Abstract
Background
Limited research has studied the influence of social determinants of health (SDoH) on the receipt, disease risk, and subsequent effectiveness of neutralizing monoclonal antibodies (nMAbs) for outpatient treatment of COVID-19.
Objective
To examine the influence of SDoH variables on receiving nMAb treatments and the risk of a poor COVID-19 outcome, as well as nMAb treatment effectiveness across SDoH subgroups.
Design
Retrospective observational study utilizing electronic health record data from four health systems. SDoH variables analyzed included race, ethnicity, insurance, marital status, Area Deprivation Index, and population density.
Participants
COVID-19 patients who met at least one emergency use authorization criterion for nMAb treatment.
Main Measure
We used binary logistic regression to examine the influence of SDoH variables on receiving nMAb treatments and risk of a poor outcome from COVID-19 and marginal structural models to study treatment effectiveness.
Results
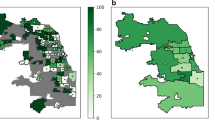
The study population included 25,241 (15.1%) nMAb-treated and 141,942 (84.9%) non-treated patients. Black or African American patients were less likely to receive treatment than white non-Hispanic patients (adjusted odds ratio (OR) = 0.86; 95% CI = 0.82–0.91). Patients who were on Medicaid, divorced or widowed, living in rural areas, or living in areas with the highest Area Deprivation Index (most vulnerable) had lower odds of receiving nMAb treatment, but a higher risk of a poor outcome. For example, compared to patients on private insurance, Medicaid patients had 0.89 (95% CI = 0.84–0.93) times the odds of receiving nMAb treatment, but 1.18 (95% CI = 1.13–1.24) times the odds of a poor COVID-19 outcome. Age, comorbidities, and COVID-19 vaccination status had a stronger influence on risk of a poor outcome than SDoH variables. nMAb treatment benefited all SDoH subgroups with lower rates of 14-day hospitalization and 30-day mortality.
Conclusion
Disparities existed in receiving nMAbs within SDoH subgroups despite the benefit of treatment across subgroups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Over the course of the coronavirus disease 2019 (COVID-19) pandemic, historically disadvantaged groups have experienced disproportionate risks of COVID-19 infection, hospitalization, and death.1 Due to these observations, there has been a heightened interest in understanding the social determinants, defined by the World Health Organization as “the conditions in which people are born, grow, work, live and age and their access to power, money and resources,” that influence uptake and effectiveness of COVID-19 treatments.1, 2
Neutralizing monoclonal antibodies (nMAbs) targeting the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) became available in November 2020 for the early treatment of mild to moderate illness in non-hospitalized patients.3,4,5 The federal government and health systems developed guidance to ensure equitable distribution of nMAbs to historically underserved and disadvantaged populations.6,7,8
Despite this guidance, evidence exists that acceptance and receipt of nMAb treatment are lower in historically disadvantaged populations.9,10,11,12 In one health system, Bierle et al. (2021) reported that acceptance of nMAb treatment was higher in patients who were non-Hispanic white, spoke English, and had a spouse or life partner.9 In a recent consortium study, Boehmer et al. (2022) found that black and Hispanic patients were 23.3% and 51.3% less likely to receive outpatient nMAb treatment than white and non-Hispanic patients, respectively.10 In a single-center study reported by Wu et al. nMAb delivery rates were lower in geographic areas with higher social vulnerability in the greater Chicago, Illinois area.12 However, the previous studies have been limited in sample sizes, patient-level data availability, and geographic scope. In addition, to our knowledge, no study has explored the relationship between disparities in receiving nMAb and severe COVID-19 outcomes.2
In this study, we used electronic health record (EHR) data from four health systems to abstract social determinants of health (SDoH) variables on the individual and geographic level, including race, ethnicity, insurance, marital status, Area Deprivation Index (ADI, higher scores indicating more vulnerable), and population density. We examined (1) the influence of SDoH variables on whether a patient received outpatient nMAb treatment; (2) the influence of SDoH variables on a COVID-19 disease risk score (DRS); and (3) whether nMAb treatment effectiveness differed across SDoH groups.
