointestinal upset and cardiorespiratory symptoms [4,5,6, 9].
The global prevalence of ME/CFS is approximately 1% [4,5,6, 10]. As investigations into an illness-specific biomarker for ME/CFS remain ongoing, diagnosis continues to rely on the fulfillment of case definitions [4, 9]. Currently, the preferred case definitions for diagnosing ME/CFS include the Canadian Consensus Criteria (CCC) [6] and International Consensus Criteria (ICC) [5]. There is no curative therapy for ME/CFS and recovery is reported in fewer than 10% of cases [4, 9, 11, 12]. The aetiopathogenesis of ME/CFS also remains elusive [4,5,6, 9]. Many environmental stressors, such as exposure to chemicals, trauma, stress and injury, have been identified as risk factors [11,12,13]. However, between 60% and 80% of pwME/CFS report a post-infectious illness onset [4, 14, 15].
Chronic multi-systemic illness reminiscent of ME/CFS has been observed among people with a history of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection [16,17,18]. Termed “Post COVID-19 Condition (PCC)”, this post-infectious sequela of acute COVID-19 illness consists of persistent symptoms for a minimum of 12 weeks according to the World Health Organization (WHO) case definition [19]. Between 40% and 60% of people with PCC (pwPCC) fulfil ME/CFS case criteria [20,21,22]. Additionally, the reported prevalence of post-exertional malaise among pwPCC ranges from 50% to 100% [20, 22,23,24,25,26].
Like ME/CFS, PCC is associated with poorer self-perceptions of overall health status and impairments in physical, mental and emotional wellbeing [22, 27, 28]. Whilst shared impairments in cell function have been identified among pwME/CFS and pwPCC [29], incomplete understanding of ME/CFS and PCC pathophysiology impedes definitive conclusions regarding the relationship of these two illnesses as the same or related, yet different, entities [16, 17, 30]. Additionally, PCC case definitions are broad and are unable to differentiate between illness subtypes [30,31,32]. Identifying COVID-19 survivors at risk of long-term illness reminiscent of ME/CFS is integral to guide the appropriate provision of care services and ensure a personalised approach to illness management [31,32,33].
The present study therefore serves to inform developments in PCC case definitions by comparing the illness burdens experienced by pwME/CFS and pwPCC in detail. Regression and cluster analyses were pursued to determine whether PCC exhibits distinct illness characteristics when compared with ME/CFS that may aid in differentiating subtypes of post-COVID-19 sequelae. Hence, this research may provide further insight into the role of ME/CFS in the illness trajectory of PCC.
This study also contributes to informing care pathways for ME/CFS and PCC by identifying associations between specific symptoms with QoL and functional capacity domains. Consequently, this research may highlight priority areas to be considered in the clinical management of ME/CFS and PCC to mitigate further QoL reductions and functional impairments. Finally, this study is the first to document symptom clusters and associations with patient-reported outcomes among an Australian cohort of pwME/CFS and pwPCC. By exemplifying the burden of ME/CFS and PCC on consumers in the Australian context, this research serves to guide national healthcare policy reforms and necessitate improved access to multidisciplinary care and support services for Australians who live with these conditions.
Methods
Study setting and participants
Data was collected for this cross-sectional study between March 2021 and August 2022 from a cohort of pwME/CFS and pwPCC who participated in a previous research project at the National Centre for Neuroimmunology and Emerging Diseases (NCNED), Griffith University, Gold Coast, Queensland, Australia [22]. This dataset [22] was ascertained by screening the NCNED’s participant database, which comprised approximately 1,200 participants. Of the database participants, 250 were eligible and recruited. Among these participants, n = 61 pwME/CFS and n = 31 pwPCC participated in the research [22]. These participants were subsequently evaluated to determine their eligibility for further analysis in the present study (Fig. 1).
Participant recruitment and screening for eligibility. Figure generated with Microsoft Word. Abbreviations NCNED National Centre for Neuroimmunology and Emerging Diseases; PwME/CFS People/person with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome; PwPCC People/person with Post COVID-19 Condition
To be considered eligible, participants were required to be: (1) aged between 18 and 65 years; (2) a current Australian resident; and (3) formally diagnosed with ME/CFS or PCC by a physician. Additional eligibility criteria for pwME/CFS included: (a) a history of fulfilling at least one of the CCC [6] or ICC [5] within the last two years and (b) no history of acute COVID-19 illness prior to ME/CFS onset. Fulfilling the WHO case definition [19] was mandatory for pwPCC.
Participants who were currently smoking or pregnant were deemed ineligible. Additionally, participants were excluded if they reported a history of health concerns that may confound or explain their symptoms, QoL or functional capacity. Such exclusionary health concerns have been previously described [22] and include any formally diagnosed: (1) genetic, metabolic, immunological, neurological, cardiovascular or respiratory disease; (2) malignancy within the last five years; and (3) mental illness or other chronic multi-systemic or post-viral illness.
Comorbid dysautonomia or chronic pain conditions (such as Irritable Bowel Syndrome (IBS), Postural Orthostatic Tachycardia Syndrome and Fibromyalgia) were not considered exclusionary in the present study due to the notable overlap of the symptoms of these conditions with ME/CFS and post-viral illness [5, 6, 15, 34, 35]. Similarly, a concurrent or subsequent diagnosis of anxiety or depression was not considered exclusionary due to the frequent co-occurrence of secondary anxiety and depression with ME/CFS and PCC [5, 6, 19, 34, 36].
This study received ethical approval from the Griffith University Human Research Ethics Committee (HREC) (Reference Number: 2019/1005) and the Gold Coast University Hospital HREC (Reference Number: HREC/2019/QGC/56469). Informed consent was obtained from all study participants prior to participation. The research design, collection of data and reporting of results have been informed by and adhere to the Australian Government National Health and Medical Research Council National Statement on Ethical Conduct in Human Research 2023 [37], the World Medical Association Declaration of Helsinki [38] and the Strengthening the Reporting of Observational Studies in Epidemiology Statement guidelines [39] (Table S1, Online Resource 1).
Data collection
The NCNED’s Research Registry Questionnaire was used to collect participants’ sociodemographic characteristics and illness presentation (including symptom presence, severity and frequency) as previously described [22]. This questionnaire also consisted of validated patient-reported outcome measures (PROMs) to quantify participants’ QoL and functional capacity. In the context of the present study, QoL is defined as one’s perceptions of their health, including their physical, mental, emotional and social wellbeing [40, 41]. Functional capacity refers to one’s ability to complete activities relating to daily living and participation in one’s community [42]. QoL and functional capacity were captured in this study via the 36-Item Short-Form Health Survey version 2 (SF-36v2) [41] and the World Health Organization Disability Assessment Schedule version 2.0 (WHODAS 2.0) [42], respectively.
The SF-36v2 [41] consists of eight domains: Physical Functioning, Role Limitations due to Physical Health Problems (Role Physical), Bodily Pain, General Health Perceptions, Vitality, Social Functioning, Role Limitations due to Personal or Emotional Problems (or Role Emotional) and General Mental Health [41]. SF-36v2 [41] domain scores reflect the percentage of QoL, with minimum and maximum scores of 0 and 100, respectively [41].
Seven domains comprise the WHODAS 2.0 [42], including: Cognition, Mobility, Self-Care, Getting Along, Life Activities 1, Life Activities 2 and Participation [42]. The Life Activities 2 domain measures one’s ability to perform work or school activities [42]. Consequently, this domain has been omitted from the present study, as many pwME/CFS and pwPCC experience a reduced capacity to work [9, 16, 34, 43]. WHODAS 2.0 domain scores range from 0 to 100 and correspond to the percentage of disability or difficulty in functioning [42].
