Abstract
COVID-19 pandemic is associated with devastating effects on social, psychological, and economical aspects of survivors. We assume that erectile function (EF) is affected as well. We performed a systematic review of the published articles about the change in EF among patients and health care providers during the COVID-19 pandemic. We searched PubMed and Cochrane databases for English literature using a combination of medical subject headings (MeSH) terms and keywords. We extracted data of erectile dysfunction (ED) rate, international index of erectile function (IIEF), changes related to exposure to the pandemic (Primary objectives), and factors affecting these differences (Secondary objectives). Twenty articles were included in the screening phase. Only 3 articles were eligible for primary objectives, and 2 articles were included for the secondary objective. Three articles revealed an increase in ED cases and a reduction in IIEF-5 scores during the pandemic. Rates of ED have ranged from 32% to 87% of the study populations. Anxiety, depression, and post-traumatic stress disorder (PTSD) were associated with increased ED rates. We conclude that the COVID-19 pandemic is associated with increased rates of ED. Anxiety and depression augment this increase. Health care providers are at higher risk for PTSD, which increases the risk of ED.
Similar content being viewed by others
Introduction
In 2020, World Health Organization declared COVID-19 as a pandemic [1]. Since then, the number of affected individuals was globally increasing [2]. Mortality rates were also increased to numbers that were not previously accustomed since the Spanish flu and World Wars [2, 3]. Numbers were publicly announced on daily basis. Health care systems were markedly burdened [4], and many countries have suffered from severe deficiencies in medical supplies [5]. Accordingly, all countries have obligated their people to follow lockdown policies to prevent further spread, and many families were further loaded at economic and social levels.
Several reports showed that sexual function was affected during and after the pandemic [6,7,8,9,10]. The number of diagnosed cases with sexual dysfunction was increased among males [11] and females [12, 13]. Men’s complaints have included decreased libido and orgasm [14], erectile dysfunction (ED) [6], and decreased sexual satisfaction in comparison to a pre-COVID state [15]. Of note that many patients have reported a decrease in erectile function (EF), which was confirmed by a reduction of their international index of erectile function (IIEF) assessment [16].
The high incidence of sexual dysfunction during the pandemic was the interest of several studies that tried to address the underlying etiology. Assumptions of biological underlying mechanisms such as hypogonadism, endothelial and cardiopulmonary dysfunction were proposed [17]. On the other hand, several other studies have shown that psychological disturbances, e.g., anxiety or depression, were the principal underlying etiology of sexual dysfunction during the pandemic [7, 15, 16].
This article has reviewed the status of EF among patients and health care providers during the COVID-19 pandemic. Further, it has addressed the social and economic effects of lockdown as proposed risk factors for ED.
The rationale of the current study was to demonstrate whether a realistic association would be present between the COVID-19 pandemic and ED and to identify the factors that may affect changes in EF during the pandemic. This study highlighted the need for more prospective research to identify the possible underlying etiology of ED during the COVID-19 pandemic.
Materials and methods (Evidence Acquisition)
The methodology was designed before the revision of articles and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18]. The protocol was registered in the PROSPERO registry by the number (CRD42021248283).
Literature search methodology
PubMed and Cochrane’s databases were searched for English articles published from 1/1/2020 to 6/2/2021. The language was restricted to facilitate the revision of full articles. We used combined medical subject headings (MeSH) terms and keywords to build a search strategy. MeSH terms included; COVID-19, SARS-COV-2, COVID-19 post-intensive care syndrome, post-acute COVID-19 syndrome, erectile dysfunction, and penile erection. Keywords included erectile function, SARS, sexual dysfunction, and impotence. Reference lists were reviewed for related articles.
Study selection
Articles were reviewed independently by the authors (AB and AE). Disagreement was solved by discussion. The target articles were any full article of cross-sectional design, that investigated the status of EF during the pandemic, either quantitatively or qualitatively. The targeted population was adult males (>18 years old), regardless of marital status. Study groups included health care workers, COVID-19 survivors, and persons locked down due to the pandemic. Comparison groups have no or less exposure to these risks factors than the study groups. The outcome were assessed in terms of subjective ED complain and further IIEF-5 score [19].
Data extraction
Data were extracted by the two authors (AB and AE). Data has included: title, author, journal name, date of publishing, and the state of lockdown in the authors’ country at the time of data collection. Participant’s data has included sample size, average age, whether females are included in the study for other purposes, and the number of positive cases with diagnosis of COVID-19. Outcome data have included the rate of ED, an average IIEF-5 score, and the significance of the difference in study groups. Data of risk factors have included correlation with being a health care provider, marriage status, alcohol consumption, previous history of sexual dysfunction, and rate of sexually transmitted disease. Data about the frequency of sexual life and the significance of association were also gathered.