METHODS
Study Population
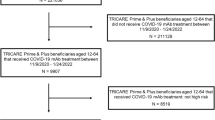
The Houston Methodist, Intermountain, Mayo Clinic, and University of California-Irvine health systems provided de-identified EHR data to a centralized registry for COVID-19 positive patients. Patients were included in the registry if they were 12 years of age or older, were eligible for nMAb treatment, and had a laboratory-confirmed positive COVID-19 polymerase chain reaction or antigen test collected in the non-inpatient setting between November 2020 and January 2022. Patients were considered eligible for nMAb treatment if they had at least one of the conditions or factors listed in the Emergency Use Authorization (EUA).3,4,5, 13
During our study period, patients could receive the following nMAb treatments: bamlanivimab, bamlanivimab-etesevimab, casirivimab-imdevimab, or sotrovimab. Patient index date was the date of a positive COVID-19 test result or date of treatment referral. Patients were excluded from the study population if they had received a different COVID-19 therapeutic (e.g., molnupiravir, nirmatrelvir/ritonavir) in a non-hospitalized setting within the outcome window of 30 days.
SDoH and Clinical Variables
SDoH variables were collected through routine care and included birth sex, race, ethnicity, health insurance, marital status, and the geographic location of primary residence. Race and ethnicity variables were collapsed to include a white non-Hispanic group and a white Hispanic group. Non-white races who self-identified as either Hispanic or non-Hispanic were labelled according to their race group. To comply with Safe Harbor guidelines, health systems provided only the 3-digit ZIP code of each patient’s primary residence, which were then mapped to the ADI and population density estimates from the American Community Survey.14,15,16 ADI scores for 5-digit ZIP codes were weighted by population densities to produce estimates of ADI scores for 3-digit ZIP codes. Population densities from the 2019 American Community Survey for 5-digit ZIP codes were weighted by the geographic areas to produce estimates by 3-digit ZIP code. COVID-19 vaccination status was obtained from vaccine registries and integrated into the EHR workflow. Patients were considered partially vaccinated if they received one Moderna or Pfizer vaccine and fully vaccinated if they received one Janssen vaccine or two Moderna/Pfizer vaccines. Patients were considered boosted if they had one additional vaccine after being “fully vaccinated.” Comorbid conditions in the two years prior to the index date were grouped according to Elixhauser and internally developed comorbidity groupings to provide variables of comorbidity status.17 Healthcare utilization included the number of total healthcare visits in the two years prior to the index date. Results by health system are not presented in accordance with the data use agreements.
Propensity Score Model
The propensity score (PS) in this study is the probability a patient received nMAbs conditional on a set of covariates and served two purposes. The first purpose was to use the coefficients of the PS model to understand the influence of SDoH and clinical variables on the probability a patient received nMAbs. The second purpose was to use the PS to adjust for potential confounding via inverse probability of treatment weighting in our effectiveness models. Of note, our dataset does not provide information on whether a patient was offered or declined nMAb treatment.
To build the PS model, continuous variables were categorized to enable a direct comparison to binary variable coefficients. Age was categorized into 10-year bands (e.g., 20 to 29, 30 to 39), total number of healthcare visits and ADI were grouped by quintiles, and population density was grouped by quartiles. Quartiles for population density were necessary due to a large percent of the patients living in a single 3-digit ZIP code. A full list of the variables used in the PS model is described in Table S1. Logistic and decision tree PS models were built using a hyperparameter grid search and assessed for covariate balance.18 The selected PS model was a logistic regression with L1 regularization, an inverse regularization strength of 0.1, and balanced class weights, and used the stochastic average gradient acceleration (SAGA) solver. The selected PS model achieved adequate covariate balance, with all absolute standardized mean differences < 0.1.19
Disease Risk Score Model
A patient’s DRS is the risk of a poor outcome, defined as either a hospitalization or death within 30 days of a patient’s index date. The DRS model used data only from non-treated patients to prevent the influence of treatment on the DRS outcome. The DRS model was an L2 logistic regression with an inverse regularization strength of 10 and balanced class weights and used the SAGA solver. Logistic regression and decision tree models were evaluated for use in the DRS model. The highest-ranking logistic regression model was used for this study because it was less likely to overtrain the model than the tree-based methods, it was well-calibrated, and the results and coefficients are easily interpretable. The influence of SDoH variables on the DRS was assessed via the coefficients of the DRS model. The DRS model included all the variables used in the PS model.