Statistical analyses
Data was analysed using Statistical Package for the Social Sciences (SPSS) version 29 (IBM Corp, Armonk, New York [44]). The statistical methods chosen and the reporting of results have been informed by the Statistical Analyses and Methods in the Published Literature guidelines [45]. For all statistical tests (including post-hoc analyses), α = 0.05 and p-values are accurate to two significant figures except where p < 0.001. For all continuous variables, normality and homogeneity of variances were investigated to determine the appropriate parametric or non-parametric test. Normality was confirmed with the Kolmogorov-Smirnov and Shapiro-Wilk tests among pwME/CFS (n ≥ 50) and pwPCC (n < 50), respectively. Normally distributed variables were assessed for homogeneity of variances using Levene’s test. The number and percentage of participants with missing data are reported for all relevant variables.
Sociodemographic and illness characteristics
Mann-Whitney U tests were used for non-parametric variables and two-tailed independent samples t-tests for parametric variables to compare the sociodemographic and illness characteristics of the two study cohorts. Categorical variables were analysed with Chi-square, Fisher’s exact and Fisher-Freeman-Halton tests depending on the distribution and number of outcomes in the dependent variable. Post-hoc pairwise comparisons (either a Chi-square or Fisher’s exact test, depending on the distribution of outcomes) were performed for categorical variables when more than two outcomes returned significance. The p-values resulting from these post-hoc analyses were subsequently adjusted for multiple comparisons using the Benjamini-Hochberg correction [46].
Multivariate linear regression
For each PROM domain, multivariate linear regression models of symptom presence were generated while controlling for age, sex, body mass index (BMI) and illness duration. Separate regression models were created for the two participant cohorts. The sociodemographic covariates were added into each model using the ‘Enter’ method with entry = 0.05 and removal = 0.10. Using the same entry and removal thresholds, symptoms were subsequently entered into the regression models using the ‘Stepwise’ method. For each PROM domain, the lowest Akaike Information Criterion (AIC) value identified the final model. All independent variables were assessed for multicollinearity and the residuals were examined for outliers and normality, as well as linearity and homoscedasticity with the predictive values. Partial rank correlations of the PROM domains with symptom presence while controlling for age, sex, BMI and illness duration were also performed to determine the robustness of the multivariate linear regression models. The final partial rank correlation models were generated by including the sociodemographic covariates and all symptoms returning significance.
McDonald’s ω internal consistency values were generated for all PROM domains to determine their reliability among the entire study cohort. The threshold for sufficient reliability was ω ≥ 0.7 [47].
Cluster analysis
An exploratory, agglomerative approach using unsupervised hierarchical cluster analysis was employed to identify clusters among the pwME/CFS and pwPCC collectively based on symptom presence. The hierarchical cluster analysis was performed using Ward’s method and a squared Euclidean distance threshold of 10. Sociodemographic data, illness characteristics and patient-reported outcomes were subsequently compared among the resulting clusters. Categorical variables were analysed using the same methods outlined in the analysis of the sociodemographic and illness characteristics. Non-parametric variables were compared between the clusters with Kruskal-Wallis H tests and parametric variables with one-way Analysis of Variance tests. One-way Analysis of Covariance (ANCOVA) tests were employed to compare the parametric PROM domains between the clusters while controlling for age, sex, BMI and illness duration. Partial rank correlations controlling for the sociodemographic covariates were performed for the non-parametric PROM domains and as robustness checks of the parametric domains. The p-values arising from the partial rank correlations were adjusted for multiple comparisons with the Benjamini-Hochberg correction [46].
Internal consistency of the PROM domains was also investigated among each of the clusters using McDonald’s ω and the ω ≥ 0.7 threshold for sufficient reliability [47].
Results
The present study captured n = 60 pwME/CFS and n = 30 pwPCC. Two participants included in the previous study [22] – n = 1 pwME/CFS and n = 1 pwPCC – did not provide complete symptom data and, consequently, could not be included in the cluster or regression analyses of the present study (Fig. 1). The cohort sizes for the regression analyses were n = 60 pwME/CFS and n = 29 pwPCC, as illness duration data was missing for n = 1 pwPCC. Complete symptom data was otherwise available for this participant and included in the cluster analyses.
Sociodemographic and illness characteristics
Participants’ sociodemographic and illness characteristics are summarised in Table 1. PwME/CFS were significantly younger and had a significantly longer illness duration than pwPCC (p = 0.017 and p < 0.001, respectively). Most pwME/CFS and pwPCC were female, living in Queensland and had completed tertiary education. ME/CFS case criteria were met by 60.0% (n = 18/30) of pwPCC. There was no difference in the distribution of the most stringent ME/CFS criteria met after post-hoc analyses (p > 0.05, corrected). PwME/CFS experienced significantly more symptoms compared with pwPCC (p < 0.001). Similar results were returned when comparing the total number of symptoms experienced among only the participants fulfilling ME/CFS criteria (p = 0.0022).
Symptoms and patient-reported outcomes
The results of all regression models generated, including the unstandardised B coefficients of the included variables and adjusted R2 goodness-of-fit values, for the SF-36v2 [41] and WHODAS 2.0 [42] subscales are provided in Tables S2 and S3, Online Resource 1 for the pwME/CFS and pwPCC, respectively.
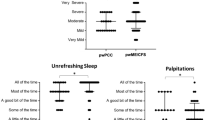
ME/CFS
Poorer scores in most SF-36v2 [41] domains (including Physical Functioning, Role Physical, Bodily Pain, Vitality and Social Functioning) were observed in the presence of dyspnoea. Additionally, lower Physical Functioning, Role Physical and Social Functioning scores (indicating worsened QoL) were associated with light-headedness or dizziness. Nausea also had negative associations with Physical Functioning, General Health, Social Functioning and Mental Health. Other symptoms returning significant negative associations with SF-36v2 [41] domains included short-term memory loss (Social Functioning), myalgia (Bodily Pain), arthralgia (General Health) and sweating episodes (Role Emotional). Interestingly, muscle weakness returned positive associations with multiple SF-36v2 [41] domains, including Physical Functioning, Role Physical, Vitality and Social Functioning. General Health returned positive relationships with abdominal pain and lymphadenopathy. Headaches were associated with increased Social Functioning scores.
Upon performing robustness checks, myalgia and urinary disturbances gained significance for the Physical Functioning and Vitality models, respectively. Symptoms that lost significance included: muscle weakness (Physical Functioning, Role Physical and Social Functioning), light-headedness (Physical Functioning and Social Functioning), memory loss, headaches and nausea (Social Functioning), arthralgia, abdominal pain and lymphadenopathy (General Health), sweating (Role Emotional) and recurrent feelings of feverishness (Physical Functioning).
Like the regression models for the SF-36v2 [41] domains, dyspnoea was associated with poorer scores in all six WHODAS 2.0 [42] domains included in the present study. Urinary disturbances returned positive associations (indicating heightened disability) with Mobility and Life Activities 1. Worsened Self-Care scores were observed in the presence of light-headedness. Symptoms returning negative associations with WHODAS 2.0 [42] domains included myalgia (Mobility, Self-Care and Life Activities 1), arthralgia (Getting Along and Participation), sleep disturbances (Cognition, Mobility and Life Activities 1), unrefreshed sleep (Mobility and Self-Care), muscle weakness (Self-Care and Participation) and headaches (Cognition).
Following robustness checks, sensitivity to odour or taste and light-headedness gained significance for the Cognition model. Symptoms that lost significance included: sleep disturbances (Cognition and Life Activities 1), unrefreshed sleep (Mobility and Self-Care), muscle weakness (Self-Care and Participation), myalgia and urinary disturbances (Life Activities 1), headaches (Cognition) and arthralgia (Participation).
