Abstract
Purpose
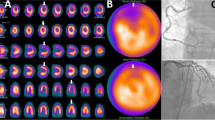
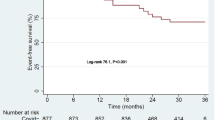
To assess myocardial injury using rest single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) in patients with COVID-19 and to evaluate whether myocardial injury detected by rest MPI predict the prognosis of symptoms after 6 months follow-up.
Methods
Patients suspected of myocarditis between December 2022 and March 2023, after the lifting of COVID-19 pandemic restrictions, and between December 2018 and March 2019, prior to the pandemic, were referred to our study. All patients underwent rest MPI. One hundred and sixty four patients with COVID-19 infection after the lifting of pandemic restrictions and 101 patients before the pandemic were included as the study and control groups, respectively. One hundred and fifty three patients of the study group and 83 of the control group presented symptoms when they initially visit to our department. Compare the parameters of myocardial injury detected by rest SPECT MPI between the two groups and then investigate the association between myocardial injury and symptom prognosis in symptomatic patients of both groups.
Results
Total perfusion defect (TPD) (4.2% ± 3.3% vs. 2.3% ± 2.2%, P < 0.001), summed rest score (SRS) (5.3 ± 5.4 vs. 2.7 ± 2.0, P < 0.001), the proportion of patients with TPD > 4% (43.3% vs. 17.8%, P < 0.001), TPD > 10% (6.71% vs 0, P < 0.001), SRS > 4 (40.2% vs 15.8%, P < 0.001), SRS > 10 (12.8% vs 0, P < 0.001), the number of abnormal perfusion segments (3.9 ± 3.1 vs. 2.4 ± 1.7, P < 0.001) were all significantly higher in the study group. All the parameters of rest MPI were not associated with the prognosis of symptoms in symptomatic patients of both groups after 6 months follow-up.
Conclusion
Myocardial injury in COVID-19 patients could be assessed by rest SPECT MPI. The COVID-19 patients could exhibited a higher frequency and greater severity of myocardial injury than uninfected control patients. Myocardial injury assessed by rest MPI did not predict for the prognosis of symptoms in symptomatic patients of both COVID-19 patients and uninfected patients.




Similar content being viewed by others
Availability of data and material
The data and material that support the findings of this study are available on request from the corresponding authors.
References
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–4. https://doi.org/10.1016/s1473-3099(20)30120-1.
Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281-92.e6. https://doi.org/10.1016/j.cell.2020.02.058.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8. https://doi.org/10.1016/s0140-6736(20)30937-5.
Azevedo RB, Botelho BG, Hollanda JVG, Ferreira LVL, Junqueira de Andrade LZ, Oei S, et al. Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens. 2021;35:4–11. https://doi.org/10.1038/s41371-020-0387-4.
Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, et al. Recognition and Initial Management of Fulminant Myocarditis: a scientific statement from the American Heart Association. Circulation. 2020;141:e69–92. https://doi.org/10.1161/cir.0000000000000745.
Araz M, Soydal Ç, Sütçü G, Demir B, Özkan E. Myocardial perfusion SPECT findings in postCOVID period. Eur J Nucl Med Mol Imaging. 2022;49:889–94. https://doi.org/10.1007/s00259-021-05552-4.
Assante R, D’Antonio A, Mannarino T, Gaudieri V, Zampella E, Mainolfi CG, et al. Impact of COVID-19 infection on short-term outcome in patients referred to stress myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2022;49:1544–52. https://doi.org/10.1007/s00259-021-05619-2.
Çap M, Bilge Ö, Gündoğan C, Tatlı İ, Öztürk C, Taştan E, et al. SPECT myocardial perfusion imaging identifies myocardial ischemia in patients with a history of COVID-19 without coronary artery disease. Int J Cardiovasc Imaging. 2022;38:447–56. https://doi.org/10.1007/s10554-021-02477-9.