Treatment Effectiveness
Effectiveness outcomes included (1) hospitalizations within 14 days and (2) mortality within 30 days of a patient’s index date. Hospitalizations on the index date or treatment date were not considered as outcomes. Marginal structural models (MSM) were used to study nMAb effectiveness within SDoH subgroups. To increase statistical power in the effectiveness models, patients who identified as American Indians, Alaska Natives, Native Hawaiians, and Pacific Islanders, and those self-identifying as other were collapsed into the “other” race category. To account for the missing data, which was missing at < 3% for all variables, predictive mean matching was used to generate ten imputed datasets.20 Stabilized weights derived from the propensity scores within each imputation group were used in logistic regression MSMs and effect estimates were pooled using Rubin’s Rules.21
RESULTS
Study Population Description
The study population included 167,183 patients, of which 25,241 (15.1%) received nMAb treatment. In unadjusted analyses, nMAb-treated patients were more likely to be older than the non-treated patients (Table 1). Women outnumbered men in both treatment groups, but men had a higher proportion treated (16.6%) than women (14.0%). The race and ethnicity group with the highest proportion of treated patients was white non-Hispanic at 16.7%. Treatment rates for the remaining racial subgroups were lower, ranging from 10.1% for white Hispanic patients to 13.3% for American Indian or Alaska Native patients. In terms of insurance, the nMAb treatment rate was highest for patients with Medicare (30.6%), but lowest in patients who self-paid or had no insurance (7.3%).
Factors Associated with Receiving Treatment
The adjusted odds ratios (OR) from the PS models indicate subgroups with lower or higher odds of being treated with nMAb, after adjusting for additional covariates (Fig. 1 and Table S1). In regard to the SDoH variables, females were less likely to be treated than males (OR = 0.89; 95% CI = 0.87 – 0.91). Compared to white non-Hispanic patients, black or African American patients were less likely to be treated (OR = 0.86; 95% CI = 0.82 – 0.91), whereas white Hispanic, Native Hawaiian or Other Pacific Islander, and American Indian or Alaska Native were more likely to be treated with nMAbs. Compared to patients with private insurance, Medicaid patients and patients who self-paid or had no insurance were less likely to be treated with nMAbs. For example, Medicaid patients had 0.89 (95% CI = 0.84 – 0.93) times the odds of nMAb treatment compared to patients with private insurance. Compared with married patients, patients who were divorced, unmarried, or widowed all had lower odds of receiving nMAb treatment. We observed a non-linear relationship between our ADI categories and propensity to treat. Compared to patients living in low ADI areas (ADI < 30), those in mid-range zones (ADI 40–45, 46–56) were more likely to receive nMAbs. Those with the highest deprivation (ADI 57 +) were less likely to receive nMAb treatment. We observed that patients in more dense geographic locations were more likely to be treated.
In general, the most influential factors associated with receiving treatment were age, comorbidities related to immunosuppression, and index date year and month. As a patient’s age increased, their odds of nMAb treatment increased. For example, patients 80 + years old had 7.11 (95% CI = 6.37 – 7.94) times the odds of being treated compared to patients 12 to < 20 years old. The most influential comorbidity on propensity to treat was if a patient had a diagnosis related to solid organ or blood stem cell transplantation in the year prior to the index date (OR = 3.36; 95% CI = 2.78 – 4.06). Patients diagnosed in September or October 2021 had 15.39 (95% CI = 14.27–16.60) and 16.28 (95% CI = 15.04 – 17.62) times the odds of nMAb treatment, respectively, compared to patients diagnosed in November 2020, which was the first month nMAbs received EUA.