PCC
Cold extremities returned the most negative associations with SF-36v2 [41] domains, including Role Physical, Vitality and Social Functioning. Other symptoms that returned poorer scores in more than one SF-36v2 [41] domain included memory loss (Bodily Pain and Mental Health), headaches (Vitality and Social Functioning), dyspnoea (Physical Functioning and Social Functioning) and feverishness (Role Physical and Social Functioning). Additional symptoms returning negative associations included: altered bowel habits and laryngitis (Vitality), abdominal pain (General Health), sleep disturbances (Mental Health), muscle weakness (Physical Functioning) and bloating (Role Emotional). Positive associations with SF-36v2 [41] domains were observed for light-headedness (Bodily Pain and Role Emotional), lymphadenopathy and heart palpitations (General Health) and sensitivity to odour or taste (Bodily Pain).
Upon completing robustness checks, lymphadenopathy gained significance for the Role Physical model but lost significance for General Health. Similarly, altered bowel habits gained significance for Social Functioning but lost significance for Vitality. Other symptoms that lost significance included: headaches (Vitality and Social Functioning), cold extremities (Role Physical and Vitality), sensitivity to odour or taste and light-headedness (Bodily Pain), sleep disturbances (Mental Health), laryngitis (Vitality) and dyspnoea (Social Functioning).
Worsened scores in the Self-Care and Getting Along domains of the WHODAS 2.0 [42] were observed in the presence of abdominal pain. Feverishness was associated with poorer Cognition and Mobility scores. Other symptoms returning positive associations with WHODAS 2.0 [42] domains included memory loss and lymphadenopathy (Cognition), muscle weakness (Self-Care), dyspnoea (Mobility) and sweating (Getting Along). Light-headedness was associated with lower Cognition and Self-Care scores. Lymphadenopathy was a negative predictor of Life Activities 1 and feverishness returned positive associations with both Life Activities 1 and Participation. However, neither the Life Activities 1 nor the Participation regression model were statistically significant (p = 0.061 and p = 0.15, respectively).
Following robustness checks, feverishness gained significance for the Life Activities 1 model but lost significance for Mobility. Other symptoms that lost significance included: light-headedness (Cognition and Self-Care), abdominal pain and sweating (Getting Along), muscle weakness (Self-Care) and lymphadenopathy (Cognition).
Reliability statistics
The internal consistency values for each of the PROM domains are summarised in Table S4, Online Resource 1. All WHODAS 2.0 [42] domains returned a McDonald’s ω value greater than 0.7 and therefore had sufficient reliability among pwME/CFS and pwPCC. Most SF-36v2 [41] domains for which internal consistency could be calculated also returned a McDonald’s ω value greater than 0.7 except for Vitality (ω = 0.556).
Symptom clusters
Four clusters were identified from the hierarchical cluster analysis of symptom presence among the pwME/CFS and pwPCC (Fig S1). The sociodemographic information, illness characteristics and patient-reported outcome data of the four clusters are summarised in Table S5, Online Resource 1. Comparisons of and reliability statistics for the PROM domain scores across the four clusters are provided in Tables S6 and S7, Online Resource 1, respectively.
No significant differences were observed in the sociodemographic characteristics of the four clusters. Across the four clusters, Vitality and Role Physical consistently returned the poorest of the SF-36v2 [41] domain scores and Life Activities 1 and Participation were the greatest affected WHODAS 2.0 [42] domains. Significantly lower scores in the General Health domain of the SF-36v2 [41] were observed for Cluster 2 compared with Cluster 3 (median (M) = 25.00, quartile 1 to quartile 3 (Q1–Q3) = 16.67–31.25, 95% confidence interval (95%CI) = 16.67–25.00 and M = 45.83, Q1–Q3 = 29.17–75.00, 95%CI = 29.17–79.17, respectively; p < 0.05, corrected). Cluster 2 also returned significantly higher scores than Cluster 3 in the Cognition domain of the WHODAS 2.0 [42] (M = 55.00, Q1–Q3 = 45.00–60.00, 95%CI = 50.00–55.00 and M = 35.00, Q1–Q3 = 15.00–47.50, 95%CI = 15.00–50.00, respectively; p < 0.05, corrected). All PROM subscales for which internal consistency statistics could be generated returned a McDonald’s ω value greater than 0.7 except for the Participation domain of the WHODAS 2.0 [42] (ω = 0.699). The distribution of illness status was not significantly different across the clusters after adjustment for multiple comparisons (p > 0.05, corrected). However, the clusters differed significantly in the distribution of the most stringent ME/CFS criteria met (p < 0.001, uncorrected), illness duration (p = 0.011, uncorrected) and the total number of symptoms (p < 0.001, uncorrected).
Complete descriptive statistics of symptom presentation, comparisons between the four clusters and results of post-hoc analyses are summarised in Table S8, Online Resource 1. The distributions of severity and frequency for each symptom among the four clusters are provided in Tables S9 and S10, Online Resource 1, respectively. Across the four clusters, there were no significant differences in the presentation of hallmark ME/CFS symptoms (including post-exertional malaise, impaired concentration and unrefreshed sleep) upon adjustment for multiple comparisons. Muscle weakness was the only symptom to differ in severity across the four clusters (p = 0.0057, uncorrected) and no symptoms were significantly different in frequency. However, the prevalence of all thermostatic, cardiovascular and gastrointestinal symptoms, as well as most pain and neurosensory symptoms, differed significantly across the four clusters.
Cluster 1
Excluding the hallmark ME/CFS symptoms, the most common symptoms among the Cluster 1 participants included sleep disturbances (n = 21/21, 100.0%), altered bowel habits (n = 17/21, 81.0%) and myalgia (n = 16/21, 76.2%). Symptoms low in prevalence among the Cluster 1 participants included memory loss (n = 5/21, 23.8%), lymphadenopathy (n = 3/21, 14.3%), palpitations (n = 4/21, 19.0%), sweating (n = 3/21, 14.3%) and feverishness (n = 3/21, 14.3%). Illness presentation was largely comparable between Clusters 1 and 3. Where significant differences between these two clusters existed, most lay in the prevalence of gastrointestinal symptoms.
All neurosensory symptoms (except sensitivity to odour or taste) affected at least half of the Cluster 1 participants. Cluster 1 had a significantly higher prevalence of photophobia (n = 15/21, 71.4%) compared with Cluster 3 (p < 0.05, corrected). However, the prevalence of muscle weakness was lowest in Cluster 1 (n =11/21, 52.4%) and significantly lower when compared with Cluster 2 (p < 0.05, corrected). Cluster 1 also returned the lowest prevalence of memory loss, which was significantly less common when compared with Clusters 2 and 4 (both p < 0.05, corrected). Cluster 1’s prevalence of arthralgia (n = 9/21, 42.9%) and abdominal pain (n = 8/21, 38.1%) was significantly less prevalent when compared with Cluster 2 (both p < 0.05, corrected).
Altered bowel habits were significantly more common in Cluster 1 compared with Clusters 3 and 4 (both p < 0.05, corrected). Bloating was also significantly more prevalent in Cluster 1 than Cluster 3 (p < 0.05, corrected). However, nausea was reported by less than half of the Cluster 1 participants and was significantly less prevalent when compared with Cluster 2 (p < 0.05, corrected).
Cluster 1’s prevalence of laryngitis (n = 11/21, 52.4%), palpitations (n = 4/21, 19.0%), light-headedness (n = 13/21, 61.9%), sweating (n = 3/21, 14.3%) and feverishness (n = 3/21, 14.3%) was the lowest of the four clusters – all (except laryngitis) of which were significantly lower compared with Cluster 2 (all p < 0.05, corrected). Palpitations and light-headedness were also significantly less common in Cluster 1 than Cluster 3 (both p < 0.05, corrected). Lymphadenopathy (n = 11/21, 52.4%) was significantly less prevalent in Cluster 1 than Clusters 2 and 4 (both p < 0.05, corrected) and was, along with sweating and feverishness, among the least common symptoms experienced by the Cluster 1 participants.