Data synthesis and analysis
This systematic review has investigated the change in EF during and after the COVID-19 pandemic (primary objective). The secondary objective was to screen the risk factors that were associated with changes in EF during the pandemic and its consequences. Due to the obvious heterogeneity among the inclusion criteria, study and control populations, methodologies, and measures of effect estimates, the synthesis of meta-analysis and forest plots were not applicable.
On the other hand, techniques of synthesis without metanalysis were implemented [20]. P-values of changes in ED status were combined using Fisher’s method [21]. Sensitivity analysis of p-values combination was done restricted by the type of measurement used to indicate ED status; IIEF-5 score versus percent of patients with ED. Prevalence of ED during the pandemic was reported using percentage. Median and range were used to summarize the distribution of prevalence data. We draw a bubble plot to visualize the relation between the prevalence of ED and sample size.
The approval of the Institution Review Board is not applicable in this review.
Results (Evidence synthesis)
Literature search
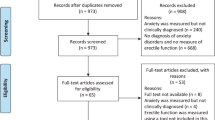
The systematic search of PubMed and Cochrane Reviews databases returned 20 records. Cochrane search returned 4 articles: 1 Cochrane review, and 3 reports from the ClinicalTrials.gov registry. There were no duplicates. Seventeen articles were excluded after revising the title and abstract. Excluded articles were reviews [17, 22], perspectives [23, 24], a letter [25], case reports [8, 14], studies about the treatment of COVID-19-related disease other than ED [26,27,28], articles considering female sexual dysfunction only [12, 13, 29], and all 4 records from Cochrane search. Three articles were included in the full qualitative synthesis process [6, 11, 16]. However, 2 articles [7, 15] had no eligible comparison groups, and they were included for the secondary objectives only (prevalence of ED, and investigation of risk factors). PRISMA diagram is shown in (Fig. 1).
Study characteristics
Table 1 shows the characteristics of the included studies. They included health care providers [6, 7], patients who have presented to the andrology clinic during the pandemic [11], and persons who have responded to online questionnaires during and after lockdown periods [15, 16].
Primary outcomes were sexual dysfunction [6, 11], decrease in EF and ejaculatory control [16], sexual satisfaction [15], and sexual attitude [7]. The study-design was non-randomized in all studies. Three studies had compared to male groups [6, 11, 16], one had compared to female group [15], and one study was non-comparative [7]. Except in one study [16], data were collected during the period of the local COVID-19 breakout, and most populations were locked down.
Participants attending the andrology clinic [3] were older than health care workers [6, 7] and social media users [16]. The control group was older than the study group in one study only [11].
Outcome measures
Change in EF
To measure the changes in EF, the IIEF-5 score was used in 2 studies [6, 16]. Change in percentage of patients with ED was used in one article [11] (Table 2).
In 2 studies, authors have compared EF status in participants during the COVID-19 pandemic with status before the pandemic [11, 16]. In the third [6], the authors have compared health care providers dealing with suspected and confirmed COVID-19 cases with patients attending the urology clinic during the pandemic.
All articles have reported a reduction in EF in association with exposure to the COVID-19 pandemic. There was significant reduction in mean IIEF-5 score (p < 0.001) [16], and significant increase in patients with ED after pandemic (p < 0.008) [11]. Health care providers had a higher rate of ED (p < 0.001), and lower median IIEF-5 scores than non-healthcare workers (p < 0.001) [6].
The heterogenicity among populations of the included studies prevented us from the quantitative synthesis of data. However, the p-values can be combined from two studies [20, 21]. For analytical purposes, we considered the reported p-values by Bulut et al., as if it has 2 investigations: the first for the change in median IIEF, and the second for the change in the rate of ED. The combined p-value for the 4 comparisons was (p < 0.00001, Chi2 = 56.6, degrees of freedom = 8). Considering sensitivity analysis, studies that reported changes in IIEF-5 [6, 16] have revealed no change in combined p-value (p < 0.00001, Chi2 = 26.2, degrees of freedom = 4). When considering studies that have reported changes in ED rates [6, 11], the combined p-value was (p < 0.00001, Chi2 = 30.4, degrees of freedom = 4).