Factors Associated with Disease Risk Score
The adjusted ORs from the DRS model indicate subgroups with lower or higher odds of a poor outcome, defined as hospitalization or death within 30 days of the index date, after adjusting for additional covariates and assuming no treatment (Fig. 2 and Table S2). Females were less likely than males to have a poor outcome (OR = 0.77; 95% CI = 0.75 – 0.79). Compared to white non-Hispanics, all other race groups except black or African American had increased risk of a poor outcome. Asian and Native Hawaiian or Other Pacific Islander patients had 1.62 (95% CIs = 1.50 – 1.75 and 1.45 – 1.82, respectively) times the odds of a poor outcome compared to white non-Hispanic patients. Black or African American patients had similar odds of a poor outcome as white non-Hispanic patients (OR = 0.99; 95% CI = 0.94 – 1.05). Compared to patients with private insurance, Medicare and Medicaid patients had increased risk of a poor outcome, whereas patients who self-paid or had no insurance were less likely to experience a poor outcome (OR = 0.72; 95% CI = 0.69 – 0.76). Compared to married patients, unmarried patients were less likely to experience a poor outcome, whereas divorced and widowed were more likely to experience a poor outcome. Patients living in geographical locations with less population density and higher ADIs were also more likely to experience a poor outcome.
Similar to the PS model results, the most important factors that predicted a poor outcome were clinical variables that included age, comorbidities, index date year and month, COVID-19 vaccination status, and pregnancy status. Patients with cystic fibrosis and severe renal failure had 3.47 (95% CI = 1.54 – 7.80) and 3.38 (95% CI = 2.81 – 4.08) times the odds of a poor outcome, respectively. We saw decreased odds of a poor outcome in patients who were fully vaccinated and fully vaccinated with a booster. Pregnant patients were more likely to experience a poor outcome (OR = 17.69; 95% CI = 16.33 – 19.16) since hospitalization became common practice for moderately ill COVID-19 positive pregnant patients.
Comparing Factors Influencing Receipt of Treatment and Disease Risk Score
We found important differences when we compared the influence of patient factors on receiving nMAb treatment with the influence of patient factors on risk of a poor outcome (Figure S1). Although black or African Americans had approximately the same risk of a poor outcome as white non-Hispanic patients, they were less likely to receive nMAb treatment. Medicaid and divorced or widowed patients were more likely to experience a poor outcome, but less likely to receive nMAb treatment. Similarly, patients in geographical locations with the highest ADI (most vulnerable) and that were more rural were more likely to experience a poor outcome, but less likely to receive treatment. The comorbidities most related to a poor outcome (cystic fibrosis and severe renal failure) were not significantly associated with receiving nMAb treatment.
Treatment Effectiveness Within Subgroups
We evaluated nMAb treatment effectiveness based on SDoH variables and found nMAb treatment significantly reduced the odds of 14-day hospitalizations and 30-day mortality across most of the subgroups (Table 2). In both males and females, nMAb treatment was effective at reducing 14-day hospitalizations and 30-day mortality. The direction of associations was consistent across all race and ethnicity groups when comparing nMAb treatment effect on 14-day hospitalizations; however, nMAb treatment was only significantly associated with reducing odds of 14-day hospitalizations in the white non-Hispanic, black or African American, and “other” race patients. All racial groups had reduced odds of 30-day mortality if treated with nMAbs, although white non-Hispanic, white Hispanic, and other racial groups had significant reductions. nMAb treatment significantly reduced 14-day hospitalizations and 30-day mortality in patients with private insurance or who were covered by Medicare. We found nMAb treatment was effective at reducing the odds of 14-day hospitalization and 30-day mortality independent of marital status, ADI, and population density.
DISCUSSION
During the COVID-19 pandemic, the federal government provided nMAbs free of charge. The health systems in our consortium created deliberate outreach plans to make treatment available through outpatient clinics, infusion centers, emergency rooms, and mobile vans.8, 22, 23 Furthermore, each health system was a regional center for nMAb treatment, accepting patients from neighboring health systems and actively seeking patients who may not have had frequent contact with traditional primary care services.