Cluster 2
Cluster 2 had the largest symptom burden and returned the highest prevalence of the four clusters for most symptoms. The Cluster 2 participants also experienced significantly more symptoms in total (M=20, Q1–Q3 = 18–22, 95%CI = 19–22 symptoms) when compared with all other clusters (all p < 0.05, corrected). Illness duration was longest among the Cluster 2 participants (M = 11.00, Q1–Q3 = 3.50–21.00, 95%CI = 5.00–18.00 years, data missing for n = 1 pwPCC from Cluster 2) and significantly longer compared with Clusters 1 and 3 (both p <0.05, corrected). Cluster 2 had the highest proportion of participants fulfilling the ICC [5] (n = 24/33, 72.7%), which was significantly higher when compared with Cluster 3 (p < 0.05, corrected).
Sweating (n = 23/33, 69.7%), nausea (n = 31/33, 93.9%) and abdominal pain (n = 31/33, 93.9%) were significantly higher among Cluster 2 than all other clusters (all p < 0.05, corrected). Cluster 2’s prevalence was also significantly higher than that of Clusters 1 and 3 for arthralgia (n = 29/33, 87.9%) and lymphadenopathy (n = 16/33, 48.5%), Clusters 1 and 4 for muscle weakness (n = 32/33, 97.0%), Clusters 3 and 4 for altered bowel habits (n =31/33, 93.9%), Cluster 1 alone for memory loss (n =26/33, 78.8%), palpitations (n = 20/33, 60.6%), light-headedness (n = 31/33, 93.9%), sweating, and feverishness (n = 18/33, 54.5%) and Cluster 3 alone for myalgia (n = 32/33, 97.0%), photophobia (n = 28/33, 84.8%), sensitivity to noise or vibration (n = 29/33, 87.9%) and bloating (n = 25/33, 75.8%) (all p < 0.05, corrected). Muscle weakness was more severe for Cluster 2 when compared with Clusters 3 and 4 (both p < 0.05, corrected).
Cluster 3
Other than the cardinal symptoms of ME/CFS, the most prominent symptoms in Cluster 3 were light-headedness (n = 9/9, 100.0%), headaches (n = 8/9, 88.9%), muscle weakness (n = 6/9, 66.7%), laryngitis (n = 6/9, 66.7%) and palpitations (n = 6/9, 66.7%). Cluster 3 had the most significant differences with Cluster 2.
Cluster 3’s prevalence of myalgia (n = 5/9, 55.6%) was the lowest of the four clusters and significantly lower when compared with Cluster 2 (p < 0.05, corrected). Excluding headaches, Cluster 3 had the lowest prevalence of all other pain symptoms, including arthralgia (n = 2/9, 22.2%) and abdominal pain (n = 1/9, 11.1%) – both of which were significantly less prevalent when compared with Cluster 2 (p < 0.05, corrected). All neurosensory symptoms, except muscle weakness, were lowest in prevalence in Cluster 3, including photophobia (n = 2/9, 22.2%), sensitivity to noise or vibration (n = 2/9, 22.2%) and sensitivity to odour or taste (n = 1/9, 11.1%). When compared with Cluster 3, photophobia was significantly more prevalent in Clusters 1, 2 and 4 (all p < 0.05, corrected) and sensitivity to noise or vibration was significantly more common in Clusters 2 and 4 (both p < 0.05, corrected).
Of the four clusters, Cluster 3 returned the lowest prevalence of all gastrointestinal symptoms. Prevalence was significantly lower among the Cluster 3 participants for nausea (n = 1/9, 11.1%) when compared with Clusters 2 and 4, bloating (n = 0/9, 0.0%) when compared with Clusters 1, 2 and 4 and altered bowel habits (n = 1/9, 11.1%) when compared with Clusters 1 and 2 (all p < 0.05, corrected). Among the Cluster 3 participants, prevalence was also significantly lower for lymphadenopathy (n = 0/9, 0.0%) when compared with Clusters 2 and 4 and sweating (n = 2/9, 22.2%) when compared with Cluster 2 (all p < 0.05, corrected).
Cluster 4
Cluster 4 was largely comparable with Cluster 2 and had the second-highest median total number of symptoms (M = 16, Q1–Q3 = 14–18, 95%CI = 14–18 symptoms), which was significantly higher when compared with Cluster 3 (p < 0.05, corrected). Among the Cluster 4 participants, prevalence was significantly lower than that of Clusters 1 and 2 for altered bowel habits (n = 4/27, 14.8%), and Cluster 2 alone for abdominal pain (n = 13/27, 48.1%), muscle weakness (n = 18/27, 66.7%) and sweating (n = 6/27, 22.2%) (all p < 0.05, corrected). Altered bowel habits and urinary disturbances were among the least common symptoms in Cluster 4 (both n = 4/27, 14.8%). Among the Cluster 4 participants, the prevalence of nausea (n = 17/27, 63.0%) and bloating (n = 16/27, 59.3%) was significantly higher than that of Cluster 3 but significantly lower than Cluster 2 (all p < 0.05, corrected).
Discussion
The present pilot study documents symptom clusters among pwME/CFS and pwPCC and identifies associations between symptoms and patient-reported outcomes. To the authors’ knowledge, this is the first study to identify symptom clusters in a collective population of pwME/CFS and pwPCC. Importantly, none of the four clusters were specific to ME/CFS or PCC. These novel findings further characterise the illness presentation of PCC to inform developments in the diagnostic criteria of this emergent condition. This study also serves to inform changes to approaches to care and service delivery for pwME/CFS and pwPCC by providing detailed analyses of symptom burden on QoL and functioning. Symptoms were associated with poorer scores in all measures of QoL and functional capacity among both illness cohorts. This reflects the widespread and complex impacts of ME/CFS and PCC on daily living and functioning and, therefore, the need for access to multidisciplinary care and support [1, 3, 7, 8].
Furthermore, this study highlights symptoms that contribute to worsened health outcomes among pwME/CFS and pwPCC, which may signify priority areas for symptom management in clinical practice. Autonomic symptoms appeared the most burdensome and returned poorer patient-reported outcomes across most domains among both pwME/CFS and pwPCC. Interestingly, while negative associations were observed among both illness cohorts, the presence of dyspnoea had a pronounced impact on pwME/CFS. This may be due to case criteria requirements. PwME/CFS must experience a defined set of symptoms to meet diagnostic criteria; however, the presence of respiratory symptoms is not compulsory [5, 6]. Therefore, dyspnoea (in addition to the mandatory, hallmark symptoms of ME/CFS) may further compound existing reductions in QoL and functional capacity.
The contribution of thermostatic intolerance, memory loss, pain, sleep disturbances and muscle weakness to illness burden also varied between pwME/CFS and pwPCC. Thermostatic intolerance was associated with poorer scores in several PROM subscales among pwPCC. However, the only association for this symptom group observed among pwME/CFS was sweating with the Role Emotional domain of the SF-36v2 [41]. Additionally, memory loss was burdensome in both illness cohorts but returned more negative associations with patient-reported outcomes among pwPCC. Furthermore, pain (notably myalgia), muscle weakness and sleep disturbances were associated with increased QoL and functional capacity among pwME/CFS but only returned poor patient-reported outcomes among pwPCC.
These results may be explained by changes in illness presentation over time. Whilst the long-term prognosis of PCC is not yet known, existing ME/CFS literature has noted that the burden of symptoms may evolve as the illness progresses [11, 12]. Among pwME/CFS, the burden of neurocognitive and autonomic dysfunction appears to increase over time and surpass that of flu-like and inflammatory symptoms, which may be more pronounced in earlier stages of illness [11, 12]. This is further supported by the increased total number of symptoms, as well as higher prevalence of gastrointestinal and neurosensory symptoms, observed among clusters with longer illness duration in the present study.