There was strong evidence supported that EF status and scores were negatively affected by exposer to the COVID-19 pandemic. There was an increase in number of ED patients and a reduction in IIEF-5 scores during the pandemic in comparison to before the pandemic. The same results were reported among health care providers when compared to patients attending urology clinics.
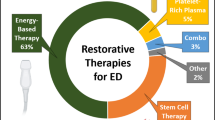
Assessment of ED
Most studies used a scoring system to assess ED. Three studies considered specific cut-off points of IIEF-5 scores <21 [6, 15], or IIEF score <25 [7]. Two studies defined ED as any decrease in the IIEF-5 score [16], or as a clinical-based diagnosis [11] (Fig. 2).
Accordingly, the rate of ED among populations who responded to online questionnaires was 32% [15, 16]. The rate of ED was higher among health care providers 40% [7] and 82% [6]. The highest rate (87%) was reported among older men attending andrology clinics during the pandemic [11].
Meta-analysis cannot be achieved due to clear differences among population characteristics. Data are summarized into a bubble plot (Fig. 3). The median value detected during the pandemic was 40%, and range from 32% to 87%.
Risk factors associated with EF changes
All studies have agreed that increased anxiety scores (Generalized Anxiety Disorder-7 (GAD-7) questionnaire, or State-Trait Anxiety Inventory-1 (STAI-I)) were associated with increased rates of ED [7]. Post-traumatic stress disorder (PTSD) score (Impact of Event Scale-Revised (IES-R)) was increased among health care providers and was associated with the increase in ED rates [6]. Increased depression score (Patient Health Questionnaire-9 (PHQ-9) was also associated with increased ED [15, 16], however, there was no association with Beck score [7]. Reduced frequency of sexual life and dissatisfaction was associated with more prevalence or severity of ED [15, 16] (Table 3).
The rate of ED was not affected by age, marital status, educational level, history of sexual dysfunction or intake of related drugs, smoking, chronic diseases, income level, occupational or economic changes. The association between increased ED rates and alcohol consumption was controversial. Being a health care provider or working in proximity to confirmed COVID-19 cases showed insignificant association with the increased rate of ED in 2 studies.
Frequency of sexual life
Reduction in frequency of sexual practice was associated with an increase in ED rate [16]. Changes in sexual life frequency after the pandemic was not universal. There was a significant reduction in the frequency of sexual practice per week among health care providers (1.32 (±1.27) during COVID-19 pandemic, vs 2.53 (±1.12) before pandemic; p < 0.001) [7], while the number per month was not changed among social media users (5.42 (±6.4) after pandemic vs 5.32 (±5.73) before pandemic; p = 0.713) [16].
Discussion
EF is always influenced by psychological as well as physiologic status and interaction of therapy for different concomitant conditions [30, 31]. Individuals who survived the COVID-19 pandemic were exposed to stressful events in terms of social, economic, and health issues. In the post-COVID-19 era, concerns were raised regarding possible long-term consequences. The pathogenesis of COVID-19 is not yet well understood, and investigation of the possible complications becomes mandatory.
Reviewing a rapidly evolving literature of COVID-19 offered few studies that investigated ED and sexual dysfunction among men. After more than one year of the initial spread of COVID-19, only 5 articles have addressed the rate of ED among survivors. On the other hand, patients attending clinics seeking advice about sexual health were increased, and diagnoses of sexual and other andrological diseases were also augmented during the pandemic [11].
There was an increase in rates of ED during and after the pandemic. There was also a significant reduction in IIEF-5 scores, which indicated an increase in the severity of ED. The significance of these changes was confirmed after combining p-values of the 3 studies that have investigated this issue (Table 2). In the current study, we have used sensitivity analysis to investigate the effect of heterogeneity among measures of effect estimates. We also combined p-values from studies that reported the change in the rate of ED and combined p-values from studies that reported the change in IIEF-5. Both tests agreed with our initial proposal.
The 5 studies have investigated the possible correlation between ED and psychological changes. Although psychological factors have played a critical role, biological and pathological factors cannot be excluded especially when the available data about the diagnosis of COVID-19 was limited. Furthermore, since infection can be asymptomatic in a significant number of patients, we cannot count psychological factors as the only underlying etiology of ED in the post-COVID-19 era.
The prevalence of ED during the pandemic ranged from 32% to 87%. Studies that have used social media to collect data have reported the lowest rate of ED [15, 16]. Those studies may have reflected the characteristics of social media users who may be younger in age. The study that have considered the older population during the pandemic have reported the highest prevalence [11]. The estimated prevalence of ED ranged from 40% to 82% in a special group of health care providers who were in close contact with COVID-19-positive patients.