Despite this outreach effort, we observed disparities in the receipt of nMAb treatment based upon SDoH variables. Our findings that black or African American patients were less likely to be treated with nMAbs are similar to findings previously reported.9,10,11 In addition to studies exploring receipt of nMAbs, research has shown that people of color received other COVID-19 treatments including ritonavir-booster nirmatrelvir (Paxlovid) and remdesivir less often than other populations.10, 11, 24 In our study, we cannot determine the reasons for the disparity in nMAb treatment among our SDoH groups as our dataset does not provide information on whether a patient was offered or declined nMAb treatment. Bierle et al. (2021) found that the acceptance rate of nMAb treatment for black or African American patients was 47.5% versus a 60.0% acceptance rate in white patients.9 However, Wu et al. (2022) did not report a significant difference in patient refusal of nMAb treatment by racial composition.12 Other reasons for disparities in receiving treatment may be due to reduced access to COVID-19 treatment facilities,25 language barriers,12 health system mistrust and treatment hesitancy,26 and implicit or explicit bias by healthcare providers.27
Risk factors for poor COVID-19 outcomes are a well-studied research area.28,29,30,31,32 While we reported variables associated with a poor outcome, our study is unique in comparing the influence of patient characteristics on both propensity to treat and risk of disease progression. We found multiple instances where a SDoH variable was associated with decreased odds of treatment, but increased odds of a poor outcome. Specifically, patients who were on Medicaid, divorced or widowed, living in a rural area, or living in areas with the highest ADI (most vulnerable) had lower odds of receiving nMAb treatment, but higher odds of a poor outcome. The intersection of these factors provides us with a roadmap to identify those populations most in need of better access and outreach.
In general, nMAb treatment effectiveness did not vary by SDoH factor and most groups experienced significantly lower 14-day hospitalization and/or 30-day mortality rates. When treatment effectiveness differences were observed, one of the comparison groups typically was a smaller subset of the total population and the differences were not robust across both outcomes studied. Similar nMAb treatment effectiveness across SDoH subgroups is consistent with our a priori hypothesis. We had no reason to believe the nMAb binding affinity to the spike protein receptor-binding domain of SARS-CoV-2 would vary by SDoH subgroups, given that, except for birth sex, our SDoH variables are social constructs that reflect culture, history, and socioeconomics.
To our knowledge, this is the largest study to investigate factors related to outpatient COVID-19 treatment with patient-level data. However, several limitations of our study are important to recognize. As discussed previously, our study did not know which patients were offered treatment and which patients declined treatment. To meet Safe Harbor requirements, this study only collected deidentified data, which necessitated using 3-digit ZIP codes to represent a patient’s primary residence. Our ADI and population density metrics would have provided more valuable information if we could have mapped 5-digit ZIP codes to those factors, as the 3-digit ZIP codes contained, on average, 43.5 5-digit ZIP codes with a standard deviation of the ADI of 15.9. We did not have access to some important SDoH variables including primary language spoken at home, household income, and patient education.1 Finally, the nMAbs studied in this research are no longer in use. However, many of our results correspond with other study findings that investigated utilization of current COVID-19 treatments including ritonavir-boosted nirmatrelvir and we believe our novel findings can be applied to future treatment outreach efforts.
Previous strategies proposed to expand COVID-19 vaccine coverage in communities of color may provide a blueprint to improve outpatient treatment uptake.33, 34 Chhibber et al. (2022) provide comprehensive guidance for innovative delivery of care for vulnerable populations through partnerships with churches, extended-hours clinics, community health worker outreach, and other measures.34 In addition, training healthcare providers to use specific language when discussing potential outpatient COVID-19 treatments may help address COVID-19 mistrust and increase uptake.35 Community-engaged research including topics on the dissemination and implementation of treatments for COVID-19 can help address care for historically disadvantaged groups and for those with greatest need.
References
World Health Organization. COVID-19 and the social determinants of health and health equity: evidence brief [Internet]. Geneva: World Health Organization; 2021 [cited 2022 Nov 7]. Available from: https://apps.who.int/iris/handle/10665/348333.
Centers for Disease Control and Prevention. Outpatient Use of COVID-19 Medication [Internet]. 2022 [cited 2022 Nov 22];Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/data-review/evidence.html.