Negative associations between QoL and gastrointestinal symptoms, namely nausea, were also more pronounced among pwME/CFS in this study. Comorbid gastrointestinal disorders appear common in ME/CFS, with up to 60% of pwME/CFS experiencing IBS [48, 49]. New-onset IBS has also been disproportionately observed among COVID-19 survivors [50]. The pathophysiological mechanisms underpinning gastrointestinal symptoms in ME/CFS and PCC remain unclear. Additionally, the burden of gastrointestinal symptoms among pwPCC varies in the existing literature and has been described as both comparable to and less than that experienced by pwME/CFS [22, 51, 52]. Nevertheless, the results of the present study reiterate the importance of identifying and managing potential comorbid gastrointestinal disorders and related symptoms (as outlined in clinical guidelines for ME/CFS [4, 9, 53, 54]) to reduce further implications on QoL.
It is also worth noting that, as some symptoms that returned positive associations with patient-reported outcomes were highly prevalent, the sample sizes of participants not experiencing these symptoms were small. Consequently, the relative increases in QoL and functional capacity among these participants may not be truly representative. Importantly, the associations between symptoms and patient-reported outcomes observed in the present study are relative to the presence of other symptoms and positive associations should not be interpreted as minimising the burden of these symptoms on the lives of pwME/CFS and pwPCC.
Despite some differences in the regression analyses, pwME/CFS could not be distinguished from pwPCC through hierarchical cluster analysis of symptom presence. There were no significant differences in the prevalence, severity or frequency of hallmark ME/CFS symptoms across the four clusters. Differences in patient-reported outcomes across the four clusters were marginal. The Cognition domain of the WHODAS 2.0 [42] was significantly more impaired among the Cluster 2 than Cluster 3 participants. Friedberg et al. [55] observed a worsening of cognitive symptoms among pwME/CFS over time. However, Cluster 2 (while characterised by a significantly longer illness duration) did not differ from Cluster 3 in the prevalence, severity or frequency of cognitive disturbances. The disparities in the scores for the General Health domain of the SF-36v2 [41] among the Cluster 2 and Cluster 3 participants likely align with the differences in illness duration [12, 56], as the General Health subscale queries self-perceptions of health in comparison to others, as well as self-perceptions of future health [41].
Clusters 2 and 3 had the lowest comparability of all the clusters. These two clusters were the only cluster pair to differ significantly in measures of QoL and functional capacity, as well as in the distribution of fulfilling the ICC [5] case definition for ME/CFS. The likelihood of spontaneously recovering from ME/CFS is highest within the first two years following illness onset [11, 12]. This could explain the lower prevalence of many symptoms in Cluster 3, which returned the shortest median illness duration of 1.58 years. Hence, these cluster analysis findings may suggest that the illness burden of ME/CFS and PCC accumulates over time. Similarly, as the four symptom clusters appeared to be differentiated largely by the presence of gastrointestinal and neurosensory disturbances, an increased burden of these symptoms may potentially indicate a later stage of illness.
This postulation is supported by the regression results of the present study, as well as the increased burden of autonomic and neurosensory symptoms as ME/CFS progresses [11, 12]. Following cluster analyses of pwME/CFS fulfilling the Fukuda criteria [57], Słomko et al. [58] also documented poorer QoL and worsened fatigue in a cluster defined by autonomic dysfunction. Participants in this cluster returned a higher burden of autonomic symptoms, poorer scores in autonomic function tests, greater fatigue impact and severity, higher prevalence of post-exertional malaise and the lowest QoL of the four identified clusters [58].
Publications investigating clusters among pwPCC have similarly identified subgroups delineated by the prevalence of flu-like symptoms and pain when compared with neurocognitive and gastrointestinal symptoms [31, 33, 59,60,61]. However, further longitudinal research is necessary to determine whether the contributors to PCC burden shift to resemble those of ME/CFS over time. Cluster analyses among COVID-19 survivors have suggested that a greater number of symptoms and increased symptom severity during acute SARS-CoV-2 infection may be associated with an increased likelihood of PCC development, as well as a heightened PCC symptom burden [33, 60, 61]. However, the indicators of recovery from or persistence of PCC have not been well-described. The present paper therefore provides novel insight into the potential illness trajectory of PCC. Future longitudinal research is warranted to determine the role of post-acute symptom presentation in predicting long-term PCC prognosis.
Strengths and limitations
There are limitations to this study, including the small sample size and cross-sectional nature. To confirm the role of illness duration in the differences observed in the present study, pwPCC should be matched with pwME/CFS with comparable illness durations in future studies to further evaluate PCC as an equivalent model to the early stages of ME/CFS. Additionally, the contributions of each symptom to patient-reported outcomes reported in this study are relative to other symptoms. Hence, the regression analyses reported herein do not convey the crude impact of ME/CFS and PCC symptoms (particularly hallmark ME/CFS symptoms, which were ubiquitous among the study population) on QoL and functional capacity. Finally, the results presented in this study may not accurately represent pwME/CFS and pwPCC who belong to marginalised populations.
The use of validated PROMs to mitigate observer bias was a strength of the present investigation. This study also benefited from having multiple methods of survey administration. Participants were able to complete the questionnaire online, as an offline digital or paper copy, or over the phone to allow for flexibility in participation. The questionnaire was also suitable to be completed with assistance from a family member, friend or support worker and could be paused and recommenced at any time to enable participants experiencing severe illness to participate in the research.
Importantly, this study provides detailed analyses of the illness presentation of ME/CFS and PCC to inform care pathways for people who live with these conditions. The impairments in all patient-reported outcomes observed in this study necessitate access to multidisciplinary care services for pwME/CFS and pwPCC. Additionally, as autonomic symptoms (such as respiratory and gastrointestinal issues) were noteworthy contributors in the regression and cluster analyses, the present study highlights the potential importance of prioritising these symptoms in the management of ME/CFS and PCC to prevent further deteriorations in QoL and functioning. This study also documents novel data among an Australian cohort of pwME/CFS and pwPCC to inform national health policies that determine access to care and support services. Finally, the findings of this study also serve to inform PCC case definitions. The noteworthy similarities between these conditions observed in this study reiterate the importance of identifying pwPCC experiencing ME/CFS-like illness to deliver early interventions and optimise health outcomes.
Conclusion
Autonomic symptoms appear to contribute to a worsened illness burden among both pwME/CFS and pwPCC. However, associations of thermostatic intolerance, memory loss, pain, sleep disturbances and muscle weakness with QoL and functional capacity varied between the two illness cohorts. While four symptom clusters were identified, none were unique to ME/CFS or PCC. This further implicates ME/CFS as a potential post-infectious sequela of acute COVID-19 illness and reiterates the possible benefit of shared management approaches. Longitudinal research is warranted to confirm the relationship between cluster status and illness progression. Meanwhile, the numerous negative associations between symptoms and patient-reported outcomes in the present study emphasises the importance of multidisciplinary and person-centred care and support for all pwME/CFS and pwPCC.
Data availability
The datasets generated and analysed that support the findings of the current study are not publicly available due to confidentiality agreements. However, these datasets are available from the corresponding author upon reasonable request.
Change history
17 October 2024
Supplementary information file (Figure S1) is included.