The global prevalence of ED before the pandemic was variable. It was reported (3–76.5%) [32], (2–86%) [33], and (16.1%) [34], among patients with different ages. Studies from the Middle East area have reported the rate of ED to be 92.6% of patients visiting andrology clinics [35], 49.9% of adults older than 18 years [36], and 45.1% among internet users [37]. However, It was unfeasible to perform a precise comparison between absolute numbers among reports before and after the pandemic.
As expected, an increased ED rate is associated with decreased satisfaction during intercourse, and also with a reduced number of sexual practices. The fear of catching infection or infecting the partners play a role in amplifying the prevalence of anxiety and associated ED [6, 7]. Fears of transmitting an asymptomatic infection can contribute to increased anxiety and depression scores [7, 15, 16]. Furthermore, reduced physical contact during lockdown was associated with an increase in solitary sexual behaviors in the younger age group (18–32 yrs) [38]. Another study emphasized on the bidirectional relation between sexual activity and psychological status, and authors concluded that sexually active men who live with their partners during the pandemic have lower scores of GAD-7 and PHQ-9 [39]
No significant difference in age, marital status, education level, income level, chronic disease, and smoking rates between those who developed ED or showed a decrease in EF scores, and those who do not [6, 7, 16]. History of sexual dysfunction before the pandemic, either treated or not, was not associated with changes in ED rate after the pandemic [16]. Increased ED rates after the COVID-19 pandemic seem to be a special entity, not an exacerbation of a chronic condition.
There were controversial findings regarding the association of alcohol intake and increased ED [7, 16]. Although health care providers were facing higher levels of anxiety, an increase in ED among them was not reproducible [6, 16]. A recent study had addressed the considerations that should be put in mind during the assessment and treatment of ED patients. In that study, factors related to patient, partner, and physician judgment, all determine the course of ED and the response to the management plan. Among many important factors, patients and partner expectations, interrelation with the partner, satisfaction, and social factors are all affecting the EF status and the related therapeutic regimens [40].
The current study is limited by the availability of safe methods of interviewing patients during the pandemic. Authors in several studies relied upon social media to recruit cases, which might be biased toward special age groups. On the other hand, patients who had attended health care services during lockdown were not representing the general population, but a specific group of patients who were seeking urgent medical services. Further, Fisher’s method of combining p-values cannot address the magnitude of change. It assumes that the contribution of each study into the final p-value is equal to each other, and we could not estimate the weight of each sample size. Using median and range to summarize data about the prevalence of ED has not definitely addressed the effect of sample size in each study.
Conclusion
Exposure to the COVID-19 pandemic and its consequences was associated with increased anxiety, depression, PTSD, and sexual dissatisfaction. Both health care providers and the general population were affected but in variable degrees. Anxiety, depression, and PTSD were associated with an increase in ED cases and a reduction in EF score. This model emphasizes the effect of pandemic situation and similar disasters on the ability to maintain a normal sexual life.
References
WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. [cited 2021 Aug 4]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data [Internet]. [cited 2021 Aug 4]. Available from: https://covid19.who.int/.
Organization WH. Coronavirus disease 2019 (COVID-19): situation report, 73. World Health Organization;
Jin H, Wang H, Li X, Zheng W, Ye S, Zhang S, et al. Economic burden of COVID-19, China, January–March, 2020: a cost-of-illness study. Bull World Health Organ [Internet]. 2021;99:112. Feb 1 [cited 2021 Aug 4]Available from: /pmc/articles/PMC7856360/.
Mahendradhata Y, Andayani NLPE, Hasri ET, Arifi MD, Siahaan RGM, Solikha DA, et al. The Capacity of the Indonesian Healthcare System to Respond to COVID-19. Front public Heal [Internet]. 2021;9(July):649819. Available from: http://www.ncbi.nlm.nih.gov/pubmed/34307272%0A. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC8292619.
Bulut EC, Ertaş K, Bulut D, Koparal MY, Çetin S The effect of COVID-19 epidemic on the sexual function of healthcare professionals. Andrologia. 2021;(December 2020):1–8.
Culha MG, Demir O, Sahin O, Altunrende F. Sexual attitudes of healthcare professionals during the COVID-19 outbreak. Int J Impot Res [Internet]. 2021;33:102–9. https://doi.org/10.1038/s41443-020-00381-9. Available from.