FDA. FDA Fact Sheet for Health Care Providers Emergency Use Authorization (EUA) of Sotrovimab. [Internet]. 2022 [cited 2022 Apr 11];Available from: https://www.fda.gov/media/149534/download.
FDA. FDA Fact Sheet for Health Care Providers Emergency Use Authorization (EUA) of REGEN-COV® (casirivimab and imdevimab) [Internet]. 2021 [cited 2022 Apr 11];Available from: https://www.fda.gov/media/145611/download.
FDA. FDA Fact Sheet for Health Care Providers Emergency Use Authorization (EUA) of bamlanivimab and etesevimab. 2022 [cited 2022 Apr 11];Available from: https://www.fda.gov/media/145802/download.
Administration of Strategic Preparedness & Response. State/Territory-Coordinated Distribution of COVID-19 Therapeutics [Internet]. 2022 [cited 2022 Nov 1];Available from: https://aspr.hhs.gov/COVID-19/Therapeutics/Distribution/Pages/default.aspx.
CDC. Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals [Internet]. Cent. Dis. Control Prev. 2020 [cited 2022 Jun 13];Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html.
Sakata T, Brunisholz KD, Andersen C, Davie D, Srivastava R, Webb BJ. The MAb Squad: Delivering Covid-19 Monoclonal Antibody Therapy Across a Large Geographic Region. NEJM Catal [Internet] 2021 [cited 2022 Sep 9];2(9):CAT.21.0154. Available from: http://catalyst.nejm.org/doi/https://doi.org/10.1056/CAT.21.0154.
Bierle DM, Ganesh R, Wilker CG, et al. Influence of Social and Cultural Factors on the Decision to Consent for Monoclonal Antibody Treatment among High-Risk Patients with Mild-Moderate COVID-19. J Prim Care Community Health [Internet] 2021 [cited 2021 Oct 19];12:21501327211019280. Available from: https://pubmed.ncbi.nlm.nih.gov/34032171/.
Boehmer TK, Koumans EH, Skillen EL, et al. Racial and Ethnic Disparities in Outpatient Treatment of COVID-19 – United States, January–July 2022. MMWR Morb Mortal Wkly Rep [Internet] 2022 [cited 2022 Oct 28];71(43):1359–65. Available from: http://www.cdc.gov/mmwr/volumes/71/wr/mm7143a2.htm?s_cid=mm7143a2_w.
Wiltz JL, Feehan AK, Molinari NM, et al. Racial and Ethnic Disparities in Receipt of Medications for Treatment of COVID-19 — United States, March 2020–August 2021. MMWR Morb Mortal Wkly Rep [Internet] 2022 [cited 2022 Nov 1];71(3):96–102. Available from: http://www.cdc.gov/mmwr/volumes/71/wr/mm7103e1.htm?s_cid=mm7103e1_w.
Wu E-L, Kumar RN, Moore WJ, et al. Disparities in COVID-19 Monoclonal Antibody Delivery: a Retrospective Cohort Study. J Gen Intern Med [Internet] 2022 [cited 2022 Nov 1];37(10):2505–13. Available from: https://link.springer.com/https://doi.org/10.1007/s11606-022-07603-4.
National Institute of Health. Anti-SARS-CoV-2 Monoclonal Antibodies [Internet]. COVID-19 Treat. Guidel. 2022 [cited 2022 Mar 7];Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/anti-sars-cov-2-monoclonal-antibodies/.
United States Census Bureau. 2019 American Community Survey. [cited 2022 Feb 18];Available from: https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/.
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible — The Neighborhood Atlas. N Engl J Med [Internet] 2018 [cited 2022 Mar 4];378(26):2456–8. Available from: https://doi.org/10.1056/NEJMp1802313.
University of Wisconsin School of Medicine and Public Health. 2019. Area Deprivation Index, Version 3.1 [Internet]. [cited 2022 Feb 28];Available from: https://www.neighborhoodatlas.medicine.wisc.edu.