Abbreviations
- 95%CI:
-
95% confidence interval
- AIC:
-
Akaike Information Criterion
- ANCOVA:
-
Analysis of Covariance
- BMI:
-
Body mass index
- C:
-
Consensus
- CCC:
-
Canadian Consensus Criteria
- HREC:
-
Human research ethics committee
- IBS:
-
Irritable Bowel Syndrome
- ICC:
-
International Consensus Criteria
- M:
-
Median
- ME/CFS:
-
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
- NA:
-
Not applicable
- NCNED:
-
National Centre for Neuroimmunology and Emerging Diseases
- PCC:
-
Post COVID-19 Condition
- PROM:
-
Patient-reported outcome measure
- PwME/CFS:
-
People/person with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
- PwPCC:
-
People/person with Post COVID-19 Condition
- Q1–Q3:
-
Quartile 1 to quartile 3
- QoL:
-
Quality of life
- SARS-CoV-2:
-
Sudden Acute Respiratory Syndrome Coronavirus-2
- SF-36v2:
-
36-Item Short-Form Health Survey (version 2)
- SPSS:
-
Statistical Package for the Social Sciences
- WHO:
-
World Health Organization
- WHODAS 2.0:
-
World Health Organization Disability Assessment Schedule (version 2.0)
References
Eaton-Fitch, N., Johnston, S. C., Zalewski, P., Staines, D. R., & Marshall-Gradisnik, S. M. (2020). Health-related quality of life in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: An Australian cross-sectional study. Quality of Life Research, 29(6), 1521–1531. https://doi.org/10.1007/s11136-019-02411-6
Cambras, T., Castro-Marrero, J., Zaragoza, M. C., Díez-Noguera, A., & Alegre, J. (2018). Circadian rhythm abnormalities and autonomic dysfunction in patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. PLoS One, 13(6), e0198106. https://doi.org/10.1371/journal.pone.0198106
Strand, E. B., Mengshoel, M., Sandvik, A., Helland, L., Abraham, I. B. S., & Solberg Nes, L. (2019). Pain is associated with reduced quality of life and functional status in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Scandinavian Journal of Pain, 19(1), 61–72. https://doi.org/10.1515/sjpain-2018-0095
Baraniuk, J. (2022). Myalgic Encephalomyelitis (Chronic Fatigue Syndrome). BMJ Best Practice. Retrieved October 23, 2023, from https://bestpractice.bmj.com/topics/en-gb/277
Carruthers, B. M., Van de Sande, M. I., De Meirleir, K. L., Klimas, N. G., Broderick, G., Mitchell, T., Staines, D. R., Powles, A. C. P., Speight, N., Vallings, R., Bateman, L., Baumgarten-Austrheim, B., Bell, D. S., Carlo-Stella, N., Chia, J., Darragh, A., Jo, D., Lewis, D., Light, A. R., … Stevens, S. (2011). Myalgic Encephalomyelitis: International consensus criteria. Journal of Internal Medicine, 270(4), 327–338. https://doi.org/10.1111/j.1365-2796.2011.02428.x.
Carruthers, B. M., Jain, A. K., De Meirleir, K. L., Peterson, D. L., Klimas, N. G., Lerner, A. M., Bested, A. C., Flor-Henry, P., Joshi, P., Powles, A. C. P., Sherkey, J. A., & Van de Sande, M. I. (2003). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Journal Of Chronic Fatigue Syndrome, 11(1), 7–115. https://doi.org/10.1300/J092v11n01_02
Chang, C. J., Hung, L. Y., Kogelnik, A. M., Kaufman, D., Aiyar, R. S., Chu, A. M., Wilhelmy, J., Li, P., Tannenbaum, L., Xiao, W., & Davis, R. W. (2021). A comprehensive examination of severely ill ME/CFS patients. Healthcare, 9(10). https://doi.org/10.3390/healthcare9101290
Johnston, S. C., Brenu, E. W., Hardcastle, S. L., Huth, T. K., Staines, D. R., & Marshall-Gradisnik, S. M. (2014). A comparison of health status in patients meeting alternative definitions for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Health and Quality of Life Outcomes, 12(1), 64. https://doi.org/10.1186/1477-7525-12-64
Bested, A. C., & Marshall, L. M. (2015). Review of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: An evidence-based approach to diagnosis and management by clinicians. Reviews on Environmental Health, 30(4), 223–249. https://doi.org/10.1515/reveh-2015-0026
Lim, E. J., Ahn, Y. C., Jang, E. S., Lee, S. W., Lee, S. H., & Son, C. G. (2020). Systematic review and meta-analysis of the prevalence of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME). Journal of Translational Medicine, 18(1), 100. https://doi.org/10.1186/s12967-020-02269-0
Chu, L., Valencia, I. J., Garvert, D. W., & Montoya, J. G. (2019). Onset patterns and course of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Frontiers in Pediatrics, 7, 12. https://doi.org/10.3389/fped.2019.00012
Nacul, L., O’Boyle, S., Palla, L., Nacul, F. E., Mudie, K., Kingdon, C. C., Cliff, J. M., Clark, T. G., Dockrell, H. M., & Lacerda, E. M. (2020). How Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) progresses: The natural history of ME/CFS. Frontiers in Neurology, 11. https://doi.org/10.3389/fneur.2020.00826
Johnston, S. C., Staines, D. R., & Marshall-Gradisnik, S. M. (2016). Epidemiological characteristics of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis in Australian patients. Journal of Clinical Epidemiology, 8, 97–107. https://doi.org/10.2147/CLEP.S96797
Jason, L. A., Yoo, S., & Bhatia, S. (2021). Patient perceptions of infectious illnesses preceding Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Chronic Illness, 18(4), 901–910. https://doi.org/10.1177/17423953211043106
Choutka, J., Jansari, V., Hornig, M., & Iwasaki, A. (2022). Unexplained post-acute infection syndromes. Nature Medicine, 28, 911–923. https://doi.org/10.1038/s41591-022-01810-6
Davis, H. E., McCorkell, L., Vogel, M., J., & Topol, E. J. (2023). Long COVID: Major findings, mechanisms and recommendations. Nature Reviews Microbiology, 21(3), 133–146. https://doi.org/10.1038/s41579-022-00846-2
Sukocheva, O. A., Maksoud, R., Beeraka, N. M., Madhunapantula, S. V., Sinelnikov, M., Nikolenko, V. N., Neganova, M. E., Klochkov, S. G., Kamal, A., Staines, M., D. R., & Marshall-Gradisnik, S. M. (2022). Analysis of Post COVID-19 Condition and its overlap with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Journal of Advanced Research, 40, 179–196. https://doi.org/10.1016/j.jare.2021.11.013
Wong, T. L., & Weitzer, D. J. (2021). Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) - a systematic review and comparison of clinical presentation and symptomatology. Medicina (Kaunas, Lithuania), 57(5), 418. https://doi.org/10.3390/medicina57050418
Soriano, J. B., Allan, M., Alsokhn, C., Alwan, N. A., Askie, L., Davis, H. E., Diaz, J. V., Dua, T., De Groote, W., Jakob, R., Lado, M., Marshall, J., Murthy, S., Preller, J., Relan, P., Schiess, N., & Seahwag (2023). A. A clinical case definition of Post COVID-19 Condition by a Delphi consensus. World Health Organization: Geneva, Switzerland. Retrieved September 5, from https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1
Bonilla, H., Quach, T. C., Tiwari, A., Bonilla, A. E., Miglis, M., Yang, P. C., Eggert, L. E., Sharifi, H., Horomanski, A., Subramanian, A., Smirnoff, L., Simpson, N., Halawi, H., Sum-Ping, O., Kalinowski, A., Patel, Z. M., Shafer, R. W., & Geng, L. N. (2023). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome is common in post-acute sequelae of SARS-CoV-2 infection (PASC): Results from a post-COVID-19 multidisciplinary clinic. Frontiers in Neurology, 14. https://doi.org/10.3389/fneur.2023.1090747