Perlis RH, Santillana M, Ognyanova K, Safarpour A, Lunz Trujillo K, Simonson MD, et al. Prevalence and Correlates of Long COVID Symptoms Among US Adults. JAMA Netw Open. 2022;5: e2238804. https://doi.org/10.1001/jamanetworkopen.2022.38804.
Laissy JP, Hyafil F, Feldman LJ, Juliard JM, Schouman-Claeys E, Steg PG, Faraggi M. Differentiating acute myocardial infarction from myocarditis: diagnostic value of early- and delayed-perfusion cardiac MR imaging. Radiology. 2005;237:75–82. https://doi.org/10.1148/radiol.2371041322.
Liu B, Li M, Zhou Z, Guan X, Xiang Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J Autoimmun. 2020;111: 102452. https://doi.org/10.1016/j.jaut.2020.102452.
de la Rica R, Borges M, Gonzalez-Freire M. COVID-19: In the Eye of the Cytokine Storm. Front Immunol. 2020;11: 558898. https://doi.org/10.3389/fimmu.2020.558898.
Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319–29. https://doi.org/10.1038/s41577-021-00536-9.
Chen C, Zhou Y, Wang DW. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz. 2020;45:230–2. https://doi.org/10.1007/s00059-020-04909-z.
Amraei R, Rahimi N. COVID-19, Renin-Angiotensin System and Endothelial Dysfunction. Cells. 2020;9. https://doi.org/10.3390/cells9071652.
Yin J, Wang S, Liu Y, Chen J, Li D, Xu T. Coronary microvascular dysfunction pathophysiology in COVID-19. Microcirculation. 2021;28: e12718. https://doi.org/10.1111/micc.12718.
Becker RC. COVID-19 update: Covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020;50:54–67. https://doi.org/10.1007/s11239-020-02134-3.
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021;372: n693. https://doi.org/10.1136/bmj.n693.
Saririan M, Armstrong R, George JC, Olechowski B, O'Connor S, Byrd JB, Chapman AR. ST-segment elevation in patients presenting with COVID-19: case series. Eur Heart J Case Rep. 2021;5:ytaa553. https://doi.org/10.1093/ehjcr/ytaa553.
Arnold JR, McCann GP. Cardiovascular magnetic resonance: applications and practical considerations for the general cardiologist. Heart. 2020;106:174–81. https://doi.org/10.1136/heartjnl-2019-314856.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265–73. https://doi.org/10.1001/jamacardio.2020.3557.
Wang H, Li R, Zhou Z, Jiang H, Yan Z, Tao X, et al. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2021;23:14. https://doi.org/10.1186/s12968-021-00710-x.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40. https://doi.org/10.1007/s00259-015-3139-x.
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28:583–90. https://doi.org/10.1038/s41591-022-01689-3.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–15. https://doi.org/10.1038/s41591-021-01283-z.
Jurgens CY, Lee CS, Aycock DM, Masterson Creber R, Denfeld QE, DeVon HA, et al. State of the Science: The Relevance of Symptoms in Cardiovascular Disease and Research: A Scientific Statement From the American Heart Association. Circulation. 2022;146:e173–84. https://doi.org/10.1161/cir.0000000000001089.
Huang S, Vignon P, Mekontso-Dessap A, Tran S, Prat G, Chew M, et al. Echocardiography findings in COVID-19 patients admitted to intensive care units: a multi-national observational study (the ECHO-COVID study). Intensive Care Med. 2022;48:667–78. https://doi.org/10.1007/s00134-022-06685-2.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of the First Affiliated Hospital of the Air Force Medical University. The committee’s reference number was KY20232047-X-1. All procedures performed in this study were performed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethics standards. Informed consent to participate was obtained from all patients included in the study.
Consent for publication
Written informed consent for publication was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xin, K., Ma, X., Meng, X. et al. Assessment of myocardial injury by SPECT myocardial perfusion imaging in patients with COVID-19 infection in a single center after lifting the restrictions in China. Ann Nucl Med 38, 971–979 (2024). https://doi.org/10.1007/s12149-024-01970-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-024-01970-0