Salama N, Blgozah S COVID-19 and Male Sexual Functioning: A report of 3 Recovered Cases and Literature Review. Clin Med Insights Case Reports [Internet]. 2021 [cited 2021 Aug 4];14. Available from: https://pubmed.ncbi.nlm.nih.gov/34104031/.
De Rose AF, Chierigo F, Ambrosini F, Mantica G, Borghesi M, Suardi N, et al. Sexuality during COVID lockdown: a cross-sectional Italian study among hospital workers and their relatives [Internet]. Int J Impot Res Int J Impot Res. 2021;33:131–6. https://pubmed.ncbi.nlm.nih.gov/33402720/.
Karagöz MA, Gül A, Borg C, Erihan İB, Uslu M, Ezer M, et al. Influence of COVID-19 pandemic on sexuality: a cross-sectional study among couples in Turkey. Int J Impot Res 2020 [Internet]. 2020 Dec 16 [cited 2021 Aug 4];1–9. Available from: https://www.nature.com/articles/s41443-020-00378-4.
Duran MB, Yildirim O, Kizilkan Y, Tosun C, Cirakoglu A, Gultekin MH, et al. Variations in the number of patients presenting with andrological problems during the coronavirus disease 2019 pandemic and the possible reasons for these variations: a multicenter study. Sex Med. 2021;9.
Kaya Y, Kaya C, Tahta T, Kartal T, Tokgöz VY. Examination of the effect of COVID-19 on sexual dysfunction in women. Int J Clin Pract. 2020;(November):1–5.
Fuchs A, Matonóg A, Pilarska J, Sieradzka P, Szul M, Czuba B, et al. The impact of COVID−19 on female sexual health. Int J Environ Res Public Health. 2020;17:1–9.
Shoar S, Khavandi S, Tabibzadeh E, Vaez A, Oskouei AK, Hosseini F, et al. A Late COVID-19 complication: male sexual dysfunction. Prehosp Disaster Med. 2020;35:688–9.
Omar SS, Dawood W, Eid N, Eldeeb D, Munir A, Arafat W. Psychological and sexual health during the COVID-19 pandemic in Egypt: are women suffering more? Sex Med. 2021;9:1–12.
Fang D, Peng J, Liao S, Tang Y, Cui W, Yuan Y, et al. An online questionnaire survey on the sexual life and sexual function of chinese adult men during the coronavirus disease 2019 epidemic. Sex Med. 2021;9.
Sansone A, Mollaioli D, Ciocca G, Limoncin E, Colonnello E, Vena W, et al. Addressing male sexual and reproductive health in the wake of COVID-19 outbreak. J Endocrinol Invest [Internet]. 2021;44:223–31. https://doi.org/10.1007/s40618-020-01350-1.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews [Internet]. Vol. 372, The BMJ. British Medical Journal Publishing Group; 2021 [cited 2021 Aug 4]. Available from: https://www.bmj.com/content/372/bmj.n71.
Rosen R, Cappelleri J, Smith M, Lipsky J, Peña B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. https://www.nature.com/articles/3900472.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:1–6.
Loughin TM. A systematic comparison of methods for combining p-values from independent tests. Comput Stat Data Anal. 2004;47:467–85.
He Y, Wang J, Ren J, Zhao Y, Chen J, Chen X. Effect of COVID-19 on male reproductive system – a systematic review. Front Endocrinol (Lausanne). 2021 May 27;12.
Žižek S The Appointment in Samarra: A New Use for Some Old Jokes. J Bioeth Inq. 2020;
Cocci A, Presicce F, Russo GI, Cacciamani G, Cimino S, Minervini A. How sexual medicine is facing the outbreak of COVID-19: experience of Italian urological community and future perspectives. Int J Impot Res [Internet]. 2020;32:480–2. https://doi.org/10.1038/s41443-020-0270-4.
Bertolo R, Cipriani C, Bove P. Anosmia and ageusia: a piece of the puzzle in the etiology of COVID-19-related transitory erectile dysfunction. J Endocrinol Invest. 2021;44:1123–4. May 1.
Feitosa MR, Parra RS, De Camargo HP, Da Costa Ferreira S, De Almeida Troncon LE, Da Rocha JJR, et al. COVID-19 quarantine measures are associated with negative social impacts and compromised follow-up care in patients with inflammatory bowel disease in Brazil. Ann Gastroenterol. 2021;34:39–45.
Salgotra R, Gandomi M, Gandomi AH. Time series analysis and forecast of the COVID-19 pandemic in India using Genetic Programming. Chaos, Solitons and Fractals. 2020 Sep 1;138.