Kedor, C., Freitag, H., Meyer-Arndt, L., Wittke, K., Hanitsch, L. G., Zoller, T., Steinbeis, F., Haffke, M., Rudolf, G., Heidecker, B., Bobbert, T., Spranger, J., Volk, H. D., Skurk, C., Konietschke, F., Paul, F., Behrends, U., Bellmann-Strobl, J., & Scheibenbogen, C. (2022). A prospective observational study of post-COVID-19 Chronic Fatigue Syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nature Communications, 13(1), 5104. https://doi.org/10.1038/s41467-022-32507-6
Weigel, B., Eaton-Fitch, N., Thapaliya, K., & Marshall-Gradisnik, S. M. (2024). Illness presentation and quality of life in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Post COVID-19 Condition: A pilot Australian cross-sectional study. Quality of Life Research. https://doi.org/10.1007/s11136-024-03710-3
Retornaz, F., Rebaudet, S., Stavris, C., & Jammes, Y. (2022). Long-term neuromuscular consequences of SARS-CoV-2 and their similarities with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Results of the retrospective CoLGEM study. Journal of Translational Medicine, 20(1), 429. https://doi.org/10.1186/s12967-022-03638-7
Vernon, S. D., Hartle, M., Sullivan, K., Bell, J., Abbaszadeh, S., Unutmaz, D., & Bateman, L. (2023). Post-exertional malaise among people with Long COVID compared to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). WORK: A Journal of Prevention, Assessment & Rehabilitation, 74(4), 1179–1186. https://doi.org/10.3233/WOR-220581
Twomey, R., DeMars, J., Franklin, K., Culos-Reed, S. N., Weatherald, J., & Wrightson, J. G. (2022). Chronic fatigue and postexertional malaise in people living with long COVID: An observational study. Physical Therapy & Rehabilitation Journal, 102(4), pzac005. https://doi.org/10.1093/ptj/pzac005
Davis, H. E., Assaf, G. S., McCorkell, L., Wei, H., Low, R. J., Re’em, Y., Redfield, S., Austin, J. P., & Akrami, A. (2021). Characterising Long COVID in an international cohort: 7 months of symptoms and their impact. The Lancet Discovery Science, 38(August 2021), 101019. https://doi.org/10.1016/j.eclinm.2021.101019
Alves de Sousa, K. C., Gardel, D. G., & Lopes, A. J. (2022). Postural balance and its association with functionality and quality of life in non-hospitalized patients with Post-Acute COVID-19 Syndrome. Physiotherapy Research International: The Journal for Researchers and Clinicians in Physical Therapy, 27(4), e1967. https://doi.org/10.1002/pri.1967
Cai, J., Lin, K., Zhang, H., Xue, Q., Zhu, K., Yuan, G., Sun, Y., Zhu, F., Ai, J., Wang, S., & Zhang, W. (2023). A one-year follow-up study of systematic impact of long COVID symptoms among patients post SARS-CoV-2 omicron variants infection in Shanghai, China. Emerging Microbes & Infections, 12(2), 2220578. https://doi.org/10.1080/22221751.2023.2220578
Martini Sasso, E., Muraki, K., Eaton-Fitch, N., Smith, P., Lesslar, O. L., Deed, G., & Marshall-Gradisnik, S. M. (2022). Transient receptor potential melastatin 3 dysfunction in Post COVID-19 Condition and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome patients. Molecular Medicine, 28(1), 98. https://doi.org/10.1186/s10020-022-00528-y
Komaroff, A. L., & Lipkin, W. I. (2021). Insights from Myalgic Encephalomyelitis/Chronic Fatigue Syndrome may help unravel the pathogenesis of Postacute COVID-19 Syndrome. Trends in Molecular Medicine, 27(9), 895–906. https://doi.org/10.1016/j.molmed.2021.06.002
Thaweethai, T., Jolley, S. E., Karlson, E. W., Levitan, E. B., Levy, B., McComsey, G. A., McCorkell, L., Nadkarni, G. N., Parthasarathy, S., Singh, U., Walker, T. A., Selvaggi, C. A., Shinnick, D. J., Schulte, C. C. M., Atchley-Challenner, R., Horwitz, L. I., Foulkes, A. S., & RECOVER Consortium Authors. (2023). Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA, 329(22), 1934–1946. https://doi.org/10.1001/jama.2023.8823
Basharat, S., Chao, Y. S., & McGill, S. C. (2024). Subtypes of Post-COVID-19 Condition: A review of the emerging evidence. Canadian Agency for Drugs and Technologies in Health: Ottawa, Canada. Retrieved April 23, from https://www.ncbi.nlm.nih.gov/books/NBK601826/
Fernández-de-las-Peñas, C., Martín-Guerrero, J. D., Florencio, L. L., Navarro-Pardo, E., Rodríguez-Jiménez, J., Torres-Macho, J., & Pellicer-Valero, O. J. (2022). Clustering analysis reveals different profiles associating long-term post-COVID symptoms, COVID-19 symptoms at hospital admission and previous medical co-morbidities in previously hospitalized COVID-19 survivors. Infection, 51(1), 61–69. https://doi.org/10.1007/s15010-022-01822-x
Bateman, L., Bested, A. C., Bonilla, H. F., Chheda, B. V., Chu, L., Curtin, J. M., Dempsey, T. T., Dimmock, M. E., Dowell, T. G., Felsenstein, D., Kaufman, D. L., Klimas, N. G., Komaroff, A. L., Lapp, C. W., Levine, S. M., Montoya, J. G., Natelson, B. H., Peterson, D. L., Podell, R. N., … Yellman, B. P. (2021). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of diagnosis and management. Mayo Clinic Proceedings, 96(11):2861–78. https://doi.org/10.1016/j.mayocp.2021.07.004
Maixner, W., Fillingim, R. B., Williams, D. A., Smith, S. B., & Slade, G. D. (2016). Overlapping chronic pain conditions: Implications for diagnosis and classification. The Journal of Pain, 17(9 Suppl), T93–107. https://doi.org/10.1016/j.jpain.2016.06.002
Raveendran, A. V., Jayadevan, R., & Sashidharan, S. (2021). Long COVID: An overview. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 15(3), 869–875. https://doi.org/10.1016/j.dsx.2021.04.007
National Health and Medical Research Council, Australian Research Council, & Universities Australia. National Statement on Ethical Conduct in Human Research. National Health and Medical Research Council: Canberra, Australia. Retrieved June 19 (2024). from https://www.nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2023
World Medical Association. (2013). World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. https://doi.org/10.1001/jama.2013.281053
Von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., & Vandenbroucke, J. P. (2008). The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Journal of Clinical Epidemiology, 61(4), 344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008
World Health Organization Constitution of the World Health Organization. World Health Organization: Geneva, Switzerland. Retrieved September 1, 2024, from https://www.who.int/about/governance/constitution
Ware, J. E. Jr (2000). SF-36 Health Survey Update. Spine, 25(24), 3130–3139. https://doi.org/10.1097/00007632-200012150-00008
Üstün, T. B., Kostanjsek, N., Chatterji, S., Rehm, J., & World Health Organization. &. Measuring health and disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). World Health Organization: Geneva, Switzerland. Retrieved September 20, 2023, from https://www.who.int/publications/i/item/measuring-health-and-disability-manual-for-who-disability-assessment-schedule-(-whodas-2.0).
Nittas, V., Gao, M., West, E. A., Ballouz, T., Menges, D., Hanson, W., S., & Puhan, M. A. (2022). Long COVID through a public health lens: An umbrella review. Public Health Reviews, 43, 1604501. https://doi.org/10.3389/phrs.2022.1604501
Corp, I. B. M. (Released 2022). IBM Statistical Package for the Social Sciences (SPSS) statistics for Windows, Version 29.0. Armonk, New York: IBM Corp.