AHRQ. Elixhauser Comorbidity Software Refined for ICD-10-CM diagnosis, v2022.1. 2021;Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/CMR-User-Guide-v2022-1.pdf. Accessed 2022 Dec 2
Belitser SV, Martens EP, Pestman WR, Groenwold RHH, de Boer A, Klungel OH. Measuring balance and model selection in propensity score methods. Pharmacoepidemiol Drug Saf [Internet] 2011 [cited 2021 Nov 9];20(11):1115–29. Available from: https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1002/pds.2188.
Stuart EA, Lee BK, Leacy FP. Prognostic score–based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol [Internet] 2013 [cited 2022 Mar 11];66(8):S84-S90.e1. Available from: https://www.jclinepi.com/article/S0895-4356(13)00162-5/fulltext.
van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw [Internet] 2011 [cited 2021 Dec 10];45(3):1–67. Available from: https://www.jstatsoft.org/index.php/jss/article/view/v045i03.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons; 1987. [cited 2022 Nov 15].
R B, G L, H T, BrownewellVicki. Rapid Operationalization of Covid-19 Monoclonal Antibody Infusion Clinics. NEJM Catal Innov Care Deliv [Internet]. 2021 Mar 29 [cited 2022 Oct 5]; Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0040.
Razonable RR, Aloia NCE, Anderson RJ, et al. A Framework for Outpatient Infusion of Antispike Monoclonal Antibodies to High-Risk Patients with Mild-to-Moderate Coronavirus Disease-19. Mayo Clin Proc [Internet] 2021 [cited 2022 Nov 7];96(5):1250–61. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0025619621001919.
Castro AD, Mayr FB, Talisa VB, et al. Variation in Clinical Treatment and Outcomes by Race Among US Veterans Hospitalized With COVID-19. JAMA Netw Open. 2022 Oct 3;5(10):e2238507. [cited 2022 Dec 15].
Hill L, Artiga S, Rouw A, Kates J. How Equitable is Access to COVID-19 Treatments? [Internet]. 2022 [cited 2022 Nov 28];Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/how-equitable-is-access-to-covid-19-treatments/.
Bogart LM, Ojikutu BO, Tyagi K, et al. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. JAIDS J Acquir Immune Defic Syndr [Internet] 2021 [cited 2022 Nov 28];86(2):200–7. Available from: https://journals.lww.com/https://doi.org/10.1097/QAI.0000000000002570.
Williams DR, Wyatt R. Racial Bias in Health Care and Health: Challenges and Opportunities. JAMA [Internet] 2015 [cited 2022 Nov 28];314(6):555. Available from: http://jama.jamanetwork.com/article.aspx?doi=https://doi.org/10.1001/jama.2015.9260.
Jehi L, Ji X, Milinovich A, et al. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLOS ONE [Internet] 2020 [cited 2022 Mar 2];15(8):e0237419. Available from: https://dx.plos.org/https://doi.org/10.1371/journal.pone.0237419.
Bennett TD, Moffitt RA, Hajagos JG, et al. Clinical Characterization and Prediction of Clinical Severity of SARS-CoV-2 Infection Among US Adults Using Data From the US National COVID Cohort Collaborative. JAMA Netw Open 2021;4(7):e2116901.
Razonable RR, Ganesh R, Bierle DM. Clinical Prioritization of Antispike Monoclonal Antibody Treatment of Mild to Moderate COVID-19. Mayo Clin Proc [Internet] 2022 [cited 2022 Nov 7];97(1):26–30. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0025619621008685.
Webb BJ, Levin NM, Grisel N, et al. Simple scoring tool to estimate risk of hospitalization and mortality in ambulatory and emergency department patients with COVID-19. PLOS ONE [Internet] 2022 [cited 2022 Nov 7];17(3):e0261508. Available from: https://dx.plos.org/https://doi.org/10.1371/journal.pone.0261508.
Chow DS, Glavis-Bloom J, Soun JE, et al. Development and external validation of a prognostic tool for COVID-19 critical disease. PLOS ONE [Internet] 2020 [cited 2022 Nov 7];15(12):e0242953. Available from: https://dx.plos.org/https://doi.org/10.1371/journal.pone.0242953.