Mazza M, Marano G, Lai C, Janiri L, Sani G Danger in danger: Interpersonal violence during COVID-19 quarantine. Psychiatry Res. 2020 Jul 1;289.
Saeaib N, Peeyananjarassri K, Liabsuetrakul T, Buhachat R, Myriokefalitaki E. Hormone replacement therapy after surgery for epithelial ovarian cancer. Cochrane Database Syst Rev. 2020 Jan 28;2020.
El-Sakka AI. Erectile dysfunction, depression, and ischemic heart disease: does the existence of one component of this triad necessitate inquiring the other two? (CME). J Sex Med. 2011;8:937–40. Apr 1.
El-Sakka AI, Shamloul R, Yassin AA Erectile dysfunction, cardiovascular diseases and depression: Interaction of therapy [Internet]. Vol. 10, Expert Opinion on Pharmacotherapy. Taylor & Francis; 2009 [cited 2021 Apr 11]. p. 2107–17. Available from: https://www.tandfonline.com/doi/abs/10.1517/14656560903089326.
Kessler A, Sollie S, Challacombe B, Briggs K, Van Hemelrijck M. The global prevalence of erectile dysfunction: a review. BJU Int [Internet]. 2019;124:587–99. www.bjui.org.
Prins J, Blanker MH, Bohnen AM, Thomas S, Bosch JLHR. Prevalence of erectile dysfunction: a systematic review of population-based studies. Int J Impot Res 2002 146 [Internet]. 2002 Dec 19 [cited 2021 Jun 7];14:422–32. Available from: https://www.nature.com/articles/3900905.
Nicolosi A, Glasser DB, Moreira ED, Villa M. Prevalence of erectile dysfunction and associated factors among men without concomitant diseases: a population study. Int J Impot Res [Internet] 2003;15:253–7. https://www.nature.com/articles/3901010.
El-Sakka AI. Erectile dysfunction in Arab countries. Part I: prevalence and correlates. Arab J Urol [Internet]. 2012;10:97–103. https://www.tandfonline.com/action/journalInformation?journalCode=taju20.
Ghalayini IF, Al-Ghazo MA, Al-Azab R, Bani-Hani I, Matani YS, Barham A-E, et al. Erectile dysfunction in a Mediterranean country: results of an epidemiological survey of a representative sample of men. Int J Impot Res. 2010;22:196–203. https://www.nature.com/articles/ijir200965.
Shaeer O, Shaeer K. The global online sexuality survey (GOSS): erectile dysfunction among Arabic-speaking internet users in the middle east. J Sex Med. 2011;8:2152–63. Aug 1.
Cascalheira CJ, McCormack M, Portch E, Wignall L. Changes in sexual fantasy and solitary sexual practice during social lockdown among young adults in the UK. Sex Med [Internet]. 2021;9:100342 https://doi.org/10.1016/j.esxm.2021.100342.
Mollaioli D, Sansone A, Ciocca G, Limoncin E, Colonnello E, Di Lorenzo G, et al. Benefits of sexual activity on psychological, relational, and sexual health during the COVID-19 breakout. J Sex Med [Internet]. 2021;18:35–49. https://doi.org/10.1016/j.jsxm.2020.10.008.
Bakr AM, El-Sakka AA, El-Sakka AI. Considerations for prescribing pharmacotherapy for the treatment of erectile dysfunction. Exp Opin Pharmacother. 2020;44:1–14.
Funding
This work has not received funding.
Author information
Authors and Affiliations
Contributions
AMB contributed to all parts of the manuscript; AIE contributed to all parts of the manuscript; All authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bakr, A.M., El-Sakka, A.I. Erectile dysfunction among patients and health care providers during COVID-19 pandemic: A systematic review. Int J Impot Res 34, 145–151 (2022). https://doi.org/10.1038/s41443-021-00504-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-021-00504-w
This article is cited by
-
Epidemiological and clinical characteristics of long COVID-19 among Iranians: A community-based study in southern Iran
BMC Public Health (2024)
-
Time-dependent analysis of erectile dysfunction in kidney transplant recipients: insights from four distinct time periods
BMC Infectious Diseases (2024)
-
A wearable adaptive penile rigidity monitoring system for assessment of erectile dysfunction
Microsystems & Nanoengineering (2024)
-
COVID‑19‑related postponement of elective sexual or reproductive health operations deteriorates private and sexual life: an ongoing nightmare study
International Journal of Impotence Research (2022)
-
Tip of the iceberg: erectile dysfunction and COVID-19
International Journal of Impotence Research (2022)