Lang, T. A., & Altman, D. G. (2023). Basic statistical recording for articles published in biomedical journals: The Statistical Analyses and Methods in the Published Literature or The SAMPL Guidelines. In: Smart P, Maisonneuve H, Polderman A (Eds.). Science Editor’s Handbook, 2nd Ed. European Association of Science Editors: Cornwall, United Kingdom. Retrieved November 20, from https://www.equator-network.org/wp-content/uploads/2013/07/SAMPL-Guidelines-6-27-13.pdf
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B (Methodology), 57(1), 289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x
Stensen, K., & Lydersen, S. (2022). Internal consistency: From alpha to omega. Tidsskr Nor Laegeforen, 142(12). https://doi.org/10.4045/tidsskr.22.0112
Weigel, B., Eaton-Fitch, N., Passmore, R., Cabanas, H., Staines, D., & Marshall-Gradisnik, S. (2020). Gastrointestinal symptoms, dietary habits, and the effect on health-related quality of life among Australian Myalgic Encephalomyelitis/Chronic Fatigue Syndrome patients: A cross-sectional study. Annals of Epidemiology and Public Health, 3(1), 1045. https://meddocsonline.org/annals-of-epidemiology-and-public-health/gastrointestinal-symptoms-dietary-habits-and-the-effect-on-health-related-quality-of-life-among-australian-myalgic-encephalomyelitis-chronic-fatigue-syndrome-patients-a-cross-sectional-study.pdf
Castro-Marrero, J., Faro, M., Aliste, L., Sáez-Francàs, N., Calvo, N., Martínez-Martínez, A., de Fernández, T., & Alegre, J. (2017). Comorbidity in Chronic Fatigue Syndrome/Myalgic encephalomyelitis: A nationwide population-based cohort study. Psychosomatics, 58(5), 533–543. https://doi.org/10.1016/j.psym.2017.04.010
Marasco, G., Maida, M., Cremon, C., Raffaella Barbaro, M., Stranghellini, V., & Barbara, G. (2023). Meta-analysis: Post-COVID-19 functional dyspepsia and irritable bowel syndrome. Aliment Pharmacol Ther, 58(1), 6–15. https://doi.org/10.1111/apt.17513
Jason, L. A., Islam, M. F., Conroy, K., Cotler, J., Torres, C., Johnson, M., & Mabie, B. (2021). COVID-19 symptoms over time: Comparing long-haulers to ME/CFS. Fatigue Biomed Health Behav, 9(2), 59–68. https://doi.org/10.1080/21641846.2021.1922140
Azcue, N., Gómez-Esteban, J. C., Acera, M., Tijero, B., Fernandez, T., Ayo-Mentxakatorre, N., Pérez-Concha, T., Murueta-Goyena, A., Lafuente, J. V., Prada, Á., de López, A., Ruiz-Irastorza, G., Ribacoba, L., Gabilondo, I., & Del Pino, R. (2022). Brain fog of Post-COVID-19 Condition and Chronic Fatigue Syndrome, same medical disorder? J Transl Med, 20(1), 569. https://doi.org/10.1186/s12967-022-03764-2
Myalgic Encephalomyelitis - Adult and paediatric: International consensus primer for medical practitioners. Retrieved May 31, 2024, from http://www.investinme.org/Documents/Guidelines/Myalgic%20Encephalomyelitis%20International%20Consensus%20Primer%20-2012-11-26.pdf.
Friedberg, F., Bateman, L., Bested, A. C., Davenport, T., Friedman, K. J., Gurwitt, A., Jason, L. A., Lapp, C. W., Stevens, S. R., Underhill, R. A., & Vallings, R. (2014). Chronic Fatigue Syndrome/Myalgic Encephalomyelitis - Primer for clinical practitioners. 2014 Edition. International Association of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Retrieved June 17, 2024, from https://massmecfs.org/images/pdf/Primer_2014.pdf
Friedberg, F., Dechene, L., McKenzie, M. J., II, & Fontanetta, R. (2000). Symptom patterns in long-duration Chronic Fatigue Syndrome. Journal of Psychosomatic Research, 48(1), 59–68. https://doi.org/10.1016/S0022-3999(99)00077-X
Megari, K. (2013). Quality of life in chronic disease patients. Health Psychology Research, 1(3), e27. https://doi.org/10.4081/hpr.2013.e27
Fukuda, K., Straus, S. E., Hickie, I., Sharpe, M. C., Dobbins, J. G., & Komaroff, A. (1994). The Chronic Fatigue Syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine, 121(12), 953–959. https://doi.org/10.7326/0003-4819-121-12-199412150-00009
Słomko, J., Estévez-López, F., Kujawski, S., Zawadka-Kunikowska, M., Tafil-Klawe, M., Klawe, J. J., Morten, K. J., Szrajda, J., Murovska, M., Newton, J. L., & Zalewski, P. (2020). Autonomic phenotypes in Chronic Fatigue Syndrome (CFS) are associated with illness severity: A cluster analysis. Journal of Clinical Medicine, 9, 2531. https://doi.org/10.3390/jcm9082531. & The European Network on ME/CFS (EUROMENE).
Goldhaber, N. H., Kohn, J. N., Ogan, W. S., Sitapati, A., Longhurst, C. A., Wang, A., Lee, S., Hong, S., & Horton, L. E. (2022). Deep dive into the long haul: Analysis of symptom clusters and risk factors for post-acute sequelae of COVID-19 to inform clinical care. International Journal of Environmental Research and Public Health, 19(24), 16841. https://doi.org/10.3390/ijerph192416841
Fischer, A., Zhang, L., Elbéji, A., Wilmes, P., Oustric, P., Staub, T., Nazarov, P. V., Ollert, M., & Fagherazzi, G. (2022). Long COVID symptomatology after 12 months and its impact on quality of life according to initial Coronavirus Disease 2019 disease severity. Open Forum Infectious Diseases, 9(8), ofac397. https://doi.org/10.1093/ofid/ofac397
Van den Houdt, S. C. M., Slurink, I. A. L., & Mertens, G. (2024). Long COVID is not a uniform syndrome: Evidence from a person-level symptom clusters using latent class analysis. Journal of Infection and Public Health, 17(2), 321–328. https://doi.org/10.1016/j.jiph.2023.12.019
Funding
This research was supported by The Stafford Fox Medical Research Foundation (489798), The National Health and Medical Research Council (1199502), The Mason Foundation (47107), The McCusker Charitable Foundation (49979), Talei Stewart, The Buxton Foundation (4676), Henty Community (4879), Blake Beckett Trust Foundation (4579), Alison Hunter Memorial Foundation (4570), The Change for ME Charity (4575) and Dr John Hamwood. The authors declare that the funders had no role in the study design, collection or analysis of data, decision to publish or preparation of the present manuscript.
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
The present study forms part of the PhD dissertation of BW. NE-F and SM-G conceptualised this study and developed the necessary resources and methodology. Formal analysis, data collection and writing of the original draft was performed by BW and NE-F. KT and SM-G conducted quality assurance of the data analysis and critically reviewed and edited manuscript drafts. SM-G supervised and acquired the funding for this research. All authors contributed substantially to the present manuscript and have approved the final, submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained for the present study from the Griffith University HREC (Reference Number: 2019/1005) and the Gold Coast University Hospital HREC (Reference Number: HREC/2019/QGC/56469). Access to the online questionnaire was granted upon agreement to a mandatory consent question, ensuring that informed consent was electronically obtained from all study participants prior to their participation. The present study was conducted in accordance with the Griffith University Research Ethics Manual, the Australian Government National Health and Medical Research Council National Statement on Ethical Conduct in Human Research 2023 [37] and the World Medical Association Declaration of Helsinki [38].
Consent to publish
Prior to participation, all study participants provided informed consent for the publication of their data as unidentifiable, combined group results.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weigel, B., Eaton-Fitch, N., Thapaliya, K. et al. A pilot cross-sectional investigation of symptom clusters and associations with patient-reported outcomes in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Post COVID-19 Condition. Qual Life Res 33, 3229–3243 (2024). https://doi.org/10.1007/s11136-024-03794-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-024-03794-x