Center for Disease Control. A Guide for Community Partners: Increasing COVID-19 Vaccine Uptake Among Members of Racial and Ethnic Minority Communities [Internet]. 2021 [cited 2022 Nov 28]. Available from: https://www.cdc.gov/vaccines/covid-19/downloads/guide-community-partners.pdf.
Chhibber A, Kharat A, Duong K, et al. Strategies to minimize inequity in COVID-19 vaccine access in the US: Implications for future vaccine rollouts. Lancet Reg Health - Am [Internet] 2022 [cited 2022 Nov 28];7:100138. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2667193X21001344.
Opel DJ, Lo B, Peek ME. Addressing Mistrust About COVID-19 Vaccines Among Patients of Color. Ann Intern Med [Internet] 2021 [cited 2022 Nov 28];174(5):698–700. Available from: https://www.acpjournals.org/doi/https://doi.org/10.7326/M21-0055.
Acknowledgements
This work was performed by the mAb Real World Evidence Collaborative. Author order is listed alphabetically by last name. The authors would like to acknowledge Mark McClellan, M.D. from the Duke-Margolis Center for Health Policy and Scott Fox, M.S., MITRE Corporation for their contributions to the research design of our study. The views expressed are solely those of the authors and do not necessarily represent those of the U.S. Department of Health and Human Services.
Funding
This study was supported wholly or in part with federal funds from the Administration for Strategic Preparedness and Response, Biomedical Advanced Research and Development Authority, under contract number 75FCMC18D0047 task order 75A50121F80012 awarded to The MITRE Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr Amin reported receiving grants from the University of California, Irvine, during the conduct of the study; grants from Alexion Pharmaceuticals, Blade Therapeutics, Eli Lilly and Company, Fulcrum Therapeutics, Humanigen, the National Institute of Allergy and Infectious Diseases, Novartis, NRx Pharmaceuticals, Octapharma, Pulmotect, PTC Therapeutics, and Takeda Pharmaceuticals; and personal fees from Achogen LaJolla, Alexion Pharmaceuticals, AseptiScope, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly and Company, Ferring Pharmaceuticals, Gilead Sciences, HeartRite, Millennium Pharmaceuticals, Mylan, Nabriva Therapeutics, Novartis, Paratek Pharmaceuticals, Pfizer, Portola Pharmaceuticals, Salix Pharmaceuticals, Seres Therapeutics, Spero Therapeutics, Sprightly Health, Sunovion Pharmaceuticals, and Tetraphase Pharmaceuticals outside the submitted work. Dr Bertagnolli reported receiving personal fees from The MITRE Corporation during the conduct of the study. Dr Chow reported receiving personal fees from Canon Medical Systems outside the submitted work. Dr Drews reported receiving grants from The MITRE Corporation during the conduct of the study and outside the submitted work. Dr Hanna reported receiving personal fees from Abpro Corporation and Merck & Co outside the submitted work. Dr Jones reported receiving personal fees from The MITRE Corporation during the conduct of the study. Dr Lopansri reported receiving personal fees from Seegene outside the submitted work. Dr O’Horo reported receiving grants from The MITRE Corporation during the conduct of the study; grants from nference; and personal fees from Bates College outside the submitted work. Dr Piantadosi reported receiving personal fees from The MITRE Corporation during the conduct of the study and outside the submitted work. Dr Pritt reported receiving funding from The MITRE Corporation during the conduct of the study. Dr Razonable reported receiving grants from Gilead Sciences, Regeneron Pharmaceuticals, and Roche and personal fees from Novartis outside the submitted work. Dr Webb reported receiving grants from Gilead Sciences and Regeneron Pharmaceuticals outside the submitted work. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shyam Rele, PhD, a former employee of The MITRE Corporation.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ambrose, N., Amin, A., Anderson, B. et al. The Influence of Social Determinants on Receiving Outpatient Treatment with Monoclonal Antibodies, Disease Risk, and Effectiveness for COVID-19. J GEN INTERN MED 38, 3472–3481 (2023). https://doi.org/10.1007/s11606-023-08324-y
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1007/s11606-023-08324-y